 Dr Mahmoud Hariri, one of the lead trainers, guides participants through a practical session during the Hostile Environment Surgical Training. Photo: WHO28 November 2024 – For surgeons in the operating rooms of northwest Syria, where the hum of generators replaces the sterile quiet of modern hospitals, every decision is a race against time, every procedure a battle to save lives amidst conflict.
Dr Mahmoud Hariri, one of the lead trainers, guides participants through a practical session during the Hostile Environment Surgical Training. Photo: WHO28 November 2024 – For surgeons in the operating rooms of northwest Syria, where the hum of generators replaces the sterile quiet of modern hospitals, every decision is a race against time, every procedure a battle to save lives amidst conflict.
For doctors like Dr Abdullah Al-Saleh, a general surgeon at Al-Andalus Hospital in Idlib, the stakes could not be higher. “The hardest cases are the ones where every second counts,” he says. “We deal with severe abdominal and chest injuries, where even a small delay can mean losing a life. The reality is harsh. We do what we can with what we have.”
A surge in need amid escalating hostilities
After years of conflict, the health care system in northwest Syria is hanging by a thread. Hostilities, and the associated displacement and deteriorating living conditions, have led to a sharp rise in trauma cases, overwhelming already strained hospitals. The lack of resources and specialists often forces surgeons to step into roles outside their specialty. They must master multiple skills to meet the pressing demands.
Amid this mounting pressure, the Hostile Environment Surgical Training (HEST) programme is proving to be a lifeline. Developed to empower surgeons to manage complex emergencies, it combines technical expertise with real-world application.
“If you know how to hold a knife, you can do miracles”
 Participants at the HEST collaborate on a practical exercise, using anatomical models to refine critical surgical techniques for conflict and emergency settings. Photo: WHOFor Dr Mahmoud Hariri, one of the lead trainers, the training is not just about technical skills – it’s a culmination of lessons learned working in conflicts.
Participants at the HEST collaborate on a practical exercise, using anatomical models to refine critical surgical techniques for conflict and emergency settings. Photo: WHOFor Dr Mahmoud Hariri, one of the lead trainers, the training is not just about technical skills – it’s a culmination of lessons learned working in conflicts.
“There’s no room for strict specialization,” he says. “One day you’re a general surgeon, the next you’re managing vascular injuries or performing thoracic surgery. If you know how to hold a knife, you can do miracles.”
The training curriculum combines advanced techniques with innovative teaching tools tailored to conflicts. Participants work on lifelike simulators, practicing procedures like suturing a heart, stabilizing severe vascular injuries and performing tracheostomies under battlefield-like conditions. This hands-on approach ensures that surgeons are prepared to act decisively, even in the chaos of mass casualty events.
“These aren’t just theoretical skills,” says Dr Hariri. “When I performed 11 emergency heart sutures in Aleppo 13 years ago, 7 patients survived – a testament to the power of preparation.”
“Empowered to act in the moments that matter most”
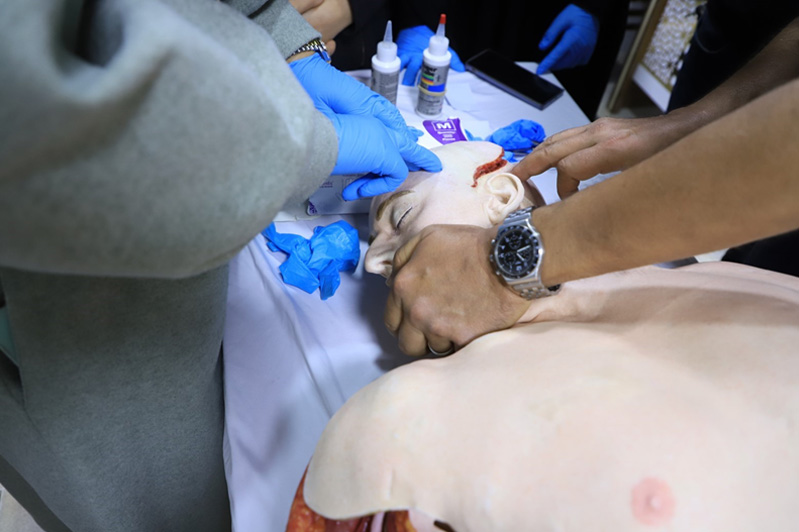 Participants practice wound management techniques on a medical mannequin during the Hostile Environment Surgical Training, focusing on real-life scenarios in conflict zones. Photo: WHOFor participants, the training is more than an opportunity to learn – it’s often the difference between life and death for their patients.
Participants practice wound management techniques on a medical mannequin during the Hostile Environment Surgical Training, focusing on real-life scenarios in conflict zones. Photo: WHOFor participants, the training is more than an opportunity to learn – it’s often the difference between life and death for their patients.
Take Dr Shahira Al-Hameed, an obstetrician and gynecologist at Jisr Hospital. Recently, she faced a complex case of uterine rupture and internal bleeding. “The patient’s abdomen was filled with blood, and it was nearly impossible to identify the anatomy,” she says. “The techniques I learned here helped me stabilize her. She left the hospital alive and healthy.”
Dr Shahira joined the HEST programme to prepare for emergencies that go beyond her specialty. “As a gynaecologist, I often encounter cases where I need to manage injuries to the intestines or bladder,” she says. “This training has given me the confidence to handle such situations until a specialist arrives.”
For Dr Alaa Barhoon, a general surgeon with over a decade of experience, the training introduced faster, more effective methods that fit the realities of northwest Syria. He highlights how techniques like vascular shunting – a method to restore blood flow when vessels are severely damaged – have become essential when traditional resources are unavailable.
“Time is everything,” he says. "The new methods we’re learning can save lives in ways that older approaches cannot."
Preparing for the unpredictable
HEST also emphasizes triage systems, a critical need in hospitals faced with mass casualties. “Triage planning can make or break a hospital’s response during emergencies,” says Dr Hariri. “In many hospitals here, the lack of proper triage leads to chaos. Through this training, we’re showing how even simple systems can save lives.”
Participants gain confidence through scenario-based learning. Simulations of battlefield trauma and mass casualty events help them practice the most complex procedures under harsh conditions.
The toll of working in such conditions is heavy. Dr Al-Saleh, a father of 3, says treating injured children is particularly harrowing. “It’s impossible not to imagine my own children in their place,” he says.
Dr Shahira echoes these sentiments. “The emotional strain is immense, but seeing a mother and child survive after a complicated delivery reminds me why I chose this path.”
Ready to save lives
 A trainer demonstrates advanced surgical procedures to participants during a hands-on session of the training. Photo: WHOAs the training concludes, its impact is already evident in the preparedness of its participants. “This isn’t just about surgery,” says Dr Hariri. “It’s about empowering doctors to face the worst and still deliver care.”
A trainer demonstrates advanced surgical procedures to participants during a hands-on session of the training. Photo: WHOAs the training concludes, its impact is already evident in the preparedness of its participants. “This isn’t just about surgery,” says Dr Hariri. “It’s about empowering doctors to face the worst and still deliver care.”
Beyond immediate skills, HEST focuses on long-term impact. Many participants, like Dr Ahmed Ghandour, have gone on to become trainers themselves. “I learned these techniques in 2019 and have since trained my entire surgical team in them,” says Dr Ghandour. “The ripple effect is profound – every surgeon we train can save hundreds of lives.”
The HEST training, delivered by expert trainers from the David Nott Foundation, was made possible through the support of USAID’s Bureau for Humanitarian Assistance (BHA) and implemented by the World Health Organization (WHO).


