

Addressing health emergencies

In 2019, 15 of the 22 countries and territories in the Region faced major emergencies, including three at the highest level, Grade 3. More than 70 million people needed humanitarian assistance, and the Region was both the source of more forcibly displaced people and host to a larger number of forcibly displaced people than anywhere else in the world.
WHO worked with a wide range of partners to respond to these emergencies, offering direct support to countries in the form of expertise and supplies, and helping partners deliver essential health services. We also worked with countries to help strengthen emergency preparedness and resilience, and to monitor and investigate potential disease outbreaks and other risks.
Responding to emergencies
Maintaining health systems and services

Emergencies increase the demand for health services while simultaneously disrupting and undermining the systems that deliver those services. WHO strove to maintain and expand health care provision across a wide range of technical areas, even in the most challenging circumstances.
Our noncommunicable diseases (NCD) kit provides a standard package of essential medicines and medical devices to meet the priority NCD health needs of 10 000 people for three months in emergency situations. In 2019, technical support was provided for its procurement and deployment in Afghanistan, Iraq, Libya, the Syrian Arab Republic and Yemen.
Mental health and psychosocial support were provided in countries affected by the Syrian crisis, Iraq, Libya and Yemen, in coordination and collaboration with our partner United Nations agencies, nongovernmental organizations, national stakeholders and academic institutions.
A framework for action for quality health care in extreme adversity was developed to support the implementation of evidence-based policies and strategies to ensure the delivery of quality and safe health care services in fragile, conflict-affected and vulnerable settings. It was pilot tested in Libya and Palestine during the year.
Meanwhile, as part of the recovery phase in Iraq and the Syrian Arab Republic, technical support was provided to strengthen technical capacities in procurement and distribution systems and the rational use of essential medicines, to support the transition from donations and supply systems managed by international organizations to national supply systems.
Improving surveillance and monitoring risks
Strengthening emergency preparedness

Extensive activities were undertaken to strengthen countries’ preparedness for emergencies. A joint external evaluation (JEE) was conducted in Iraq to assess the country’s public health capacities to deal with all hazards under the International Health Regulations (IHR 2005). This brings to 18 the number of countries in the Region that have undergone JEEs, with evaluations in the Islamic Republic of Iran, Palestine, the Syrian Arab Republic and Yemen set to complete the tally.
JEEs provide the basis for each country to develop a national action plan for health security (NAPHS) tailored to its specific needs. As part of follow-up work in 2019, workshops were organized by WHO and attended by representatives of public institutions and partner organizations, with participants teaming up across 19 technical areas of the IHR to address the recommendations that came out of previous JEEs. Djibouti, Egypt, Tunisia and the United Arab Emirates developed their NAPHS.
In addition to this support for individual countries, cross-border and regional preparedness were important areas of focus. WHO collaborated with country offices of the FAO and national ministries of public health, animal health and environment to conduct tripartite joint risk assessments for Afghanistan and Pakistan. Staff from national and subnational offices practised shared health threats at the human–animal–environment interface using a One Health approach.
As part of ongoing efforts to support countries in maintaining IHR core capacities at points of entry, WHO collaborated with the United States Centers for Disease Control and Prevention (CDC) and IOM to develop a new Handbook for public health capacity building and cross-border collaboration at ground crossings. This global resource was pilot tested through a comprehensive three-day programme of discussions in Beirut, Lebanon, with national IHR focal points, senior officials working directly with public health issues at ground crossings, participants from relevant sectors, and WHO’s sister United Nations agencies.
Further action on cross-border security included training for personnel from Bahrain, Saudi Arabia and United Arab Emirates on public health capacity-building and cross-border collaboration at ground crossings, and a review of ground crossings in Egypt to ensure preparedness following a Rift Valley fever outbreak in Sudan.
At the end of the year, the eighth regional stakeholders meeting brought together more than 140 participants from Member States to review the implementation of the IHR. The meeting provided a platform for the introduction of several new tools and innovations to support IHR implementation, including training packages and tools for NAPHS prioritization, monitoring and evaluation. Recommendations addressed enhancing multisectoral collaboration, determining priority areas, increasing capacity-building activities and continuing knowledge exchange between countries, with WHO reaffirming its commitment to provide ongoing technical support.
Key outcomes of the meeting will feed into the first health security diplomacy meeting, set to take place in 2020, which will provide a high- level forum for continuing multisectoral collaboration and coordination for IHR implementation.
Tackling infectious disease outbreaks
Despite major investment in recent years to strengthen preparedness and core capacities under the IHR, many countries in the Region remain vulnerable to infectious disease threats. Outbreaks of infectious diseases pose a particular risk to internally displaced persons, refugees and other vulnerable groups, and tend to have far-reaching social, economic and environmental impacts.
Epidemics of infectious diseases caused more than 2 million cases of illness and around 10 000 deaths in the Region in 2019. There were new emerging infectious disease outbreaks caused by high-threat pathogens as well as sporadic upsurges of endemic diseases.
WHO took proactive steps to reduce their impact by supporting the implementation of proven interventions focusing on strengthening national capacities to prepare for emergencies, detect public health events early on, monitor their progress to respond effectively and document impact, and undertake advanced research to fill the knowledge gaps related to emerging infectious diseases.
During the year, a total of 14 outbreaks of emerging infectious diseases with the potential for global spread were investigated and responded to through technical and financial support from the Regional Office. Eight countries reported diseases with outbreak potential, including chickenpox (varicella), chikungunya, cholera, Crimean-Congo haemorrhagic fever, dengue fever, diphtheria, extensively drug-resistant typhoid fever, hepatitis A, human immunodeficiency virus (HIV), measles, Middle Eastern respiratory syndrome coronavirus (MERS-COV), poliomyelitis and Rift Valley fever.
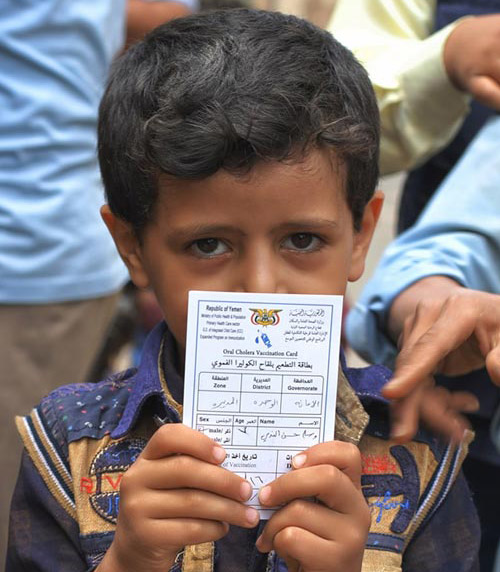
Cholera outbreaks continued to affect Somalia and Yemen for the third consecutive year. Yemen has been facing the worst cholera outbreak ever recorded, with more than 2.2 million people affected and nearly 4000 lives lost since 2016. In 2019, WHO provided substantial support to both Somalia and Yemen in implementing priority interventions to contain the outbreaks, including enhancing early warning surveillance and laboratory diagnosis, deploying rapid response teams, improving water and sanitation activities, mobilizing communities and implementing oral cholera vaccination campaigns.
We worked with Pakistan and Sudan to rapidly investigate and control one of the worst dengue fever outbreaks in recent years and implemented targeted vector control interventions to reduce vector
breeding sites, enhance entomological surveillance and improve health education campaigns targeting vulnerable populations.
Four countries – Oman, Qatar, Saudi Arabia and United Arab Emirates – faced cases of MERS during the year, reporting 223 laboratory-confirmed cases and 56 associated deaths in total. The number of hospital outbreaks decreased significantly during that time due to improved early warning surveillance and detection, as well as infection prevention and control practices.
Meanwhile, Sudan experienced multiple disease outbreaks, but a change in government policy led to all outbreaks being officially declared by the Federal Ministry of Health in line with IHR requirements and information being shared with WHO.
Enhancing EWARN
Strengthening pandemic preparedness

WHO continued to prioritize and support the development of national capacities to detect, prepare for, and respond to pandemic influenza. A major initiative in this regard was the fifth meeting of the Eastern Mediterranean Acute Respiratory Infection Surveillance (EMARIS) Network, held in conjunction with the Second Scientific Conference on Acute Respiratory Infection in the Eastern Mediterranean in Casablanca, Morocco, in November 2019.
Through the EMARIS network, countries in the Region work together to strengthen and enhance influenza surveillance, improve the use of surveillance data to strengthen disease control programmes and conduct research related to influenza and other respiratory viruses. This latest biennial meeting was organized in collaboration with the United States CDC and focused on the theme of “better data, better policy, better action”, aiming to promote quality data generation from local surveillance systems to enable evidence-informed public health policy-making.
Notable successes in the Region were discussed, including the expansion of the Pandemic Influenza Preparedness Framework, enhanced national rapid response capacities, an increase in the use of the PISA tool to estimate seasonal influenza severity, improved skills in advanced detection techniques, an increase in surveillance evaluations, a rise in the number of scientific publications and the finalization of pandemic preparedness plans.
Among other efforts to strengthen pandemic preparedness during the year, WHO provided extensive training to enhance influenza capacities, including a regional workshop on developing a protocol for the monitoring and evaluation of sentinel-based influenza surveillance systems, subregional training on influenza disease burden estimation and a meeting of directors of national influenza laboratories in the Region.
Polio – an ongoing threat
Stepping up the fight against wild poliovirus

As case numbers rose, the polio programme began systematically overhauling operations to address programme vulnerabilities and increase vaccine coverage. The governments of Afghanistan and Pakistan are committed to delivering a polio-free future for their populations, and implemented comprehensive programme reviews during 2019.
Challenges to eradication efforts include gaining access to all populations (which is affected by insecurity and partial bans on immunization in Afghanistan), quality of immunization campaigns in reservoir areas, population movement and concerns about the safety of frontline workers. Rising vaccine hesitancy, often related to misinformation spread over traditional or social media, has further complicated efforts to reach every child with polio vaccine. In response, WHO and partners are implanting transformative changes to turn the tide against the virus, including better programme management, a laser focus on entrenched polio reservoirs, measures to increase community engagement and working to overcome access barriers. The polio programme is also committed to collaborating with routine immunization programmes and forming new partnerships with broader health initiatives.
To support country efforts, the polio programme established the Global Polio Eradication Initiative (GPEI) Hub in Autumn 2019. The Hub, located in Amman, Jordan, is staffed by a dedicated team of experts with decades of experience fighting the poliovirus. They have been brought together specifically to support the Pakistan and Afghanistan teams as the countries overhaul operations and scrutinize areas of operational weakness. The Hub will provide better coordination across the GPEI partnership, enable more rapid deployment of surge support and technical expertise to Afghanistan and Pakistan, and ensure rapid decision-making closer to the ground.
Encouraging news came on 24 October 2019 when wild poliovirus type 3 (WPV3) was certified as globally eradicated by the Global Commission for the Certification of Poliomyelitis Eradication. This was a major achievement, meaning that out of the three wild polio serotypes, only one remains. For the Eastern Mediterranean Region, it was further proof that with investment in skilled workers, innovative tools, and routine immunization, it is possible to achieve a polio-free world.







