Searching for gaps
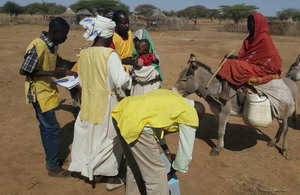
 WHO surveillance officers visit a village in a high-risk area to carry out an AFP case investigation. Photo: WHO Sudan8 February 2018 – As the world inches closer towards a polio-free future, finding and closing remaining gaps in national health system capacities to pick up traces of the virus is critical. Only three countries remain on the global endemic list – Afghanistan, Pakistan and Nigeria – but the threat of poliovirus resurgence remains very real, particularly for countries with a history of importation of poliovirus from these endemic areas.
WHO surveillance officers visit a village in a high-risk area to carry out an AFP case investigation. Photo: WHO Sudan8 February 2018 – As the world inches closer towards a polio-free future, finding and closing remaining gaps in national health system capacities to pick up traces of the virus is critical. Only three countries remain on the global endemic list – Afghanistan, Pakistan and Nigeria – but the threat of poliovirus resurgence remains very real, particularly for countries with a history of importation of poliovirus from these endemic areas.
In order to ensure that surveillance systems in these ‘at risk’ countries are up-to-scratch and sensitive enough to adequately detect and report cases of acute flaccid paralysis (AFP) – a major indicator for polio – World Health Organization (WHO) regularly leads expert reviews to put systems under the microscope.
Eighteen technical officers and polio surveillance experts from WHO, UNICEF, the US Centers for Disease Control and Prevention (CDC), the Bill & Melinda Gates Foundation and the Eastern Mediterranean Public Health Network (EMPHNET) recently met with Ministry of Health staff in Khartoum to share their findings and recommendations after scrutinizing Sudan’s surveillance performance at federal and state levels.
“Sudan has not seen a case of polio for almost nine years, however, certain factors put it at considerable risk of poliovirus importation and outbreaks,” said Dr Naeema Al Gasseer, WHO Representative to Sudan, engaged in review held 27 November ̶ 7 December. “It is very important that the country remains on guard against polio and continually analyses and improves the quality of its AFP surveillance, particularly in the high risk areas,” she said.
 Analysing the quality of AFP surveillance reporting at the field level. Photo: WHO Sudan“Strong AFP surveillance, in addition to maintaining high levels of routine immunization coverage, is a cornerstone of the polio eradication effort ̶ it enables us to quickly pick up poliovirus if it is circulating and react with an appropriate response,” said Dr Ni’ma Abid, a senior technical expert from WHO’s regional polio eradication hub in Amman, Jordan, presenting at the meeting. “There is no margin for error and in at-risk countries facing such challenges as Sudan, we need to thoroughly examine [AFP surveillance] systems to make they are sensitive and fast enough [to detect transmission]. This is a practice that will need to continue even after the world is certified polio-free,” he added.
Analysing the quality of AFP surveillance reporting at the field level. Photo: WHO Sudan“Strong AFP surveillance, in addition to maintaining high levels of routine immunization coverage, is a cornerstone of the polio eradication effort ̶ it enables us to quickly pick up poliovirus if it is circulating and react with an appropriate response,” said Dr Ni’ma Abid, a senior technical expert from WHO’s regional polio eradication hub in Amman, Jordan, presenting at the meeting. “There is no margin for error and in at-risk countries facing such challenges as Sudan, we need to thoroughly examine [AFP surveillance] systems to make they are sensitive and fast enough [to detect transmission]. This is a practice that will need to continue even after the world is certified polio-free,” he added.
Risk factors and special strategies
 Polio vaccination at a border crossing. Photo: WHO SudanSudan is the third largest country in Africa and home to over 40 million people. Insecurity, forced displacement, frequent nomadic population movement and inaccessibility in some areas make it challenging for health workers to consistently reach all children with vaccines to build immunity. Refugee influxes across porous borders with conflict-affected neighbouring countries exacerbate epidemiological risk and compound pressures on the country’s already stretched health system. In addition, high sub-Saharan temperatures and rough expansive terrain can make timely collection and transportation of stool specimens from children with AFP, for laboratory testing, difficult.
Polio vaccination at a border crossing. Photo: WHO SudanSudan is the third largest country in Africa and home to over 40 million people. Insecurity, forced displacement, frequent nomadic population movement and inaccessibility in some areas make it challenging for health workers to consistently reach all children with vaccines to build immunity. Refugee influxes across porous borders with conflict-affected neighbouring countries exacerbate epidemiological risk and compound pressures on the country’s already stretched health system. In addition, high sub-Saharan temperatures and rough expansive terrain can make timely collection and transportation of stool specimens from children with AFP, for laboratory testing, difficult.
To cater for specific surveillance challenges associated with reaching high risk groups, special strategies have been devised at state, locality and administrative unit levels. Examples include active searches for AFP cases and sample collection by community based surveillance officers in areas with access issues, the mapping of the movement of displaced populations, and establishing regular communication with nomadic community focal points who report AFP cases via mobile phone. In refugee camps, vaccination posts have provided an opportunity to screen for children with AFP, and collaboration and sensitization of non-government organization (NGO) staff has helped to improve reporting of AFP cases.
These and other strategies, including those targeting private and public physicians, and the quality of data from Sudan’s 688 health facilities reporting AFP came under review at the meeting.
Findings and the way forward
 International review team meets district surveillance team before embarking on field visits. Photo WHO Sudan.Eighteen states were assessed throughout the review, with visits to 90 health facilities, families of 16 children with AFP, and high-risk special populations conducted. Using standardized tools, teams assessed the quality of case investigation, active surveillance and surveillance documentation as well as plans for outbreak preparedness and response. Overall conclusions were that solid structures for AFP surveillance are in place in Sudan at all levels. The system is meeting global AFP surveillance targets and it is unlikely for polio to circulate undetected, however, there are gaps that need to be addressed.
International review team meets district surveillance team before embarking on field visits. Photo WHO Sudan.Eighteen states were assessed throughout the review, with visits to 90 health facilities, families of 16 children with AFP, and high-risk special populations conducted. Using standardized tools, teams assessed the quality of case investigation, active surveillance and surveillance documentation as well as plans for outbreak preparedness and response. Overall conclusions were that solid structures for AFP surveillance are in place in Sudan at all levels. The system is meeting global AFP surveillance targets and it is unlikely for polio to circulate undetected, however, there are gaps that need to be addressed.
“Surveillance system performance in Sudan is sensitive enough, and we were pleased to see implementation of the recommendations made at the last review,” said Dr Abid. “However, more attention needs to be paid to surveillance in refugee communities, cross-border population movement, and programmatic issues such as the high level of turnover of national surveillance staff,” he said. “We encourage the government of Sudan to implement the recommendations made at the review to address these and other gaps, as they will serve to further strengthen national and sub-national surveillance,” he said.
“WHO and partners commend the government of Sudan for its efforts to date, and stand ready to advise and support to keep the country polio-free,” said Dr Al Gasseer. “Until polio is gone for good, globally, we must make every endeavor to prevent resurgence,” she said.
Sudan witnessed its last case of indigenous wild poliovirus in 2001. Since then it has been exposed to several wild polio importations from Chad and Ethiopia with its most recent case in March 2009.


