Saving lives and protecting health: acceleration, innovation and impact
This album shows the work of the WHO country office in Somalia during 2020. The album documents the progress made by WHO in Somalia to improve health outcomes of the population of Somalia and highlights important achievements.
Photo credits: Ms Fouzia Bano, Communications Officer, WHO Somalia country office

Ensuring health for all for everyone everywhere: leaving no one behind
WHO has continued its work with the Government and other partners to improve primary health care (PHC) services to achieve universal health coverage (UHC).
At the request of the Federal Government, WHO started 2020 with a 3-level mission from 12 to 17 January 2020, with representatives from WHO headquarters, the Regional Office and the country office. Under the theme of PHC for UHC, the mission aimed to support the country in reviewing the current status of PHC in the country and identifying priorities and strategic directions to advance UHC. The recommendations of this mission led to the development of an Essential Package of Health Services (EPHS) by the Federal Ministry of Health, which was officially presented to the donors by the Government on 3 December 2020. The development of the EPHS, from conceptualization to content development, including prioritization of health services for different levels of health care, was supported by WHO.
WHO’s commitment to advance UHC in the context of a fragile health system and protracted crisis was reflected during the year through its organization of policy discourses, strategic engagement with partners and advocacy for building a stronger and resilient health system to achieve health for all.
During 2020, the country office also scaled up work in connection with the “Global Action Plan for Healthy Lives and Well-being for All”, especially in the PHC accelerator theme for which Somalia has been identified as a pilot country. As part of the work, the WHO country office participated in the PHC measurement initiative and also finalized a road map for bridging gaps in availability of, and access to, medical oxygen at health centres in the country.

Ensuring every child counts even during the pandemic: minimizing disruption to routine immunization
By offering life-saving vaccinations to children under the age of 1, routine immunization gives every Somali children a healthy start in life. This was severely challenged during the pandemic.
Despite the effect of COVID-19 on access to regular health services during the first half of 2020, WHO’s intensified support to the routine immunization programme helped essential health services for children to resume. In March and April, Somaliland and Puntland implemented an integrated campaign to support routine immunization coverage, which had been negatively affected by COVID-19. The integrated campaign administered measles vaccines, bivalent oral polio vaccine, vitamin A and deworming tablets to children. A similar campaign was conducted in Banadir in September. In total, 1 536 932 children received the bivalent oral polio vaccine, 1 416 950 children received measles doses, 1 395 699 children received vitamin A supplements and 1 194 948 children were given deworming tablets.
In 2020, 514 567 (83%) children aged under 1 received pentavalent 1 450 983 (73%) children received pentavalent 3 and 433 863 (70%) children received the first dose of measles vaccines. Despite this coverage, about 105 000 children did not receive the pentavalent 1 vaccine, 169 000 children did not complete 3 doses of pentavalent and 186 000 children aged under 1 missed their first measles dose. These missed cases are all attributed to the negative effect of the COVID-19 pandemic on routine immunization.
Enabling access to safe essential medicines: ensuring rational drug use at every health facility
In 2020, WHO supported the Somali Government to develop a national action plan on antimicrobial resistance. As a result, from October 2020 onwards, Somalia has been enrolled in the WHO Global Antimicrobial Resistance Surveillance System (GLASS), which supports global surveillance and research to strengthen the evidence on antimicrobial resistance. Promotion of the rational use of drugs continues as an important part of the work of the WHO country office. Work on antimicrobial resistance and Somalia’s enrolment in GLASS will generate further information on the country’s progress in improving the rational use of essential medicines in health centres.
WHO also supported the Federal Ministry of Health in conducting a survey of the pharmaceutical sector to determine access, availability, affordability, quality and rational use of medicines at the health-facility level. This survey was conducted in 65 health facilities – 30 public facilities, 30 private pharmacies and 5 public warehouses. The survey found that: 76% of public health centres, 83% of private pharmacies and 74% of public warehouses had key essential medicines available; 70% of public health centres and 87% of public warehouses had adequate stock records; and in 96% of public health centres, prescribed medicines were dispensed free of charge.

Ending tuberculosis: scaling up treatment and care in the midst of the pandemic
Despite disruption of the routine programme for universal access to treatment and care due to pandemic, WHO continued to support the Government to maintain essential TB services in such difficult and challenging settings. 17 139 TB cases were reported in 2020, of which 16 887 were drug-sensitive TB cases and 252 were drug-resistant TB cases. Case notification for drug-sensitive TB dropped by 0.5%, while that for drug-resistant TB dropped by nearly 24%, possibly as a result of COVID-19. Even though health service delivery for TB patients was severely strained, the cure rate for drug-resistant TB cases improved from 87% in 2018 to 92% in 2020.

Eliminating malaria: continuing control efforts despite disruption of services
Despite severe disruptions to services and control activities because of the COVID-19 epidemic, WHO continued its work to reduce malaria and improve vector control across the country with the goal of achieving malaria-free status.
In 2020, 341 341 suspected cases of malaria were tested, of which 27 526 were positive. All these cases were treated with artemisinin-based combination therapy. Compared with 2019, the number of malaria cases treated declined by 30% (39 341 cases of malaria were treated in 2019).
WHO also scaled up control efforts in high-risk areas for malaria control. To that end, 1 473 529 long-lasting insecticidal nets were distributed to 2 947 058 people in malaria-prone areas. WHO also supported indoor residual spray activities in flood-affected areas as a core intervention to reduce and control the risk of a surge in malaria cases. An estimated 269 685 people were protected by these control interventions.

Controlling neglected tropical diseases: keeping sight of elimination goals
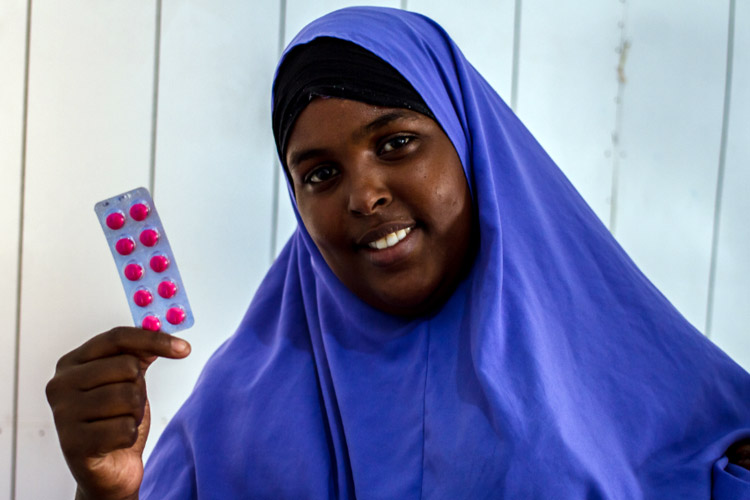
WHO maintained and worked to accelerate its efforts to control neglected tropical diseases in 2020, keeping sight of elimination goals for leprosy, schistosomiasis, soil-transmitted helminthiases and visceral leishmaniasis. With WHO’s support, a third round of mass drug adminstration for soil-transmitted helminthiases and schistosomiasis was conducted despite severe constraints on movement of people across the country and logistics challenges for drug administration. The mass drug adminstration covered 1 666 618 school-aged boys and 1 118 143 school-aged girls. A total of 5 099 986 tablets of praziquantel were distributed for schistosomiasis as well as 2 765 595 tablets of mebendazole to protect people from infections caused by worms.
Across the country in 2020, 2643 cases of leprosy were also detected and treated in owing to improved case detection and case findings.

Managing HIV/AIDS: sustaining universal access to health services
Despite the low prevalence of human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) in Somalia, WHO efforts continued to ensure universal access to prevention, treatment and care services.
By the end of December 2020, of the 10 409 people estimated to be living with HIV in Somalia, 3697 were receiving antiretroviral therapy, up from 3326 of 10 674 people living with HIV at the end of 2019. This increased the coverage of antiretroviral therapy for people living with HIV to 35.5% in 2020, up from 31.2% at the end of 2019. HIV testing for TB patients reached a coverage of 94.4% in 2020, and 81.6% of those found co-infected with TB and HIV were reported to have started antiretroviral therapy.

Eradicating polio: reaching every last child to stop transmission
Even though Somalia has been free of wild poliovirus since 2014, the country’s polio eradication programme detected outbreaks of circulating vaccine-derived poliovirus types 2 and 3 (cVDPV2 and cVDPV3) in late 2018. Since then, Somalia has continued to experience outbreaks of cVDPV2 every year; in 2020, 14 children were confirmed with cVDPV2 in the country. The pandemic challenged WHO’s continued efforts to stop and interrupt transmission of circulating vaccine-derived poliovirus in the country.
In 2020, 1 536 932 (90%) children were offered bivalent oral polio vaccines. During September and October 2020, outbreak response campaigns were conducted in the states to provide the monovalent oral polio vaccine. During each campaign, 94.6% and 96.0% of targeted children were covered, respectively. In December 2020, a nationwide campaign offering bivalent oral polio vaccine covered 97.1% of the targeted children.

Protecting the vulnerable: ensuring a continued response to health emergencies during the pandemic
Despite the pandemic, WHO managed and responded to other recurrent threats and risks to ensure that any outbreaks did not progress to become a major health concern.
In 2020, 6589 cholera cases and 33 deaths due to cholera were reported which was higher than 2019, and the cumulative attack rate was 183 cases per 100 000 populations. This increase may have been as a result of disruption of services for cholera control and elimination. Nonetheless, WHO’s support for improving case management and access to care resulted in the low case-fatality rate of 0.5% throughout the country.
As different types of emergencies occurred in the country, including armed violence, WHO continued to monitor the number of people injured or affected by such violence and responded accordingly.

Coordinating humanitarian health action during COVID-19: leading the response through the Health Cluster
Coordination is key to launching a robust and effective health response in any country. During the pandemic, the Health Cluster oversaw the regular coordination of more than 120 health partners in the country that jointly provided a strategic health response to the country’s humanitarian needs which were exacerbated during the pandemic. In 2020, 26 local and international Health Cluster partners provided 2.3 million outpatient consultations across the country, reaching 91% of the annual target. The highest proportion of consultations (17%) was in Banadir and 58% of the consultations across the country were provided to females.

Confronting COVID-19: accelerating the response
Somalia confirmed the first case of coronavirus disease (COVID-19) on 16 March 2020. By the end of 2020, the country had reported 4726 confirmed cases of COVID-19 (including 245 health care workers) with 130 associated deaths.
Since January 2020, WHO Somalia supported the country to prepare for and respond to COVID-19. This support included the establishment of incident management support teams to coordinate and enhance public health preparedness and response at national and subnational levels, covering a range of important areas such as surveillance and maintenance of essential health services.
In 2020, over 3300 community health workers were deployed by WHO to enhance detection and response activities at the community level. They detected 9048 alerts of COVID-19 through door-to-door visits. At the same time, 73 rapid response teams were deployed at the district level in 51 priority districts to investigate the alerts. Of all confirmed cases reported by the country, 42% were detected by these community health workers.
WHO equipped 694 health facilities with the Early Warning Alert and Response Network for early detection, investigation and response to COVID-19 and 14 other priority diseases. Testing capacity for COVID-19, which did not exist before the pandemic, was established in 24 laboratories across Somalia with the support of WHO. To offer care for COVID-19 patients, WHO supported the Government to establish 19 isolation centres, trained staff and provided salaries for staff and equipment and supplies. WHO trained 7189 health workers in surveillance, case management, infection prevention and control and risk communication in 2020.
Information on the trajectory of the COVID-19 epidemic was shared regularly with partners through weekly situation reports.


