The Global Conference on Primary Health Care brought together 2050 delegates from 147 countries. Its aim was to commemorate the 40th anniversary of the Alma-Ata Declaration and renew political commitment to strengthening primary health care (PHC) as the foundation of universal health coverage (UHC) and essential to progress towards the Sustainable Development Goals. It explored the whole-of-government approach to advancing primary health care.
The Global Conference on Primary Health Care brought together 2050 delegates from 147 countries. Its aim was to commemorate the 40th anniversary of the Alma-Ata Declaration and renew political commitment to strengthening primary health care (PHC) as the foundation of universal health coverage (UHC) and essential to progress towards the Sustainable Development Goals. It explored the whole-of-government approach to advancing primary health care.
The Declaration of Astana was unanimously endorsed by Member States and made pledges in four key areas:
- make bold political choices for health across all sectors
- build sustainable primary health care
- empower individuals and communities
- align stakeholder support to national policies, strategies and plans
To transform these commitments into action, the WHO Regional Office for the Eastern Mediterranean launched the Primary Health Care Measurement and Improvement Initiative (PHCMI), supported by the Bill & Melinda Gates Foundation, UNICEF and the World Organization of Family Doctors (WONCA), in April 2019.
PHCMI is a joint initiative between the Regional Office’s Universal Health Coverage/Health Systems Department and Science, Information and Dissemination Department.
The objectives of PHCMI are to:
- develop a common language/framework through which to explain the process of PHC strengthening;
- identify and aggregate data that assess key aspects of PHC;
- create tools, such as PHC Country Profiles and Vital Signs profiles, that policy-makers, development partners and advocates can use to better assess and improve PHC services;
- highlight progress, and identify key challenges to improving PHC performance;
- develop PHC improvement plans and strategies as part of routine policy, planning, management, supervision and service delivery processes.
PHCMI is built on the global Primary Health Care Performance Initiative (PHCPI), the PHC operational framework, existing regional efforts to strengthen PHC services, PHC quality indicators and the WHO regional health system profile.
PHCMI aims to build national capacity to enable countries to undertake assessment-based improvements to PHC services and promote greater adoption of the people-based family practice approach to facilitate more equitable and efficient access to essential health services for individuals, especially the most vulnerable, residing in a catchment population of a primary health care facility.
The PHCMI initiative strives to, first, assess the current status of PHC services within countries and use that assessment to inform strategies to improve PHC. The assessment process comprises three phases: 1) Preparation; 2) Measurement and 3) Improvement.
In the Region, 20 countries have begun undertaking implementation of the assessment and completing the PHCMI country profiles.
Primary Health care Measurement and Improvement (PHCMI) Initiative





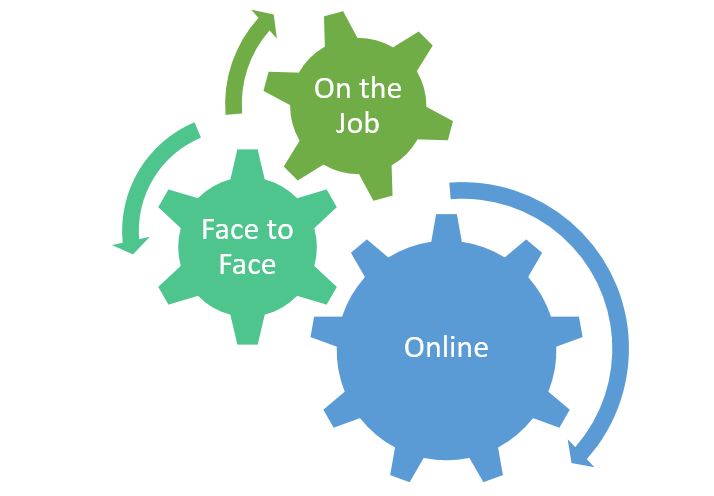
 31 March 2021 – On 16 March 2021, the WHO country office in Oman invited representatives Dr Badar Al-Alawi and Ms Mona Al-Battashi from the Oman Medical Specialty Board to discuss inititiation of a collaborative project related to online courses that had been agreed between WHO and the Board in February 2021.
31 March 2021 – On 16 March 2021, the WHO country office in Oman invited representatives Dr Badar Al-Alawi and Ms Mona Al-Battashi from the Oman Medical Specialty Board to discuss inititiation of a collaborative project related to online courses that had been agreed between WHO and the Board in February 2021.