Annual report of the Regional Director 2013
Poliomyelitis eradication
Outbreaks of poliomyelitis occurred in the Syrian Arab Republic and Somalia. These were a serious blow to the progress of the global polio eradication programme and a threat to all countries. Indeed, the outbreak in Somalia, the result of importation from Nigeria, also affected neighbouring Kenya and Uganda. In response, the Regional Committee adopted a resolution on intensifying polio eradication efforts in the Region declaring the spread of wild poliovirus an emergency for all Member States of the Region and re-emphasizing the critical importance of stopping ongoing transmission of poliomyelitis in Pakistan and Afghanistan.
In line with the resolution, comprehensive strategic plans were developed in coordination with national governments and partners to control the outbreaks. Multi-country outbreak responses were reviewed and phase II response plans developed, based on the evolving epidemiology and lessons learned.
In Somalia and Syrian Arab Republic a number of strategies were deployed to raise immediate population immunity and control the outbreaks, including use of the bivalent vaccine, short interval additional dose, permanent posts for vaccination in border transit areas, low profile vaccination teams, prepositioning of vaccine and expanding the age group for vaccination. The strong working partnership among all the partners was important in addressing the emerging issues and evolving epidemiological developments. Coordination between the WHO regional offices for Africa and the Eastern Mediterranean also had a positive impact in controlling the outbreak. Preventive vaccination campaigns were conducted in countries at particular risk, including Egypt, Jordan, Iraq, Lebanon, Palestine and Yemen, with special focus on refugees, migrants and internally displaced persons.
With regard to the two countries where poliovirus circulation continues, significant progress was made in Afghanistan, where transmission is well controlled in the southern endemic part of the country. Only one case was reported from the endemic area of the southern region. Other cases reported were from the eastern region, and genetic sequencing demonstrated a strong link with polioviruses in Pakistan. The primary challenge remains the inability to maintain high oral poliovaccine (OPV) coverage in the eastern provinces, especially Kunar. In Pakistan the situation deteriorated, largely owing to conflict, continuing ban by militants on immunization, insecurity and the continued killing of the polio workers in the field. Polio continues primarily in the Federally Administered Tribal Areas (FATA) and the neighbouring province of Khyber Pakhtunkhwa; of 93 cases reported by Pakistan in 2013, 66 were from FATA. The 2014 military operation in North Waziristan Agency of FATA has resulted in huge population migration to the neighbouring districts of Pakistan and Afghanistan. The programme is continuously monitoring this movement and vaccinating at transit points, in camps and in the host community.
WHO provided additional human resources support to Afghanistan, Pakistan and Somalia, and to the Syrian Arab Republic and neighbouring countries. All national polio laboratories were accredited and rehabilitation services continued to be supported in Pakistan for children affected by polio. The Regional Director undertook advocacy missions to infected areas and a high-level Islamic Advisory Group was established. Cross-border coordination and interregional collaboration were strengthened, several emergency consultations were held to align partner support, and additional direct financial support was provided.
HIV, tuberculosis, malaria and tropical diseases
The number of people living with HIV (PLHIV) in the Region in 2013 is estimated at 280 000, of whom 17 000 are children. With an estimated 42 000 new HIV infections in 2013, the growth of the epidemic by far outpaces improvements made in terms of access to HIV prevention, diagnosis, care and treatment services. Coverage with antiretroviral therapy remains the lowest in the world, reaching almost 20% of those in need. This is attributed to an accumulation of gaps and weaknesses in the current HIV control strategies and programmes. The biggest gap lies in the ability to create and meet demand for HIV testing services, which is the primary gateway for access to treatment. In order to close these gaps political commitment, service delivery approaches and the health system all need to be strengthened, while persistent stigma and discrimination, including in health care settings, need to be addressed urgently.
In 2013, WHO launched the regional initiative to end the HIV treatment crisis, which aims at reaching universal coverage of 80% with antiretroviral therapy by 2020. Its immediate objective is to mobilize urgent action to accelerate access to treatment. For this purpose, WHO developed a guide and tools intended to assist countries in analysing gaps and lost opportunities along the continuum of prevention, testing, care and treatment in order to identify actions that may result in accelerating access. This is known as the HIV test–treat–retain cascade analysis, and, so far, five countries have carried out the analysis. WHO and UNAIDS developed a joint advocacy document which highlights the main reasons for low coverage of treatment in the Region and recommends key strategies and actions required to accelerate the scale-up of diagnosis and treatment.
WHO also developed consolidated antiretroviral therapy guidelines and 15 countries have updated, or are in the process of updating, their HIV treatment guidelines accordingly. Training modules were developed on basic HIV knowledge and stigma reduction for health workers and tested in two countries. WHO continued its support to countries and civil society organizations in collecting and analysing strategic information, developing national strategic plans and implementing effective evidence-based HIV prevention activities among key populations at increased risk of HIV.
During 2012[1], over 430 000 cases of all forms of tuberculosis were notified in the Region. Case detection for all forms of tuberculosis and for multidrug-resistant tuberculosis (MDR-TB) continues to pose a major challenge in the Region, and globally, as does the slow pace of decline in incidence. The regional case detection rate for all forms was 63% in 2012 (62% in 2011). Twelve countries achieved or exceeded the 70% target for case detection rate. The treatment success rate for new cases remained at 88% for the fifth consecutive year, and 13 countries reached or exceeded the global target of 85%. WHO support to countries focused on ensuring quality in tuberculosis care through technical support, monitoring of country programme implementation, in-depth review missions and capacity-building.
The situation with regard to MDR-TB is a major concern. Of 18 000 estimated cases, only around 2300 were detected in 2012. Of these 1602 cases were put on treatment; the treatment success rate for MDR-TB cases is around 56%. Adequate scale-up of MDR-TB control is prevented by the need to strengthen health systems and the allocation of financial resources specifically to address this growing problem. WHO worked with 10 countries to develop plans for ambulatory care based on the MDR-TB planning tool kit.
Eight countries in the Region reported local malaria transmission in 2013. In 2012, the total number of parasitologically confirmed malaria cases exceeded 1.3 million, which represents only 10% of the estimated cases in the Region. The reported number of deaths attributed to malaria was 2307, 84% of which were in South Sudan and Sudan (Table 1)[2]. The need to strengthen diagnosis and surveillance systems continues to be a major challenge in the high-burden countries, especially Pakistan, Somalia and Sudan. There were some improvements in Afghanistan and Yemen, in particular the expansion of the malaria information system. A malaria outbreak in Djibouti highlighted the urgent need to strengthen programme capacity and to strengthen epidemic preparedness, particularly regarding availability of diagnostics, antimalarial medicine and vector control commodities, as well as trained staff.
Table 1. Reported malaria cases in countries with high malaria burden
Table 1. Reported malaria cases in countries with high malaria burden
|
Country |
2011 |
2012 |
2013 |
|||
|
Total reported cases |
Total confirmed |
Total reported cases |
Total confirmed |
Total reported cases |
Total confirmed |
|
|
Afghanistan |
482748 |
77549 |
391365 |
54840 |
319742 |
46114 |
|
Djibouti |
232 |
NA |
25 |
25 |
1674 |
1674 |
|
Pakistan |
4065802 |
334589 |
4285449 |
290781 |
NA |
NA |
|
Somalia |
41167 |
3351 |
59709 |
18842 |
NA |
NA |
|
South Sudan |
795784 |
112024 |
1125039 |
225371 |
||
|
Sudan |
1246833 |
506806 |
1001571 |
526931 |
NA |
NA |
|
Yemen |
142147 |
90410 |
165678 |
109908 |
149451 |
102778 |
Two countries, Islamic Republic of Iran and Saudi Arabia, are successfully implementing a malaria elimination strategy, despite the challenges they face in the border areas with Pakistan and Yemen, respectively. Population movement from malaria-endemic to malaria-free countries is increasing, resulting in more imported malaria and raising the risk of reintroduction of local transmission or occurrence of limited outbreaks of local cases as reported in Oman and Tunisia (Table 2). With WHO support, six countries conducted joint in-depth programme reviews involving key stakeholders and partners.
Table 2. Parasitologically-confirmed cases in countries with no or sporadic transmission and countries with low malaria endemicity
Table 2. Parasitologically-confirmed cases in countries with no or sporadic transmission and countries with low malaria endemicity
|
Country |
2011 |
2012 |
2013 |
|||
|
Total reported cases |
Autochthonous |
Total reported cases |
Autochthonous |
Total reported cases |
Autochthonous |
|
|
Bahrain |
186 |
0 |
233 |
0 |
NA |
NA |
|
Egypt |
116 |
0 |
206 |
0 |
262 |
0 |
|
Iraq |
11 |
0 |
8 |
0 |
8 |
0 |
|
Islamic Republic of Iran |
3239 |
1710 |
1629 |
787 |
1387 |
NA |
|
Jordan |
58 |
0 |
117 |
0 |
56 |
0 |
|
Kuwait |
476 |
0 |
358 |
0 |
291 |
0 |
|
Lebanon |
83 |
NA |
115 |
0 |
133 |
0 |
|
Libya |
NA |
NA |
88 |
0 |
NA |
NA |
|
Morocco |
312 |
0 |
364 |
0 |
314 |
0 |
|
Palestine |
NA |
NA |
0 |
0 |
NA |
NA |
|
Oman |
1531 |
13 |
2051 |
22 |
NA |
NA |
|
Qatar |
673 |
0 |
708 |
0 |
728 |
0 |
|
Saudi Arabia |
2788 |
69 |
3406 |
82 |
2513 |
34 |
|
Syrian Arab Republic |
48 |
0 |
42 |
0 |
22 |
0 |
|
Tunisia |
67 |
0 |
70 |
0 |
68 |
4 |
|
United Arab Emirates |
5242 |
0 |
5165 |
0 |
4380 |
0 |
Access to anti-malarial treatment, insecticides and long-lasting insecticidal nets (LLINs) is improving in all endemic countries. Almost 11 million LLINs were distributed during 2011 and 2012 in endemic countries. In Afghanistan, the operational coverage in targeted high transmission districts is expected to be above 70% and in Pakistan, the operational coverage in targeted areas was 41% at the end of 2013. Access to malaria confirmation, whether by microscopy or rapid diagnostic test, continues to be a major challenge, although there is encouraging progress in Afghanistan and Yemen.
The WHO/GEF/UNEP project on sustainable alternatives to DDT for vector control proceeded with success in Islamic Republic of Iran, Morocco, Sudan and Yemen. National capacity for integrated vector management was strengthened in several countries
Remarkable successes were seen in the area of neglected tropical diseases. The number of cases of guineaworm disease in South Sudan decreased by 78% in 2013 (121 cases), compared to 2012, although three cases were identified in Sudan (South Darfur State) after almost 10 years without cases. Preliminary surveys suggest the reintroduction of the parasite from South Sudan. With regard to lymphatic filariasis, verification of the elimination of transmission was completed in Yemen and in 80% of the former affected areas of Egypt. It is still hoped to achieve similar success in Sudan. The largest schistosomiasis control programme currently operating worldwide entered its third year in Yemen with a record number of interventions in 2013 as approximately 40 million praziquantel tablets were distributed to about 13 million people. An impact evaluation assessment, conducted in selected sentinel districts, showed that infection levels have fallen by more than half since the beginning of the project. It is hoped the programme will continue to operate successfully and to achieve its goals, as well as to provide a case-study for other programmes in the Region, such as in Sudan, and beyond.
In the last quarter of 2013, data on leishmaniasis in the Region covering the past 15 years, together with interactive maps and graphs, were made available on the WHO Regional Health Observatory. Several countries developed national guidelines for leishmaniasis control and case management. In order to assess the impact of the WHO technical guidelines on leishmania, an impact assessment project was started in Morocco.
Immunization and vaccines
The main challenge for immunization programmes in 2013 was political instability and insecurity, which affected the implementation of mobile and outreach activities in Afghanistan, Pakistan and Yemen and seriously affected routine immunization in the Syrian Arab Republic. The need to strengthen managerial capacity and commitment to routine immunization in addition to competing priorities are a challenge in some countries. The availability of financial resources also needs to be assured for implementation of supplementary immunization activities for measles and tetanus, introduction of new vaccines in middle-income countries and co-financing in GAVI eligible countries, as well as activities related to improving vaccination coverage in countries with low performance.
Despite such challenges, achievement of the regional expected results for routine immunization stayed on track for the vast majority of the indicators in 2013. Fourteen countries in the Region have achieved the target of 90% routine DTP3 vaccination coverage andYemen is close to doing so.
Eleven countries achieved at least 95% coverage with MCV1 (first dose of measles-containing vaccine) at national level and in the majority of the districts, and 21 provided a routine second dose of MCV with variable levels of coverage. To boost population immunity, nationwide measles immunization campaigns targeting a wide age range were conducted in Iraq, Jordan, Lebanon, Morocco, Pakistan, Syrian Arab Republic and Sudan and child health days in Somalia. Measles case-based laboratory surveillance is implemented in all countries. Despite the current challenges in the Region, six countries have reported very low incidence of measles (<5 cases/million population), with three of these continuing to achieve zero incidence and close to verifying measles elimination. The crisis in the Syrian Arab Republic resulted in outbreaks of measles in Iraq, Lebanon and Syrian Arab Republic, as well as Jordan which had been free of measles for 3 years. In response, measles supplementary immunization activities were conducted with strong support from WHO and in close collaboration with several partners. In line with consolidating the efforts to achieve the measles elimination target, the third regional Vaccination Week focused on measles elimination under the theme “Stop measles now”.
Elimination of maternal and neonatal tetanus was documented in Iraq. Five countries have not yet achieved elimination (Afghanistan, Pakistan, Somalia, Sudan and Yemen) and Djibouti has still to document it.
Progress with regard to the introduction of new vaccines was substantial. Hib vaccine is now in use in 20 countries, pneumococcal vaccine in 14 countries and rotavirus vaccine in 8 countries. These figures exceeded the target for 2013. Hib vaccine was introduced in Somalia, pneumococcal vaccine in Afghanistan and Sudan, and rotavirus vaccine in Saudi Arabia. Libya introduced pneumococcal, rotavirus, HPV and meningococcal vaccine and Sudan successfully implemented the second phase of the meningococcal A conjugate vaccine campaign (reaching more than 95% coverage).
In order to maintain achievements, WHO extended substantial support to countries. Comprehensive immunization programme reviews, reviews of vaccines surveillance networks, and assessment of effective vaccine management were conducted in several countries. Substantial support was also provided to countries preparing to introduce new vaccines. Capacity was strengthened in countries in regard to data quality, surveillance of vaccine-preventable diseases, monitoring and evaluation, as well as laboratory surveillance for measles, bacterial meningitis, bacterial pneumonia and rotavirus. WHO continued to coordinate the external laboratory quality control system and accreditation of measles laboratories.
The implementation of vaccine regulation and production faces a number of challenges relating to the lack of human resources with appropriate skills, as well as a lack of financial resources. Regulatory capacity was strengthened in the five countries producing vaccines, especially in the area of vaccine pharmacovigilance, vaccine safety communication and vaccine licensing. In terms of post marketing surveillance, four countries – Islamic Republic of Iran, Morocco, Sudan and Tunisia – are currently contributing to the global vaccine safety initiative that was initiated in 2012.
Health security and regulations
The incidence of emerging and re-emerging infectious diseases poses a perennial threat to regional health security. Substantial support was provided by WHO to manage outbreaks of hepatitis E in South Sudan, hepatitis A in Jordan and northern Iraq, dengue fever in Pakistan, meningococcal meningitis in South Sudan, yellow fever in Sudan and Crimean-Congo haemorrhagic fever in Afghanistan and Pakistan. In addition, the Middle East respiratory syndrome coronavirus (MERS-CoV), the novel respiratory virus that emerged in 2012, continued to spread further geographically. Six countries in the Region have now reported laboratory-confirmed cases of MERS-CoV.
In 2013, WHO provided strategic and technical support for risk assessment, field investigation and detection of widespread outbreaks across many countries which resulted in limiting their spread and minimizing health impact. Field missions were conducted in Qatar, Saudi Arabia and Tunisia for control of the outbreaks caused by MERS-CoV. Outbreaks of hepatitis A were effectively contained in Jordan and northern Iraq by the national health authorities following implementation of public health measures recommended by WHO after joint field investigations. Epidemic readiness measures were scaled up in all countries affected by the Syrian crisis through establishment of early warning surveillance systems for disease outbreaks in Iraq, Jordan, Lebanon and Syrian Arab Republic, as well as strengthening of laboratory diagnostic capacities for epidemic detection.
In view of the persistent threat from MERS-CoV virus, the sentinel surveillance system for severe acute respiratory infections (SARI) was expanded in several countries with a view to sustaining the capacity to detect diagnose, and respond to outbreaks caused by any novel influenza or respiratory viruses. Public health vigilance for MERS-CoV was maintained throughout the year through enhancing surveillance and improving other regional public health preparedness measures. Technical meetings, consultations and training courses were organized while strategic guidance and advisories were produced collectively with other national health authorities to improve regional preparedness for this novel infection.
Owing to the lack of representative data, the burden and magnitude of the resistance patterns of pathogens to different micro-organisms remains poorly understood in the Region. In response to Regional Committee resolution EM/RC 60/R.1, a set of strategic directions was developed through a consultative process to translate WHO’s six policy package on antimicrobial resistance into a framework for action on containment of antimicrobial resistance. A strategic framework was developed for early detection, diagnosis and control of zoonotic diseases. Progress was made also in developing a strategic framework for prevention and control of cholera and other epidemic diarrhoeal diseases, and a strategic framework for prevention and control of acute respiratory infections with epidemic potential.
By June 2012, only one country (Islamic Republic of Iran) was ready for implementation of the International Health Regulations (2005); all other Member States obtained a 2 year extension for implementation to June 2014, except Somalia which was not able to meet the requirements. Despite progress in meeting the requirements (estimated at 70% across the Region by end 2013), particularly in surveillance, response, laboratory and zoonotic capacities, many remain a challenge. This is especially the case with regard to capacities to handle chemical, radiological and nuclear events and for points of entry and preparedness. This is due to the lack of supportive public health laws and other legal and administrative instruments; insufficient coordination among the different stakeholders at country level and with neighbouring countries; high turnover of qualified personnel; insufficient financial capacity to cover planned activities; and geopolitical instability in some States Parties. Fig. 2 shows the implementation level with regard to capacities across the Region by end 2013.
The emergence of MERS-CoV further highlighted the importance of the Regulations and that epidemic and pandemic threats are on the rise. WHO worked closely with States Parties to raise awareness about the Regulations and associated commitments and facilitated experience sharing between countries and with other WHO regions. Collaboration was strengthened with international organizations, United Nations agencies, nongovernmental organizations and WHO collaborating centres and networks of excellence to support countries to step up the implementation of the Regulations. Support for national authorities in their efforts to respond to outbreaks, including the MERS-CoV outbreak, was managed within the framework of the Regulations.
WHO continued to provide technical support to States Parties to review the status of implementation and to develop national plans to address the gaps in capacity requirements. It is expected that a considerable number of State Parties in the Region will request further extension to implement the requirements by June 2016.
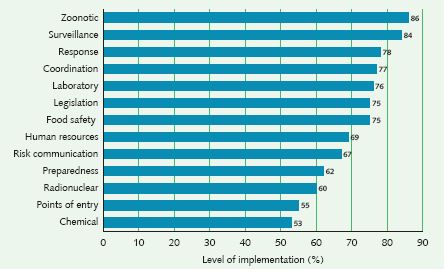
Figure 2: International Health Regulations (2005): level of core capacity implementation in the Eastern Mediterranean Region, 2013
Source: Summary of States Parties 2013 report on IHR core capacity implementation. Geneva: World Health Organization; 2014.
[1] For tuberculosis case detection, WHO receives data a year later, thus case detection data relate to 2012 and treatment outcome data to 2013.
[2] South Sudan became a Member of the African Region in May 2013.


