Research article
A.M. Mohamed,1 M.S. Hassouna 2 and M.S. Kassem 3
الفروق بين الجنسين في العوامل التي تُمْلي القرارات التي يتَّخذها المرضى في شأن التماس المعالجة للسَّلَس البولي في الإسكندرية، مصر
عايدة محيي محمد، محمد السيد حسونة، محمد شريف قاسم
الخلاصـة: تهدف هذه الدراسة الوصفية الـمُقارِنة لمسح مستعرض لمرضى المستشفيات، إلى التعرف على الفروق بين الجنسين التي تُمْلي القرارات التي يتَّخذها المرضى في شأن التماس المعالجة للسَّلَس البولي. واستخدم الباحثون استبياناً عند مقابلة المرضى، وجمعوا المعطيات من 353 مريضاً راجعوا العيادات في مستشفيات الإسكندرية، في مصر. ووجدوا أن هناك فروقاً بين الرجال والنساء في ما يتعلق بالعوامل النفسية الاجتماعية النوعيَّة التي تدفَعهُم إلى التماس الرعاية الصحية. فقد كانت النساء أقل دخولاً إلى المستشفيات كما كان عدد أيام مُكْثهنّ فيها أقلّ، وقُلْ مثل ذلك في نسبة استخدامهنّ للإجراءات التشخيصية وللجراحة. وكان عدد النسوة اللائي يُعانين من واحد على الأقل من الآثار السلبية على حياتهن الاجتماعية أكثر من عدد أمثالهن من الرجال. ويبدو أن أثر الأعراض على جودة الحياة، يمثل الحافز الرئيسي لالتماس المساعدة لمعالجة السلس البولي لدى الرجال والنساء على السواء.
ABSTRACT The objective of this descriptive, hospital-based comparative cross-sectional survey was to determine gender differences in factors associated with patients’ decisions to seek treatment for urinary incontinence (UI). Using an interview questionnaire, data were collected from 353 patients attending clinics at hospitals in Alexandria, Egypt. There were differences between males and females regarding specific psychosocial factors motivating health care seeking behaviour. Women had fewer hospital admissions and hospital days and less use of diagnostic procedures and surgery. More women suffered from at least one negative impact on their social lives compared to men. The impact of symptoms on quality of life appeared to be the main trigger for seeking help for UI in both men and women.
Différences entre les sexes en matière de facteurs associés aux décisions des patients de se faire soigner pour l’incontinence urinaire à Alexandrie, Égypte
RÉSUMÉ L’objectif de cette étude transversale comparative et descriptive basée sur les hôpitaux était de déterminer les différentes entre les sexes en matière de facteurs associés aux décisions des patients de se faire soigner pour l’incontinence urinaire . À l’aide d’un questionnaire lors d’un entretien, les données ont été recueillies auprès de 353 patients consultant dans les centres de soins et les hôpitaux à Alexandrie (Égypte). Des différences entre les hommes et les femmes ont été constatées en ce qui concerne les facteurs psychosociaux spécifiques motivant leur décision de se faire soigner. Le nombre d’hospitalisations et la durée des séjours à l’hôpital étaient inférieurs chez les femmes, tout comme le recours aux procédures diagnostiques et à la chirurgie. Les femmes étaient plus nombreuses que les hommes à souffrir d’au moins une incidence négative sur leur vie sociale. L’incidence des symptômes sur la qualité de vie s’est avérée être le principal élément déclencheur dans la décision de se faire soigner pour l’incontinence urinaire chez les hommes et chez les femmes.
Received: 22/03/09; accepted: 30/04/09
EMHJ: 2010, 16(11): 1170-1182
Introduction
Urinary incontinence (UI) is the most common diagnosis made by urologists and gynaecologists [1], but only about 20% of individuals with UI seek medical care for treatment of their symptoms [2,3]. The prevalence of UI in community studies in Alexandria, Egypt was estimated to be 49.6% during the year 2006. Despite this high prevalence, UI is widely under-diagnosed and under-reported, and many Egyptian health care providers remain uneducated about it [4].
Numerous studies report that UI has a strong, if not devastating, impact on quality of life. Adverse effects include social isolation, loneliness and sadness, psychiatric illness including depression, embarrassment that affects the activities of daily living, stigmatization, effects on sexual relationships and disturbed sleep. Practical inconveniences associated with the leakage of urine include frequent changes of clothes and bed linen and the need to bathe more often [5]. Thus it is important to know the effect of UI on quality of life because it affects not only the patient’s ability and willingness to seek help but also the ability to benefit from treatment.
With such a condition it is not only important to know how common it is, but also for what reasons patients with incontinence actually seek treatment [6]. Severity of symptoms, psychological factors, comorbid conditions and reduced quality of life have all been implicated as factors that discriminate between those who seek medical care for UI and those that do not [7]. However, the associations between these factors and health care seeking by patients have not yielded consistent associations in previous studies.
There are gender difference in the aetiology, prevalence and management of UI in adults which vary by type of incontinence, its severity, the burden of illness and impact on the quality of social and sexual life, psychosocial factors related to health care use as well as sociodemographic characteristics [8]. As little is known about gender differences in health care seeking for UI it is useful to understand how males and females act in response to this medical condition, so that educational interventions can be most effectively targeted to raise knowledge, awareness and access to appropriate continence services. The objective of this study in Alexandria, Egypt was to determine gender differences in factors associated with patients’ decisions to seek treatment for UI.
Methods
This descriptive hospital-based comparative cross-sectional survey was carried out in the departments of urology and obstetrics and gynaecology of the Main University Hospital and El-Shatby University Hospital, Alexandria.
Sample
Data were collected from all UI patients seen at the outpatient clinic or inpatients wards during the recruitment period of the study (the first half of the year 2008). The inclusion criteria were: both sexes, over 18 years old, with clinically and urodynamically diagnosed UI, untreated at enrolment and willing to participate. The exclusion criteria were: invalidating neurological disease, urogenital cancer, mutilating surgery, psychiatric disease and/or advanced cognitive alteration. All patients who met the inclusion/exclusion criteria were enrolled by the investigators after obtaining informed consent.
Data collection
Data were collected using a pretested, precoded interview format. In-depth interviews were conducted by the investigators in a quiet place at the outpatient clinic or in the patient ward and lasted up to 1 hour. During the interviews, the following data were collected:
Participant’s characteristics: age, sex, level of education, residence, occupation, body mass index, presence of comorbid conditions.
UI symptom measures: symptom duration, frequency, amount of urine leakage, associated lower urological complaints, voiding pattern, degree of bothersomeness and activities leading to urine loss.
Type of incontinence: stress incontinence (leakage with cough, sneeze, exercise, activity), urge incontinence (leakage with the urgent desire to void), mixed incontinence (combination of stress and urge), overflow incontinence (leakage associated with over-distended bladder) or functional incontinence (leakage due to physical inability to get to the bathroom) [9].
Severity of incontinence: Sandvik’s severity index for UI was used to determine how often is urine leakage experienced and how much urine lost each time (total score range 0–8, with higher scores indicating more severe UI) [10].
Perceived causes of UI: 20 dichotomous questions were developed based on a literature review and scored on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree; total score range 0–100; α-reliability = 0.89); negative questions were reversed.
Psychosocial factors related to care seeking: An interview guide was developed based on a review of the literature and was grouped into 4 domains: satisfaction with aspects of the care received (5 questions; score range 0–5; α-reliability = 0.91); knowledge of UI and its treatment (5 questions; score range 0–5; α-reliability = 0.89), attitudes towards heath care use (7 statements; score range 0–35; α-reliability = 0.90) and gender perception (6 statements; score range 0–6; higher scores indicated stronger gender perception; α-reliability = 0.93). The UI self-efficacy questionnaire was used to assess participants’ self-efficacy (15 statements; score range 15–45; α-reliability = 0.90) [11].
Adverse impacts on social and sexual life. To assess impact on social life 9 questions were developed and grouped into 5 subscales: employment, social, family, economic and physical wellbeing (yes/no scores; extent of social suffering of patients with UI was the sum of “yes” replies across the 5 different social impacts). To assess impact on sexual life 3 questions were used: Is your sex life spoil by urinary symptoms? Is there any pain on sexual intercourse? Do you have leakage on intercourse? (yes/no scores).
Impact on quality of life: the King’s health questionnaire (KHQ) was used which has 21 items in 9 domains (total score range 28–115, with higher scores indicating greater influence of UI on quality of life) [12].
Ethics
Personal details of the professional background of the researchers were given to assure participants of the confidentiality of the research and help allay fears of talking about the personal and sensitive topic of UI. The research ethics committee of the University of Alexandria, Faculty of Medicine granted ethical approval.
Statistical analysis
SPSS 13.0 program was used for analysis. As the scores were not normally distributed, the chi-squared and Mann–Whitney tests were used to determine significant differences between the sexes. Median percentage scores were calculated as (total score/maximum possible score) × 100. We hypothesized that gender differences in treatment seeking for UI would not be explained only by sociodemographic factors, clinical presentation and symptom impact, but also some important psychosocial factors of the respondents as well. To test the hypothesis, we developed a multivariate logistic regression model for each sex. The factors included in the multivariate model were based on the association of a factor of treatment seeking with gender in bivariate analysis. An α-level of 0.05 was used to determine statistical significance.
Results
Background characteristics of the study subjects
Information was collected from 353 out of a total of 374 UI patients registered in the clinics and admission lists during the study period (94.4% response rate). Those who were not recruited included those who refused, were hard to communicate with or were not seen by the interviewers for different reasons.
There were 113 (32.0%) males and 240 (68.0%) females (male to female ratio 1: 2.12). Table 1 compares the sociodemographic characteristics of both sexes. The age of patients ranged from 23 to 85 years with a median age of 41.9 [interquartile range (IQR) 10.8] years. Most of the study males (55.8%) and females (61.3%) were in the age group 40–64 years. Significant differences between men and women were noted in occupation (P < 0.001), level of education (P < 0.001) and presence of comorbidities (P = 0.006). However, age distribution, marital status, residence and body mass index did not differ significantly by sex.
Clinical presentation of UI patients
Table 2 shows that about two-thirds of the study males (64.6%) and females (67.5%) reported at least weekly incontinence. No significant sex differences were noted in the frequency of urine leakage, symptom duration, voiding pattern or the degree of bothersomeness. However, a significant difference between males and females was noted in the amount of urine leakage and in the severity of incontinence. Severe incontinence was reported among 66.3% of females but only 34.6% of males. A significantly higher proportion of females (76.7%) reported associated lower urological complaints compared with 69.0% of males. The median activities score that lead to urine loss was significantly higher for females [23.2 (IQR 4.5)] than for males [15.5 (IQR 7.9)] (P = 0.032). Male and female patients also differed significantly in the type of UI. A higher proportion of males (55.8%) were diagnosed with either overflow, functional or total incontinence while in females mixed incontinence was the most common type encountered (56.7%).
Perception of underlying causes of UI
Table 3 shows that the median perception score of underlying causes of UI was significantly higher for females [76.4 (IQR 6.1] than for males [58.6 (IQR 10.3)] (P = 0.007). A significantly higher proportion of females suggested that UI is a normal part of being a female, being overweight or obese or due to using certain medications. On the other hand, higher proportions of males believed that large babies, neurological abnormalities, smoking, excessive caffeine consumption and drinking too many fluids caused UI.
Pattern of care seeking
Table 4 presents the pattern of care seeking. A significant difference was noted between males and females in the most important reason stated for help-seeking (P = 0.004). More males than females (30.9% versus 10.4%) stated that they sought medical care because of fear of a serious underlying disease such as cancer, whereas more females than males (42.5% versus 19.5%) sought medical help because of significant distress and impact on their quality of life. Previously seeking medical help was reported by significantly more females than males (P = 0.003). Fewer males (17.8%) than females (19.1%) cared for themselves by wearing adult incontinence pads or diapers.
The median period between the onset of symptoms and reporting to the health care facility was 30 days (range 2–1800 days). No significant difference was noted in days of delay in care seeking between males and females. A significantly higher proportion of females (84.6%) received health care at the outpatient clinic. However, males were hospitalized (28.3%) and used diagnostic procedures (43.4%) more frequently than women (15.4% and 16.7%). The median days of hospital stay for males was significantly longer than for females (6.8 days versus 3.3 days respectively).
A significant difference was noted between males and females as regards the recommended treatment options (P = 0.013). Medication was prescribed for most patients (70.8% of men and 85.4% of women) but surgery was recommended for a higher proportion of males than females (24.8% versus 13.3%).
Psychosocial factors affecting care seeking
Figure 1 summarizes the domains of the assessment of psychosocial factors related to care-seeking.
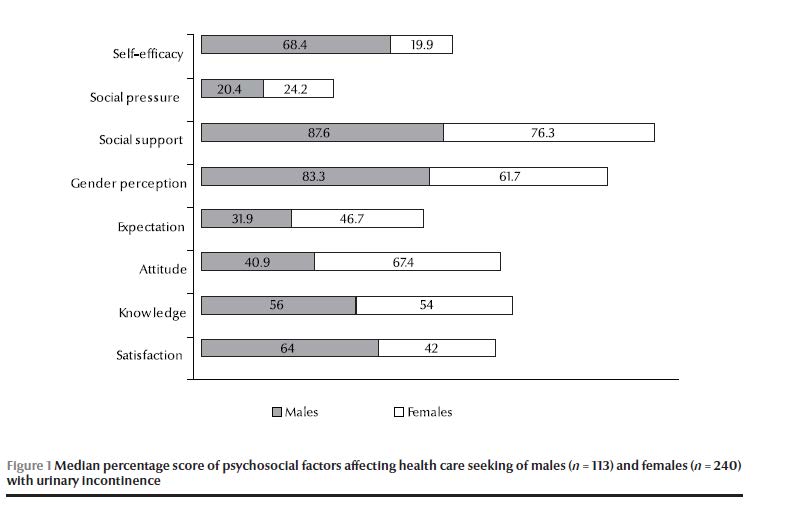
The median percentage score for satisfaction with care was significantly higher among men (64.0%) than women (42.0%) (P = 0.007). Higher proportions of males were satisfied with travel (time, distance and cost) (63.7%) and effectiveness of clinical care offered (73.5%) compared with females (42.1% and 49.6% respectively).
No significant difference was noted between males and females in the median score for knowledge related to UI, its complications and treatment (P = 0.353).
On the other hand, the median score for attitudes to care seeking was significantly higher among women (67.4%) than men (40.9%) (P < 0.001). Most patients believed that UI was not a stigmatizing disease (73.3% of females versus 54.9% of males). A significantly higher proportion of males than females (26.5% versus 9.8%) were not afraid of invasive investigations (P = 0.036). However, significantly more females than males reported no embarrassment about talking with others about urinary symptoms and fear of invasive investigations (54.2% versus 38.1%). Moreover, a significantly higher proportion of females (78.8%) intended to keep regular appointments for continued care compared with 51.3% of males. Expectations of benefit from treatment found among a significantly higher proportion of males than females (68.1% versus 53.3%, P = 0.027).
Figure 1 also shows that men and women had significant differences in gender perceptions of care seeking. A higher proportion of women than men believed that being a woman prevents them from discussing health problems (17.9% versus 2.4%) or seeking care respectively (9.2% versus 2.8%). A high proportion of women (71.3%) reported that they needed permission to obtain health care and had to be accompanied by someone (86.7%). Overall, the median gender perception score of males was significantly higher than females (83.3% versus 61.7%) (P < 0.001).
No sex differences were found in the effect of social support (P = 0.073) or social pressure (P = 0.325) on care seeking for UI (Figure 1).
The median percentage score for self-efficacy towards care seeking was significantly higher among men than women (68.4% versus 19.9%) (P < 0.001). A large proportion of men than women (53.1% versus 32.3%) were completely confident of holding their urine during strenuous exercise or when taking long-distance trips (51.3% versus 29.7%). Also a larger proportion of men (33.6%) than women (14.5%) were completely confident that they could prevent urine loss without relying on pads or protection when they were out.
Social and sexual impacts of UI
Table 5 shows that a significantly higher proportion of men than women (60.2% versus 13.3%) said that their employment opportunities were affected by their condition (P < 0.001). In the area of social life, the most frequently mentioned impact among women was “Having to take cumbersome precautions when going out” (76.3%). A composite indicator of social life problems showed that a significantly higher proportion of female respondents perceived a negative social impact compared with males (72.1% versus 48.8%) (P = 0.016) (Table 5). Overall, most women (76.3%) had experienced at least one of the itemized negative social impacts compared with 61.1% of men (P = 0.002).
In the areas of family life and financially no significant differences were noted between males and females in needing family help or increased daily expenditure. Similarly, men and women did not differ significantly in the 3 items listed in the category of physical problems. A composite indicator of physical problems showed that similar proportions of males and females perceived an impact of their condition (31.9% versus 27.1%).
Table 5 also shows no statistical significant differences between sexually active married men and women in the items addressing impact on sexual life.
Quality of life impact
The total median KHQ scores related to UI type were: for stress incontinence 42, for urge 54, for the mixed type 58, and other incontinence 41.
The total median KHQ score for women was significantly higher than that for men (67.1 versus 59.7 respectively, P = 0.002). A comparison of the median KHQ scores for women and men on the 9 subscales is shown in Table 6. Women had significantly higher scores than men on the following subscales: general health perception; UI impact; role limitations; social limitations; emotions; and sleep and energy. There were no statistical differences between the sexes on: physical limitations; personal relationships and activities performed. The most affected domain in women with regards to quality of life was “UI impact” while in men it was “activities performed”.
Determinants of incontinence care seeking
In Table 7, after adjustment for confounders, several factors were significantly associated with care seeking for UI. Women’s decision to seek treatment for UI was significantly positively associated with mixed type of incontinence, severe incontinence, perceptions about underlying causes of UI, better attitudes towards health care use, worse social impact score and worse disease-specific quality of life scores. Educations level (illiteracy) and self-care practices were determinants that adversely affected women’s care seeking. Age was not a determinant of treatment seeking. In men help seeking was related to the presence of comorbid conditions, severe UI, associated lower urological complaints, satisfaction with medical care offered, high expectation of benefit from treatment and worse disease-specific quality of life scores. These variables together explained 80.6% of the variability in care seeking behaviour (R2 = 80.6%).
Discussion
The health care needs of women cannot be explained solely in relation to reproductive function or other conditions that are unique to women. A variety of other diseases that are more prevalent in women or that manifest differently in women than in men also need attention [13]. The present study indicated that gender-based differences exist in factors associated with patients’ decisions to seek treatment for UI. These variations can support the clinical decision-making needed in addressing women’s and men’s health issues. By understanding behaviour more fully this research can help to identify ways in which an intervention may be effective in promoting treatment seeking for UI and patients may be assisted to access continence services.
Compared with men, women reported greater morbidity and seemed to be more likely to seek health care for UI, despite the fact that they were more affected by cultural and environmental factors that may work against them. Data from a World Health Organization collaborative study in 1991 revealed more frequent visits to doctors by women with UI in Tunisia than by men, a finding which may reflect women’s greater freedom of movement in Tunisia than in Egypt [14]. The same study showed women in general using more prescription medicines than men. However, in the case of less serious illnesses, women more frequently resorted to care and tended to over-report illness [15].
Gender differences in treatment seeking may vary with patients’ sociodemographic characteristics. The age of the studied men and women was not a significant contributing factor to treatment seeking. Nevertheless, many studies found that age was a significant predictor of treatment seeking for women and men with UI, perhaps because elderly patients have more frequent interactions with health care providers than younger patients due to the presence of comorbid conditions that require ongoing care [16,17]. However, the only social factor that determined health care seeking for UI in the present work was educational level; illiteracy adversely affected women’s care seeking independent of other factors.
Several diseases are associated with UI. Our study indicates that the presence of a comorbid condition was a predictive factor for medical care seeking for men but not for women. A possible explanation is that men had more severe incontinence-related morbidities even though comorbidities were more prevalent in women. A further study is needed to identify which comorbidities are more common in patients with UI compared with patients without the condition. These comorbid diseases could be used as a trigger for case-finding in general practice.
Seeking professional advice for a chronic health problem is not a clear-cut process. Individuals may have symptoms for a long time before seeking medical help. During this period, accommodation or adaptation to the symptoms occurs, with a gradual increase in the threshold for tolerance. It is only when this accommodation breaks down that people actually seek help [18]. Accordingly, women with UI in our study were more likely than men to use coping strategies such as incontinence pads. One possible explanation is that women may turn to coping strategies after finding that standard medical therapies fail (as indicated by the higher proportion of women who had previously sought medical help for UI). This finding is consistent with a recent cross-sectional survey of predominantly white US women aged 18 years and older, in which women with self-reported incontinence in the previous 30 days were more likely than men to be using pads or absorbents. This indicates that many women regard incontinence as more of a personal self-care or hygiene problem as opposed to a true medical condition [19]. However, by using incontinence pads without seeking assistance, they had closed themselves to the possibility of other treatments that may have enabled incontinence to play a less prominent part in their lives [20].
Severity of symptoms may be a driving factor that brings people to their physician because they are no longer able to cope with the symptoms. In the present study, severity of incontinence had a significant impact on the decision to seek treatment for both men and women. Moreover, incontinent women experienced significantly more associated urinary symptoms than men, which of course will add to their severity and distress. Symptom severity has been found to be associated with treatment seeking in other studies as well [21,22]. However, although severity is important, treatment seeking was not explained completely by severity. Seim et al. found that less than half of women with the highest severity of UI had sought treatment [23].
Adequate knowledge of the causes of UI can be a factor in help-seeking and successful outcome. Women’s median perception score for all stated causes of UI was significantly higher than for men, indicating a stronger perception of underlying causes of UI. However, interestingly, more women believed that UI was simply a normal part of being female. In the Gulf, using a questionnaire with close-ended questions, Saleha et al. found the more women than men perceived being overweight (51.9%) as the major cause of UI, followed by medication use (49.5%) [24]. These themes were also found in our participants’ responses, although at higher percentages. Women who believe that their UI is at least partly their responsibility (e.g. weight gain, medication use) may think they need to change the offending behaviour themselves. Women in this group may be more likely to consult a physician or other health care practitioner.
Health care providers can use our results to help counsel men and women with UI about modifiable risk factors, such as lifestyle, medications and to encourage treatment of those with non-modifiable histories, such as childbirth and prior surgery. All these perceptions should be taken into account when approaching the patient with UI, as individual belief systems will have an important impact on acceptance of the diagnosis and adherence to treatment [5].
Differences between males and females regarding specific psychosocial factors motivating health care seeking were found in the present study. The total score for patients’ knowledge did not differ by sex. However, the differences between men and women in help-seeking for UI may be heavily influenced by patients’ perceptions and attitude towards the illness and its treatment. Women’ positive attitudes towards health care use, having spoken to others about the problem and intention to keep regular appointments for continued care were significant predictive factors for care seeking among women. Moreover, stigma did not seem to prevent women from seeking care. Thus, incontinent people need to perceive the benefits of treatment in order to overcome the emotional costs of revealing their incontinence to a physician.
Males in the present study reported better overall scores in terms of gender perceptions; that is, they experienced culturally more favourable circumstances for seeking care when needed. Males were more satisfied with their care, while women tended to report longer waiting time at the incontinence outpatient clinic. We cannot assume that this was a result of gender bias by care providers; the finding could also be explained by women’s perceptions of time and the time pressure on them at leaving the house and the children. Meeting patients’ expectations may be the quickest way to achieve satisfaction with care, independent of health outcomes. Yet patient expectations may differ by sex. Therefore it is essential to identify gender-specific expectations of care seeking for UI if physicians are to provide satisfying incontinence care [25]. The present work indicated that a high expectation of benefit from treatment was a predictive factor for care seeking by incontinent men.
Interestingly, when we examined the most important reasons for raising the issue of incontinence with the physician, for men the most important reason was not related to the current impact of the condition but was concern that incontinence was a sign of a more serious condition. In contrast, significant distress and impact on their quality of life was the most commonly cited reason for women
Gender differences in utilization of hospital care services were noted in the present study. Women were significantly more likely to seek outpatient medical care and use medications than men. Inequality was observed in terms of less use of diagnostic procedures and surgery and fewer hospital admissions and hospital days among women. The present study cannot assume that this was a result of gender bias by care providers. However, family responsibilities and the financial and employment status of women in Egypt influence gender differences in utilization of hospital care resources. These findings have important implications for health care organizations that seek to provide equal care for both men and women.
Clinicians seeking to evaluate the impact of incontinence on patients’ lives should assess not only the clinical severity of symptoms but also the specific context in which symptoms occur. The findings revealed that women experienced greater patient-centred impact compared with men. More women suffered from at least one negative impact on their social lives compared with men. These experiences often lead to severe depression and a sense of despair, which, in turn, lead to self-neglect, reclusiveness, social withdrawal, poor self-image and low self-esteem [26]. A possible explanation is that incontinent men may adjust to the adverse impacts of UI over time using any means available to handle the symptoms.
An often overlooked consequence of UI is the potential interference with sexual life. The present study showed that while UI affected many sufferers’ sex lives there were no significant difference between the sexes in this regard. Additionally, the impact of UI on sexual life was not associated with seeking treatment for either men or women. The most likely explanation for this finding is that patients with UI were reluctant to raise questions regarding sexual function with their care providers. Qualitative research is needed to further characterize the relationship between UI and sexual function.
We examined the impact of UI on quality of life in the patients using a disease-specific questionnaire. The quality of life sub-dimensions showed that women had higher scores than men. The mixed type of incontinence had more impact on quality of life than that did stress incontinence. These results are consistent with previous findings [27–29]. Those with stress incontinence can probably adapt their lifestyle, e.g. by avoiding heavy lifting or exercising, and thus prevent situations that lead to involuntary loss of urine. Hagglund et al. studied a group of Swedish patients with UI and found that patients who sought treatment had higher quality of life scores [30]. Our study supports such observation. The impact of symptoms on quality of life appears to be the main trigger for seeking help for UI in both men and women.
Some limitations in the present work should be noted. The data on factors associated with help seeking and treatment patterns were collected by self-report and interviews were done by a health care worker at the hospital, which may lead to reporting bias for factors such as satisfaction with care. The design of the study was descriptive and our findings cannot show a cause and effect relationship between various factors and the decision to seek treatment.
Our results reveal a number of gender differences in the determinants of health care seeking for UI, and therefore strategies to enhance care seeking for UI should consider the role of gender in personal knowledge, needs and behaviours. Educating physicians and the public about the factors associated with treatment seeking as well as the available treatment options for UI management in adults may assist women and men to seek and receive more timely care for incontinence symptoms. The findings from this study provide important data for designing culturally competent UI care and health promotion programmes for medical practice.
References
- DuBeau, CE. Urinary incontinence. In: Evans JG, et al, eds. Oxford textbook of geriatric medicine, 2nd ed. Oxford, Oxford University Press, 2000:677–689.
- Shaw C et al. Barriers to help seeking in people with urinary symptoms. Family Practice, 2001, 18:48–52.
- Thomas TM et al. Prevalence of urinary incontinence. British Medical Journal, 2006, 481:1243–1245.
- Abed El-Fatah M. The prevalence and risk factors of UI in community-dwellings in Alexandria [MS thesis]. Department of Urology, Faculty of Medicine, Alexandria University, Alexandria, Egypt, 2006.
- Broome BA. The impact of urinary incontinence on self-efficacy and quality of life. Health and Quality of Life Outcomes, 2003, 1:35.
- Robinson D et al. Relationship between patient reports of urinary incontinence symptoms and quality of life measures. Obstetrics and Gynecology, 1998, 91:224–228.
- Gerwen MV, Schellevis F, Janssen TL. Comorbidities associated with urinary incontinence: a case-control study from the second Dutch national survey of general practice. Journal of the American Board of Family Medicine, 2007, 20(6):608–610.
- Li Y. Gender differences in health care seeking behavior for urinary incontinence and the impact of socioeconomic status: A study of the medicare managed care population. Neurourology and Urodynamics, 2004, 23(4):322–230.
- Teunissen D et al. ‘‘It can always happen’’: The impact of urinary incontinence on elderly men and women. Scandinavian Journal of Primary Health Care, 2006, 24:166–173.
- Hannestad YS et al. A community-based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of incontinence in the county of Nord-Trøndelag. Journal of Clinical Epidemiology, 2000, 53(11):1150–1317.
- Yusaf SO, Kavanagh DJ. Mechanisms of improvement in treatment for urinary incontinence: test of a self-efficacy and performance model. Journal of Cognitive Psychotherapy: An International Quarterly, 1999, 4:51–70.
- Donovan JL. Symptom and quality of life assessment. In: Abrams P et al., eds. Incontinence: 2nd International Consultation on Incontinence, Paris, July 1–3, 2001, 2nd ed., 2002:267–316.
- Gray ML. Gender, race, and culture in research on UI. American Journal of Nursing, 2003, 103(3 Suppl.):20–25.
- Andrews G. World Health Organization collaborative study on social and health aspects of ageing in Bahrain, Egypt, Jordan and Tunisia, 1991. ICPSR version. Alexandria, World Health Organization, 1998.
- Finklestein MM. Medical conditions, medications, and urinary incontinence. Canadian Family Physician, 2002, 48:420–428.
- Merkelij I. Urinary incontinence in the elderly. Southern Medical Journal, 2001, 94:952–257.
- Yue L et al. Gender differences in healthcare seeking behavior for urinary incontinence and the impact of socioeconomic status: a study of the Medicare managed care population. Medical Care, 2007, 5(11):1116–1122.
- Hovanitz CA, Kozora E. Life stress and clinically elevated MMPI scales: Gender differences in the moderating influence of coping. Journal of Clinical Psychology, 1999, 45:766–777.
- Melville JL et al. Fecal incontinence in US women: a population-based study. American Journal of Obstetrics and Gynecology, 2005, 193:2071–2076.
- Heit M et al. Adapting the theory of care seeking behavior to the clinical problem of urinary incontinence. Journal of Pelvic Medicine and Surgery, 2008, 14(1):29–35.
- Irwin D et al. symptom bother and health care seeking behavior among individuals with overactive bladder. European Urology, 2008, 53(5):1029–1039.
- Stach-Lempinen B et al. Visual analogue scale, urinary incontinence severity score and 15 D—psychometric testing of three different health-related quality-of-life instruments for urinary incontinent women. Scandinavian Journal of Urology and Nephrology, 2001, 35:476–483.
- Seim H et al. care seeking and treatment for urinary incontinence in a diverse population. Journal of Urology, 2008, 177:680–684.
- Saleh N et al. Prevalence, awareness and determinants of health care seeking behaviour for urinary incontinence in Qatari women: a neglected problem? Maturitas, 2005, 50:58–65.
- Heit M, Blackwell L, Kelly S. Measuring patient expectations for incontinence care seeking. Social Science & Medicine, 2003, 56:299–312.
- Lee KJ. The impact of urinary incontinence levels on the social lives of older Chinese in Hong Kong. Hallym International Journal of Aging, 2005, 7(1):63–80.
- Huang AJ et al. Quality-of-life impact and treatment of urinary incontinence in ethnically diverse older women. Archives of Internal Medicine, 2006, 166:2000–2006.
- Dugan E et al. The quality of life of older adults with urinary incontinence: Determining generic and condition-specific predictors. Quality of Life Research, 1998, 7:337–344.
- Shaw C. A review of the psychosocial predictors of help-seeking behaviour and impact on quality of life in people with urinary incontinence. Journal of Clinical Nursing, 2001, 10:15–24.
- Hägglund D et al. Quality of life and seeking help in women with urinary incontinence. Acta Obstetricia et Gynecologica Scandinavica, 2001, 80:1051–1055.


