Research article
S.A.Mokhtar,1 A.A. El.Mahalli,2,3 S. Al-Mulla 4 and R. Al-Hussaini 4
دراسة العلاقة بين جودة الرعاية المقدمة للمرضى الداخليين وإعادة إدخال مرضى السكري مبكراً في أحد المستشفيات في المنطقة الشرقية من المملكة العربية السعودية
سميحة أحمد مختار، عزة علي المحلي، سلمى الملا، رنا الحسيني
الخلاصة: إعادة إدخال مرضى السكري بعد إخراجهم من المستشفى له قيمة محتملة على أنه مؤشر على جودة الرعاية. وتهدف هذه الدراسة الاستعادية للأتراب وللحالات والشواهد إلى تحديد معدَّل إعادة الإدخال إلى المستشفى لمرضى السكري خلال 28 يوماً بعد خروجهم منها، والعلاقة بين جودة الرعاية المقدَّمة للمرضى الداخليين وإعادة إدخالهم إلى المستشفى دون تخطيط سابق لذلك. أجرت الباحثات تدقيقاً للسجلات في أحد المستشفيات في المنطقة الشرقية للمملكة العربية السعودية خلال الفترة 2000-2008. فوجدن أن معدَّل إعادة إدخال المرضى إلى المستشفى دون تخطيط سابق لذلك، بعد إدخالهم للمستشفى لعلاج داء السكري %5.2(العدد 1125). وأظهرت مقارنة معطيات المرضى الذين أعيد إدخالهم المستشفى (العدد 62) وعيِّنة من المرضى الذين لم يعاد إدخالهم إلى المستشفى (العدد 62) أن التزام مقدِّمي الرعاية الصحية بالدلائل الإرشادية لجمعية السكري الأمريكية في إدخال المرضى (نسبة الأرجحية 0.91، فاصلة الثقة %95: 0.85-0.99) ومعايير التأهب لإخراج المرضى من المستشفى (نسبة الأرجحية 0.89، فاصلة الثقة %95: 0.84-0.95) كان من المرجَّح لها على نحو يُعْتَدُّ به إحصائياً أن تقلل من مخاطر إعادة إدخال المرضى إلى المستشفى مرة أخرى خلال 28 يوماً.
ABSTRACT Readmission of diabetic patients after discharge from hospital has potential value as a quality of care indicator. This retrospective cohort and case–control study aimed to determine the readmission rate for diabetic patients within 28 days after discharge and the association between quality of inpatient care and unplanned readmission. An audit of records was conducted in a hospital in the Eastern province of Saudi Arabia during 2000–2008. The rate of unplanned readmission of patients originally admitted with diabetes mellitus (n = 1125) was 5.2%. Comparison of data from readmitted patients (n = 62) and a sample of nonreadmitted patients (n = 62) showed that adherence by health care providers to American Diabetes Association guidelines for admission work-up (OR 0.91, 95% CI: 0.85–0.99) and readiness for discharge criteria (OR 0.89, 95% CI: 0.84–0.95) were significantly more likely to decrease the risk of readmission within 28 days.
Étude de la relation entre la qualité des soins en séjour hospitalier et une réadmission précoce des patients atteints de diabète dans un hôpital de la province est de l'Arabie saoudite
RÉSUMÉ La réadmission de patients diabétiques après leur sortie de l'hôpital peut être une information utile en tant qu'indicateur de la qualité des soins. La présente étude cas-témoin, de cohorte et rétrospective visait à déterminer le taux de réadmission des patients diabétiques dans les 28 jours suivant leur sortie de l'hôpital et la relation entre la qualité des soins en séjour hospitalier et une réadmission non programmée. Un examen des dossiers a été réalisé dans un hôpital de la province est de l'Arabie saoudite entre 2000 et 2008. Le taux des réadmissions non programmées de patients initialement admis pour un diabète (n = 1125) était de 5,2 %. La comparaison des données concernant les patients réadmis (n = 62) et un échantillon de patients n'ayant pas été réadmis (n = 62) a mis en exergue que l'application par les prestataires de soins de santé des directives de l'American Diabetes Association [Association américaine contre le diabète] concernant l'admission des patients (O.R. 0,91 ; IC à 95 % : 0,85–0,99) et les critères de sortie (O.R. 0,89 ; IC à 95 % : 0,84–0,95) permettait de réduire significativement le risque de réadmission dans les 28 jours.
1Department of Biostatistics, 2Department of Health Administration and Behavioural Sciences, High Institute of Public Health, University of Alexandria, Alexandria, Egypt (Correspondence to A.A. El.Mahalli:
3College of Applied Medical Science, University of Dammam, Dammam, Saudi Arabia.
4Health Information Management and Technology Programme, College of Applied Medical Sciences, King Faisal University, Dammam, Saudi Arabia.
Received: 30/05/10; accepted: 30/08/10
EMHJ, 2012, 18(5): 474-479
Introduction
Diabetes mellitus is fast emerging as one of the most serious health problems worldwide. In Saudi Arabia 4 million people are estimated to suffer from diabetes mellitus [1]. Good diabetes self-management is of critical importance in preventing serious long-term complications [2]. Diabetic patients may face problems in controlling or managing blood sugar levels. The most frequent problems are hyperglycaemia or hypoglycaemia. When patients face any of these conditions, they should be admitted immediately to hospital to receive proper care [3]. At the hospital, diabetic patients should receive multidisciplinary management in addition to regular follow up [4,5].
As diabetes is associated with many acute and chronic complications and comorbidities, diabetic patients are frequently readmitted to hospital [6,7]. Hospital readmission is a matter of concern due to its implications for the cost and utilization of hospital resources in addition to the burden on the patients and their families. In general, hospitalization consumes about half of health care expenditure. Hospital readmissions have considerable potential as an indicator of the quality of care [7–9]. In the United States, almost 18% of Medicare hospital admissions result in readmissions within 30 days of discharge, resulting in $15 billion in annual expenditures [8]. About $12 billion of that is spent on potentially preventable readmissions. The American Diabetes Association (ADA) has identified 3 major categories as standards of the quality of inpatient diabetes care: admission workup, evaluation of treatment during hospitalization and discharge criteria (readiness for discharge) [10].
Several studies have documented the relationship between hospital readmission and quality of care. Ashton et al. in the United States concluded that early readmission was significantly associated with the process of inpatient care and 55% of readmitted patients were more likely to have had a quality of care problem [7]. On the other hand, no studies have addressed the relationship between quality of diabetes care and early readmission in Saudi Arabia. Therefore the present study aimed to determine the 28-day readmission rate for diabetic patients at a hospital in the Eastern province of Saudi Arabia, to assess compliance of health care providers with the ADA guidelines and to identify factors predicting readmission.
Methods
Study design and sample
This was a retrospective cohort and case–control study. The target population was the medical records of diabetic patients admitted to a hospital in Al Khobar, Eastern province of Saudi Arabia between January 2000 and December 2008. This was a 340-bed teaching hospital affiliated to King Faisal University. Diabetic patients are referred to the hospital from a specific primary health care centre.
Ethical considerations
Formal approval from the Ministry of Health was taken before conducting the research. Confidentiality of the data collected from medical records was maintained.
Cohort study
To determine the 28-day readmission rate we examined the electronic and paper-based medical records of diabetic patients who were readmitted to the internal medicine department within 28 days of index hospitalization for the same diagnosis (unplanned readmission). The index hospitalization was defined as the initial hospitalization after which the patient was readmitted to the hospital within 28 days after discharge during the study period.
Case–control study
Sample
To determine the sample size for the case–control study, it was assumed that the odds ratio (OR) of readmission among diabetic patients exposed to substandard care was 2.24, and the fraction of early unplanned readmissions attributable to substandard of care was 14.9% [7]. With a relative precision of 50%, and 95% confidence level, the minimum required sample size was estimated as 62 cases and 62 controls [11].
The cases were all the diabetic patients (n = 62) readmitted within 28 days with the same diagnosis for unplanned reasons. The controls (n = 62) were selected using systemic random sampling after calculating the sampling interval from among the total number of diabetic patients not readmitted within 28 days after discharge. The exclusion criteria were: gestational diabetes, patients with planned readmission and patients readmitted due to reasons other than diabetes mellitus.
Data collection
Data were collected onto a proforma which was divided into 3 categories: demographic characteristics of the study sample (age, sex and marital status); hospital stay and disease history (date of admission and discharge, length of stay, number of hospital admissions within 2 years previous to the index admission and patient readmission within 28 days after discharge, comorbidities); and assessment of the degree of compliance of health care providers with ADA guidelines for inpatient diabetes care.
Items from the ADA guidelines were grouped into 3 categories: admission workup (history, physical examination and initial investigations); evaluation of treatment during stay; and readiness for discharge (discharge criteria). Each item in the ADA guidelines was given a score of 1 if it was achieved and 0 if not. The total adherence score for each category was expressed as the average percentage of achieved items over the total number of items for that category: 12 for admission workup, 12 for evaluation of treatment during hospital stay and 7 for discharge criteria.
Statistical analysis
Data entry and analysis were performed using SPSS, version 11.5 [12]. Patients’ demographic and clinical characteristics were examined in relation to the outcome (readmission). Statistical analysis was done using the Student t-test for continuous variables and the chi-squared test for qualitative variables. Means, standard deviations (SDs) and frequencies are presented. Multiple logistic regression analysis was used to estimate the unique effect of adherence scores on the probability of readmission after controlling for patients’ demographic factors, hospital stay information and disease history. Odds ratios (ORs) and confidence intervals (CIs) are presented.
The statistical significance was set at P < 0.05.
Results
Readmission rate
According to the electronic medical records of the diabetic patients discharged from the study hospital between January 2000 and December 2008, there were 62 patients readmitted within 28 days and 1125 patients not readmitted. The rate of unplanned readmission for diabetic patients was therefore 5.2% (95% CI: 1.1%–8.9%).
Comparison of readmitted (cases) and non-readmitted patients (controls)
The results showed that 84% of the 62 cases were readmitted once within 28 days, 11% were readmitted 2 times, 3% 3 times and 2% 4 times, with a mean number of readmissions of 1.2 (SD 0.6). In addition, 34% of the patients were readmitted 1 week after discharge, 19% within 2 weeks, 15% within 3 weeks and 32% within 4 weeks. The mean length of time between discharge and readmission was 14.4 (SD 9.5) days.
Table 1 shows that 66.1% of readmitted patients had type 2 diabetes and 33.9% had type 1; 95.2% suffered from diseases other than diabetes. For controls, the corresponding figures were 60.3%, 39.7% and 75.8% respectively. Concerning hospital admission, 85.5% of patients did not have any admissions in the previous 2 years and 12.9% had 1 previous admission. The mean duration of stay of the index admission was 12.9 (SD 25.1) days. For controls, 62.9% had no previous admissions and 27.4% had 1 admission. The mean duration of stay of the index admission was 13.0 (SD 17.9) days. No statistically significant difference was detected between cases and controls, except for the presence of comorbidity (P < 0.05).
Figure 1 illustrates that health care providers were compliant with the total list of admission workup guidelines for only 46.8% of the cases but 87.1% of controls. Concerning treatment during the hospital stay, providers were adherent for only 50.0% of the cases but 82.3% of controls. Regarding readiness of discharge, providers were conforming to guidelines for only 46.8% of the cases and 95.2% of controls. A statistically significant difference was detected regarding level of compliance of health care providers to the guidelines when caring for cases and controls in the admission workup (χ2 = 22.8, P < 0.05), treatment during hospital stay (χ2 = 14.4, P < 0.05) and readiness of discharge (χ2 = 35.2, P < 0.05).
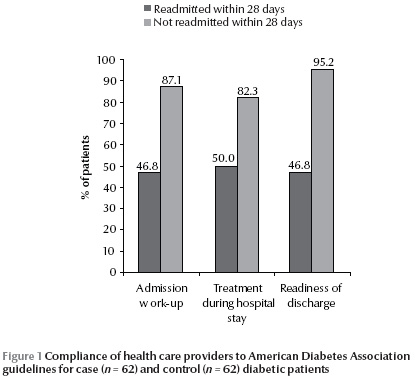
Table 2 shows that adherence of health care providers with most aspects of admission workup guidelines was lower for cases than for controls: diabetes history (74.2% and 98.4% respectively), comorbidity (75.8% and 95.2%), diabetes complications (82.3% and 93.5%), serum creatinine (59.7% and 69.4%), electrocardiography (EKG) (64.5% and 82.3%), urinalysis (74.2% and 100%), glycated haemoglobin (30.6% and 38.7%) and lipid profile (40.3% and 67.7%). For the control group health care providers had significantly better adherence with history taking (Fisher exact test, P < 0.001), documentation of comorbidity (Fisher exact test, P = 0.004), EKG analysis (χ2 = 4.9, P < 0.05), urine analysis (Fisher exact test, P < 0.001) and lipid profile (χ2 = 9.4, P < 0.05).
Table 3 shows that the compliance of health care providers with hospital stay treatment guidelines was lower for cases than controls in almost all aspects. A significant better adherence of health care providers to ADA guidelines was found for the control group in the following aspects: reporting alert of any danger signs/abnormal values to consultant physician (χ2 = 6.9, P < 0.05), consultation with expert physician (χ2 =14.5, P < 0.05), continuous insulin IV infusion (χ2 =23.2, P < 0.05), comprehensive nutrition assessment (χ2 = 12.9, P < 0.05), nutrition reassessment (χ2 = 18.3, P < 0.05) and education plan (χ2 = 37.4, P < 0.05).
Table 4 illustrates that the compliance of health care providers with all ADA guidelines of readiness for discharge was lower among the cases than the controls and the difference in compliance in all these aspects was statistically significant (P < 0.05).
Table 5 shows that the logistic regression model fit was satisfactory (χ2 = 78.2, P < 0.05). Factors in the model succeeded in explaining 76% of the variation in the probability of readmission. The model was able to predict the correct category for each case in 85% of occasions. Significant predictors were adherence of health care providers to admission workup and discharge criteria guidelines (OR 0.91, 95% CI: 0.85–0.99 and OR 0.89, 95% CI: 0.84–0.95 respectively).
Discussion
Diabetes is associated with many complications and comorbidities for which diabetic patients are frequently readmitted to hospital [6]. Complications of diabetes include damage to the nerves, blood vessels, heart, eye and kidneys. Diabetic neuropathy affects about 50% of diabetic patients. About 10%–20% of people with diabetes die of kidney failure and 50% die of cardiovascular diseases [13]. The present study showed that 5.2% of discharged diabetic patients were readmitted to hospital within 28 days. Ashton et al. revealed that 10% of diabetic patients in Veterans Affairs hospitals in the United States were readmitted within 14 days [7] and Robbin et al. found that 20% of diabetic patients in Philadelphia hospitals were readmitted within 30 days [6].
A literature review revealed that readmitted patients were more likely to have had a quality of care problem [7]. The present study showed that completeness of admission workup guidelines may decrease the likelihood of readmission (OR = 0.91, 95% CI: 0.85–0.99). The significant differences in admission criteria between cases and controls, however, were documentation of diabetic history and comorbidity, and performance of EKG, urinalysis, glycated haemoglobin and lipid profile tests. Moreover, adherence of health care providers to readiness for discharge criteria was more likely to reduce the probability of early readmission (OR 0.89, 95% CI: 0.84–0.95). All items of the discharge criteria including clinical stability, patients’ education and follow-up plan in the outpatient clinic were statistically significant. This was compatible with the results of another study which showed that the release of patients with diabetes or heart failure before meeting readiness for discharge criteria was associated with an increased probability of early readmission (OR 2.24, 95% CI: 1.11–4.49) [7]. On the other hand, other studies did not detect any association between quality of inpatient care and readmission [14].
Conclusions
Early readmission is common in patients with diabetes mellitus. Quality of inpatient care exerts a substantial influence on the risk of readmission. We therefore recommend that the study hospital should improve the quality of care delivered to diabetic patients especially with respect to health education for nutrition, insulin and drug regimen, dietary regimen, symptoms of uncontrolled diabetes and how to control complications. Special emphasis should be placed on attendance at outpatient clinics for follow up after discharge.
References
- Elhazmi M et al. Diabetes mellitus as a health problem in Saudi Arabia. Eastern Mediterranean Health Journal, 1998, 4:58–67.
- O’Reilly CA. Managing the care of patient with diabetes in the home care setting. Diabetes Spectrum, 2005, 18:162–166.
- American Diabetes Association. American Diabetes Association Position Statement. Standards of Medical Care in Diabetes, 2008, 3:S12–S46.
- Vrca-Botica M, Zelić I. Quality indicators for diabetes care in primary care. Diabetologia Croatica, 2007, 1:101–120.
- Inpatient diabetes certification. The Joint Commission [website] (http://www.jointcommission.org/cetificationprogram/Inpatient+Diabetes, accessed 19 January 2012).
- Robbin JM, Webb DA. Diagnosis of diabetes and preventing re-hospitalization: the urban diabetes study. Medical Care, 2006, 44:292–296.
- Ashton CM et al. The association between quality of inpatient care and early readmission. Annals of Internal Medicine, 1995, 122:415–421.
- Report to the Congress. Medicare payment policy. Washington DC, Medicare Payment Advisory Committee. (http://medpac.gov/documents/Mar10_EntireReport.pdf, accessed 21 March 2012).
- Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care. Archives of Internal Medicine, 2000, 160:1074–1080.
- Diabetes care. American Diabetes Association [website] (http://care.diabetesjournals.org/content/35/Supplement_1/S11.full?sid=d003310c-2d9b-4be2-8254-04092f81060e, accessed 24 March 2012).
- Lwanga SK. Lemeshows. Sample size determination in health studies: a practical manual. Geneva, World Health Organization, 1991.
- Pallent J. SPSS survival manual, 2nd ed. Milton Keynes, UK, Open University Press, 2004.
- Diabetes. World Health Organization [website] (http://www.who.int/mediacentre/factsheets/fs312/en/, accessed 21 March 2012).
- Luthi JC et al. Is readmission to hospital an indicator of poor process of care for patient with heart failure? Quality and Safety in Health Care, 2004, 13:46–51.


