Summary
The WHO Eastern Mediterranean Region is considered one of the WHO regions most vulnerable to the grave impacts of complex emergencies, especially given its high frequency of natural disasters, armed conflicts, political and economic instability, and population displacement. This has contributed to the increased incidence and prevalence of infectious diseases in the Region.
In 2022, a total of 61 infectious outbreaks, excluding coronavirus disease 2019 (COVID-19), were reported from 20 countries/territories in the Region – a remarkable increase on the 31 outbreaks reported from 11 countries in 2021. Major outbreaks in 2022 included acute watery diarrhoea (AWD)/suspected cholera, Crimean-Congo haemorrhagic fever (CCHF), dengue, malaria, measles, Middle East respiratory syndrome (MERS), mpox (monkeypox) and poliomyelitis (polio).
This report summarizes the epidemiological distribution of the major outbreaks in the affected countries based on person, place and time. The outbreaks data are presented on a periodic basis using the epidemiological curve of cases and deaths. Where there is available information, the geographical distribution of cases and deaths is also presented, using maps.
Further, the report also includes a summary of the WHO outbreak response in the affected countries/territories, challenges faced by WHO and partners in reaching the most vulnerable populations, and recommendations for prevention, control and management of infectious disease outbreaks in the Region.
Responding to emergencies and disease outbreaks is a difficult challenge that requires multisectoral and well-coordinated efforts from all stakeholders, especially in fragile, conflict-affected and vulnerable (FCV) settings. Data-sharing issues between health ministries and WHO country offices and between country offices and the WHO Regional Office for the Eastern Mediterranean continue to be a major obstacle to these efforts.
WHO thus recommends the development of a unified platform for data sharing from the health ministries to the country offices and from those offices to the Regional Office. Timely and streamlined information sharing is indispensable to strengthen both the efficiency and effectiveness of outbreak response and significantly improve coordination.
Introduction: outbreaks situation in the WHO Eastern Mediterranean Region in 2022
In 2022, the WHO Eastern Mediterranean Region witnessed a substantial increase in the number of emergencies and infectious disease outbreaks due to multiple hazards. These included natural and climate change-associated disasters such as severe droughts, floods and earthquakes, in addition to human-made disasters such as conflicts and political unrest. The emergencies and outbreaks resulted in mass population displacements and, ultimately, limited access to basic needs such as shelter, food and safe drinking water.
A total of 61 outbreaks, excluding coronavirus disease 2019 (COVID-19), were reported in 2022 from 20 countries/territories in the Region – a rise on the 31 outbreaks reported from 11countries in 2021.
The world is facing an upsurge in acute watery diarrhoea (AWD)/suspected cholera outbreaks, with a significant increase in the number of countries and populations affected, starting from mid-2021. Globally, 23 countries reported cholera outbreaks in 2021, while this number increased to 30 in 2022.
In 2022, AWD/suspected cholera outbreaks were reported from 8 countries of the Eastern Mediterranean Region: Afghanistan (suspected cases: 242 562; deaths: 87), Islamic Republic of Iran (confirmed cases: 367; deaths: 7), Iraq (suspected cases: 11 097; deaths: 24), Lebanon (suspected cases: 5422; deaths: 23), Pakistan (confirmed cases: 1002; deaths: 43), Somalia (suspected cases: 15 653; deaths: 88), Syria (suspected cases: 70 220; deaths 102) and Yemen (suspected cases: 21 178; deaths 21).
The recent cholera outbreaks in Lebanon and Syria are alarming as these 2 countries are not cholera-endemic and last experienced cholera outbreak 9 years and 20 years ago respectively. The current cholera outbreaks in the Region are disproportionately affecting children aged under 5 years: more than half of suspected cholera cases in Afghanistan (55%) and Somalia (65%) were children aged under 5 years. Meanwhile, children aged under 5 years accounted for about 26% and 24% of the suspected cholera cases in Lebanon and Yemen respectively.
The ongoing COVID-19 outbreak continued to be reported from all 22 countries and territories of the Eastern Mediterranean Region. By 31 December 2022, the global cumulative incidence of COVID-19 since the start of the pandemic had reached 651 922 986 confirmed cases, including 6 669 794 associated deaths, giving a case fatality ratio (CFR) of 1.02%. By the close of 2022, the Eastern Mediterranean Region had reported a total of 23 221 923 confirmed cases of COVID-19 – representing about 3.56% of the global magnitude – including 349 081 associated deaths (CFR: 1.5%).
In 2022, a total of 1759 suspected cases of Crimean-Congo haemorrhagic fever (CCHF), including 129 associated deaths (CFR: 7.40%), were reported from 2 countries of the Region: Afghanistan (suspected cases: 389; deaths: 15) and Iraq (suspected cases: 1370; deaths: 114).
A total of 100 432 dengue cases, including 164 associated deaths (CFR: 0.16%), were reported in 2022 from 6 countries of the Region: Afghanistan (suspected cases: 1266; deaths: 2), Oman (suspected cases: 579; deaths: 0), Pakistan (confirmed cases: 62 995; deaths: 62), Somalia (suspected cases: 5350; deaths: 18), Sudan (suspected cases: 5264; deaths: 37) and Yemen (suspected cases 24 978; deaths: 45).
In 2022, a total of 3 606 981 suspected cases of malaria, including 262 associated deaths (CFR: 0.01%), were reported from 4 of the Region’s countries: Djibouti (confirmed cases: 40 648; deaths: 0), Islamic Republic of Iran (confirmed cases: 4425; deaths: 0), Pakistan (suspected cases: 937 906; deaths: 0) and Sudan (suspected cases: 2 624 002; deaths: 262).
Globally, the number of suspected measles cases and the number of affected countries also significantly increased in 2022. There was a 79% year-on-year increase in the number of measles cases globally in the first 2 months of 2022, with children aged under 5 years the most affected age group.
In the Eastern Mediterranean Region, a total of 143 735 suspected measles cases, including 588 associated deaths (CFR: 0.41%), were reported from 8 countries: Afghanistan (suspected cases: 77 210; deaths: 388), Djibouti (suspected cases: 209; deaths: 0), Islamic Republic of Iran (suspected cases: 10 620; deaths: 0), Pakistan (suspected cases: 17 737; deaths: 117), Somalia (suspected cases: 17 361; deaths: 0), Sudan (suspected cases: 3310; deaths: 4), Syria (suspected cases: 6309; deaths: 2) and Yemen (suspected cases: 10 979; deaths: 77). This acute increase in the number of measles outbreaks in the Region is alarming and indicates an urgent need to strengthen routine immunization programmes in the affected countries.
Further, in 2022, a total of 9 cases of Middle East respiratory syndrome (MERS), including a single associated death (CFR: 11.11%), were reported from 3 of the Region’s countries: Oman (confirmed cases: 2; deaths: 1), Qatar (confirmed cases: 2; deaths: 0) and Saudi Arabia (confirmed cases: 5; deaths: 0). During the period April 2012 to December 2022, a total of 2603 laboratory-confirmed MERS cases were reported globally, including 935 associated deaths (CFR: 36%). Saudi Arabia accounted for most of the confirmed cases (2194) and deaths (854) reported (CFR: 39%).
Globally in 2022, 110 countries cumulatively reported 84 000 confirmed cases of mpox (monkeypox), including 80 associated deaths (CFR: 0.10%). Most of the cases were reported by the United States of America (29 000), followed by Brazil (10 680), Spain (7514), France (4114), Colombia (4000), United Kingdom of Great Britain and Northern Ireland (3735), Peru (3711), Mexico (3696), Germany (3684) and Canada (1460).
In the Eastern Mediterranean Region, 10 countries reported 80 confirmed mpox cases, including a single associated death (CFR: 1.25%), which occurred in Sudan. Most cases were in Lebanon (24 cases), followed by Sudan (18), United Arab Emirates (16), Saudi Arabia (8), Qatar (5), Morocco (3), Egypt (3), Bahrain (1), Islamic Republic of Iran (1) and Jordan (1).
Additionally, a total of 22 confirmed cases of wild poliovirus type 1, including zero associated deaths, were reported from Afghanistan (2) and Pakistan (20) in 2022. This indicates a significant year-on-year increase in the number of wild poliovirus type 1 cases, as only 5 cases were reported from Afghanistan (4) and Pakistan (1) in 2021, again with zero associated deaths.
Three countries reported a total of 164 cases of circulating vaccine-derived poliovirus type 2 (cVDPV2) during 2022: Somalia (), Sudan (1) and Yemen (159). This also indicates an increase compared with 2021, when 118 cVDPV2 cases were reported from 4 countries: Afghanistan (43), Pakistan (8), Somalia (1) and Yemen (66). No cases of circulating vaccine-derived poliovirus type 1 (cVDPV1) were reported in the Region in 2022; just 3 cVDPV1 cases were reported from Yemen in 2021.
Outbreaks response in 2022
Throughout 2022, the WHO Regional Office for the Eastern Mediterranean continually supported the health ministries in the affected countries/territories with the prevention, control and management of the outbreaks and worked closely with the health authorities and partners to reduce morbidities and mortalities resulting from these outbreaks.
The Infectious Hazard Prevention and Preparedness (IHP) unit of the Regional Office supported the affected countries/territories to develop and implement outbreak preparedness and response plans and improve coordination for all outbreak response pillars :
coordination and leadership
surveillance and outbreak detection
laboratory confirmation and diagnostics
case management
water, sanitation and hygiene (WASH)
risk communication and community engagement (RCCE).
WHO supported the establishment/enhancement of molecular diagnostic laboratory capacity in the Eastern Mediterranean Region, and trained laboratory technicians on standard and updated sample collection, transportation, and testing techniques. WHO also supported oral cholera vaccine (OCV) campaigns in 2022 in 5 countries of the Region: Lebanon (55% coverage), Pakistan (96% coverage), Somalia (95% coverage), Syria (93% coverage) and Yemen (88% coverage). Cumulatively, more than 8.3 million people (95.4% coverage ) aged 1 year and over were vaccinated against cholera in these countries in 2022.
In addition, the countries and territories of the Region conducted regular COVID-19 tests, and vaccination against COVID-19 continued in 2022 with WHO support. By 31 December 2022, a total of 442 303 054 laboratory tests had been conducted across the Region since the start of the COVID-19 outbreak. The highest number of polymerase chain reaction (PCR) tests were reported from the United Arab Emirates (197 950 426), followed by the Islamic Republic of Iran (54 738 231) and Saudi Arabia (44 940 564).
In total, 844 957 683 doses of COVID-19 vaccine had been administered across the Region’s 22 countries and territories by the end of 2022. Pakistan administered the highest number of doses (317 080 887), followed by the Islamic Republic of Iran (154 773 070) and Egypt (100 993 230). At the other end of the scale, the smallest number of doses of COVID-19 vaccine in the Region were administered by Djibouti (338 051), followed by Yemen (1 238 962) and Bahrain (3 476 633).
WHO provided diagnostic and case management kits in their tonnes to the health ministries in the affected countries and territories.
WHO also worked closely during 2022 with the United Nations Children’s Fund (UNICEF) and other partners to improve the WASH situation in the outbreak-affected countries.
Challenges
Responding to emergencies and disease outbreaks – especially in fragile, conflict-affected and vulnerable (FCV) countries – is a challenging task and requires multisectoral and coordinated efforts from all stakeholders. While addressing emergencies and responding to the outbreaks, WHO and partners faced multiple challenges, including fragile health systems in some countries and lack of access to affected areas owing to insecurity.
Most of the time, these bottlenecks caused delays to the planned activities, including outbreak response, increasing the risk of high-threat pathogens spreading to non-endemic areas. Among the main challenges faced in 2022 were multiple outbreaks in countries already affected by acute and protracted emergencies and with fragile and disrupted health systems, such as Somalia, Sudan, Syria and Yemen.
Prolonged insecurity in some countries – such as Iraq, Somalia, Syria and Yemen – meant that most areas of the country affected by the outbreak/emergency were inaccessible or hard to reach. Multiple natural disasters (floods in Pakistan, drought and floods in Somalia, and earthquake and floods in Afghanistan), conflict, political instabilities and population displacement also increased the spread of diseases. Further, these factors also jeopardized public awareness and the implementation of preventive measures against common infectious diseases (cholera, and vector-borne diseases), resulting in the spread of the infectious disease outbreaks. Underfinanced health systems, and those with inadequate capacity (Afghanistan and Pakistan) made the outbreak response even more challenging.
Responding to the huge number of outbreaks and emergencies requires more financial, human and technical resources. Securing the required financial resources has not been the only challenge, however. The high number of outbreaks means that WHO and partners faced shortages of diagnostics and case management kits as well as oral cholera vaccine (OCV) in 2022. Due to the global shortage of OCV, the International Coordinating Group (ICG) on Vaccine Provision had to reduce the OCV 2-dose regimen to a single dose.
While the negative impact of COVID-19 on health systems in every country and territory of the Region cannot be overestimated, the pandemic did also surface health system gaps that were subsequently addressed. In many countries/territories, WHO, the ministry of health and partners were able to identify such gaps in good time and improve the health system, most often by supporting the establishment of molecular testing capacity and oxygen plants and improving vaccine supply and cold chain management.
For almost all of the 61 reported outbreaks (excluding COVID-19), lack of integrated response plans in some of the affected countries and low coordination between the partners, especially on the outbreak response , led to fragmented response efforts and undermined the effectiveness of outbreak and emergency responses. This issue also resulted in reactive outbreak and emergency responses, and low cross-border collaboration between neighbouring countries in the Eastern Mediterranean Region. The sharing of health ministry information and outbreak data with partners remained suboptimal, which affected preparedness and timely interventions.
Recommendations
The work of WHO and its partners is based on humanitarian principles, which include humanity, impartiality, neutrality and independence. Together, WHO and its partners fight disease and hunger and reach the people most in need in all countries and territories around the world. It is thus necessary for governments and other stakeholders to grant us access to emergency-affected areas to support provision of essential health services.
The political leadership in the countries/territories, especially in fragile, conflict-affected and vulnerable (FCV) countries, needs to reaffirm its political support for improving the health of the population through close cooperation with donors and partners. Further, there is also an urgent need to improve coordination and communication among the United Nations sister agencies – especially WHO, the United Nations Children’s Fund (UNICEF) and the Food and Agriculture Organization of the United Nations (FAO) – by ensuring continuous engagement with external partners and donors, governments and communities. This could lead to trust-building, which may encourage the pooling of resources and bring about consensus on the division of responsibilities among stakeholders. Ultimately, this could result in timely and effective emergency responses.
The ministries of health and partners need to develop comprehensive preparedness and response strategies based on evidence and the on-the-ground realities. Having comprehensive preparedness and response strategies improves the effectiveness of the outbreak response and the efficient use of resources on the ground. There is also an urgent need to connect and improve the surveillance and laboratory systems and enhance coordination between these 2 vital pillars of the outbreak response. Neighbouring countries should improve cross-border collaboration and coordinate information sharing as well as outbreak investigation and response.
The ministries of health should work on a joint mechanism/platform (such as an early warning, alert and response network) to share the outbreak information on time with partners. The WHO country office should also facilitate information sharing with the WHO Regional Office for the Eastern Mediterranean and WHO headquarters via this platform.
Epidemiological situation and WHO response to outbreaks in the Eastern Mediterranean Region in 2022
1. Acute watery diarrhoea
Afghanistan
Following the collapse of the former Afghan government in August 2021, major donors halted funding to Afghanistan, which left its donor-dependent health system on the verge of collapse. Additionally, high levels of poverty, unemployment, and population movements increased the level of malnutrition, especially among children. Natural disasters (earthquakes and floods) further increase the risk of outbreaks of infectious diseases such as acute watery diarrhoea (AWD) in this country.
During the May to December 2022 outbreak, Afghanistan reported a cumulative total of 242 562 AWD cases, including 87 associated deaths (case fatality ratio [CFR]: 0.04%). More than 55% of the cases and almost 78% of the deaths were children aged under 5 years. The first few cases of AWD were reported on 4 May 2022 from Kandahar city, in Kandahar province; the outbreak then spread to 175 districts, affecting all 34 provinces of the country.
During the outbreak period, AWD cases were reported from all 34 provinces. The provinces most affected by the outbreak, however, were Kabul (56 106 cases; 23.1% of the cumulative cases), followed by Helmand (41 023; 16.9%), Baghlan (18 119; 7.5%), Nangarhar (12 845; 5.3%), Kandahar (12 748; 5.3%), Jowzjan (9371; 3.9%) and Paktia (8762; 3.6%). From week 18 to week 25 of 2022, the cases showed an increasing trend; however, the number of cases showed a slight reduction in weeks 26 and 27. The number of cases increased again in week 28 and peaked in weeks 30 and 31, with more than 12 500 cases reported weekly. Cases started to fall in number from week 32 but began to show a slight increase again in week 37. The cases showed a decreasing trend after week 37; the lowest number of cases was reported in week 52 of 2022.
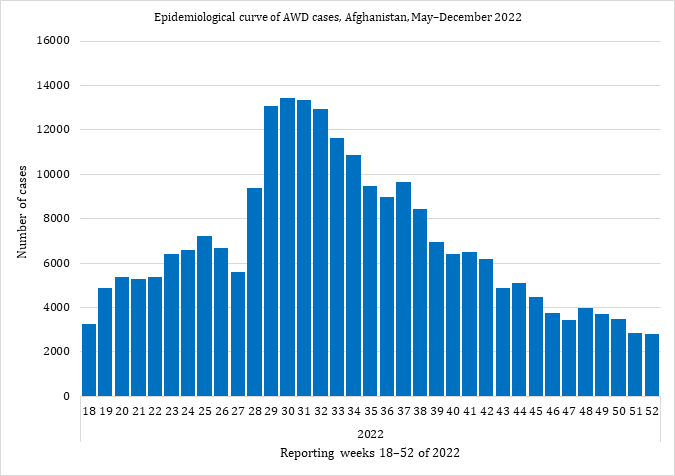 Fig. 2. Epidemiological curve of AWD cases, Afghanistan, May–December 2022
Fig. 2. Epidemiological curve of AWD cases, Afghanistan, May–December 2022
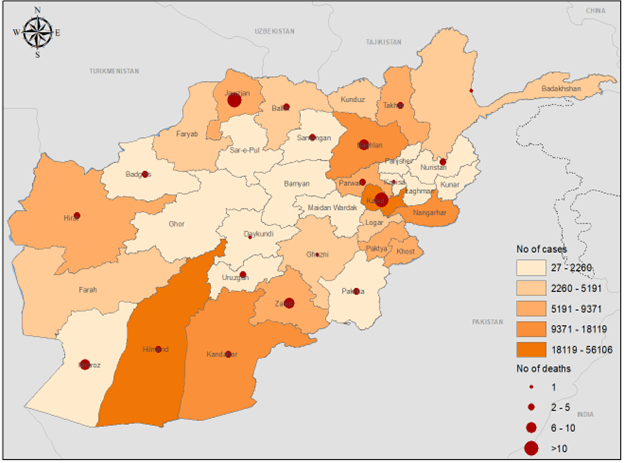 Fig. 3. Geographical distribution of AWD cases and deaths by province, Afghanistan, May–December 2022.
Fig. 3. Geographical distribution of AWD cases and deaths by province, Afghanistan, May–December 2022.
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city, or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO supported Afghanistan’s Ministry of Public Health (MOPH) in all response pillars for the prevention, control and management of this outbreak. WHO worked closely with MOPH and partners to improve coordination and the outbreak response.
Regular task force and Emergency Preparedness and Response Committee meetings took place at the national and provincial levels respectively to improve field investigation; active case finding; establishment of cholera treatment centres (CTCs), cholera treatment units (CTUs) and oral rehydration points (ORPs); and provision of AWD kits.
WHO strengthened coordination between the Health and WASH (Water, Sanitation and Hygiene) Cluster partners, which is where cholera response plans are developed, revised and updated. WHO continuously supported the surveillance and laboratory system of MOPH in Afghanistan through the provision of technical guidelines, capacity-building of staff, and provision of Cary-Blair transport media for specimens as well as rapid diagnostic tests (RDTs).
WHO worked closely with the country’s health sector to build the capacity of health workers on AWD case management. More than 1681 health workers have been trained on AWD case management since the start of the outbreak. WHO also provided more than 500 AWD case management kits and more than 1000 hygiene kits to Afghanistan in 2022.
WHO worked closely with partners to improve the WASH conditions of health facilities and the community, including through the provision of safe drinking water to the community, chlorination of wells and the building/rehabilitation of water systems in health facilities.
For risk communication and community engagement (RCCE), WHO used various media channels to support public awareness sessions on risk prevention, management of moderate AWD cases at home, and deciding when a patient needs to visit a health facility for their care.
2. Cholera
In 2022, 7 countries of the Eastern Mediterranean Region reported cholera outbreaks: Islamic Republic of Iran (confirmed cases: 367; deaths: 7), Iraq (suspected cases: 11 097; deaths: 24), Lebanon (suspected cases: 5422; deaths: 23), Pakistan (confirmed cases: 1002; deaths: 43), Somalia (suspected cases: 15 653; deaths: 88), Syria (suspected cases: 70 220; deaths: 102) and Yemen (suspected cases: 21 178; deaths: 21).
The recent cholera outbreaks in Lebanon and Syria are alarming as these 2 countries are not cholera-endemic and last experienced cholera outbreaks 29 years and 20 years ago respectively.
The cholera outbreaks in the Region in 2022 disproportionately affected children aged under 5 years, who accounted for more than half of suspected cholera cases in Afghanistan (55%) and in Somalia (65%). In addition, about 26% and 24% of suspected cholera cases in Lebanon and Yemen respectively were children aged under 5 years.
Islamic Republic of Iran
A cholera outbreak was reported from the Islamic Republic of Iran in July. By the end of October 2022, the country had reported 367 laboratory-confirmed cholera cases, including 7 cholera-associated deaths (case fatality ratio [CFR]: 1.91%). All these cases have been confirmed by culture as Vibrio cholerae biotype El Tor, serotype Ogawa.
Cases were mostly male (67%), aged 20–60 years (79%) and generally living in urban areas (81%). Most (97.06%) of the confirmed cases were Iranian citizens and only 2.2% were Afghan refugees living in the Islamic Republic of Iran. About 80% of cholera cases were imported (78% from Iraq), and 20% had a history of contact with Iranian passengers to Iraq. About two thirds (69%) of patients were hospitalized, while the rest were treated in an outpatient setting.
WHO supported the scaling up of the cholera response through a multidisciplinary approach that included strengthening surveillance and diagnostics; improving case management; strengthening water, sanitation and hygiene (WASH) systems through multisectoral mechanisms, infection prevention and control (IPC) measures, and guidance on water quality monitoring; and providing support to increase risk perception and knowledge among communities about the disease, its symptoms, associated risks, prevention and health-seeking behaviour.
Iraq
Cholera is endemic in Iraq with frequent upsurges in cases. The last large outbreak occurred in 2015, in which 4965 suspected cholera cases and 2 associated deaths (case fatality ratio [CFR]: 0.04%) were reported. Of the total suspected cases, 2868 were laboratory-confirmed cases, including the 2 cholera-associated deaths, from across 17 of Iraq’s 18 governorates.
Historically, cholera season starts in August or early September; however, in 2022, the cholera outbreak started earlier, and the first cases were reported on 19 June 2022. In 2022, Iraq reported 11 097 suspected cholera cases, including 3705 laboratory-confirmed cases and 24 cholera-associated deaths (CFR: 0.22%). Most of the confirmed cases (91.4%) were reported from 7 directorates of health, with the highest number of cases reported from Baghdad-Resafa (6041 cases), followed by Kirkuk (1676), Babylon (842) and Wassit (705).
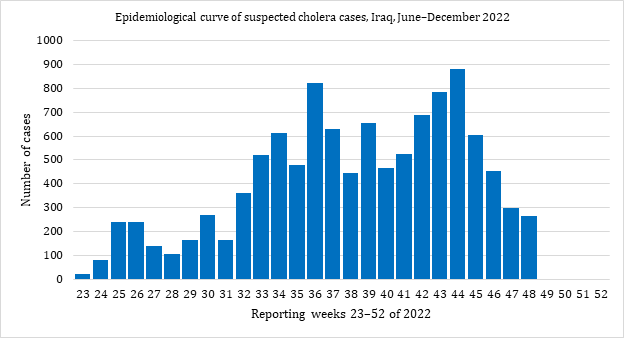 Fig. 4. Epidemiological curve of suspected cholera cases, Iraq, June–December 2022
Fig. 4. Epidemiological curve of suspected cholera cases, Iraq, June–December 2022
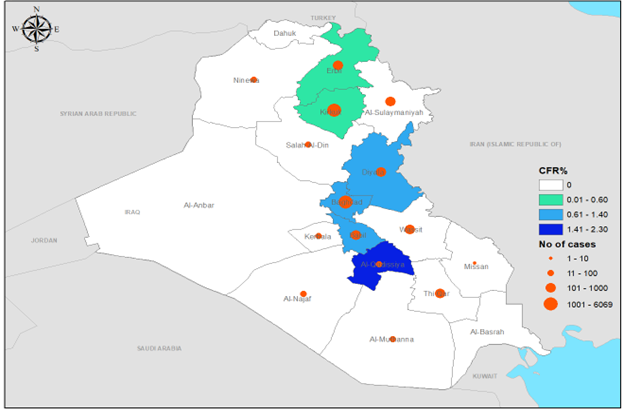 Fig. 5. Geographical distribution of suspected cholera cases and CFR by governorate, Iraq, June–December 2022
Fig. 5. Geographical distribution of suspected cholera cases and CFR by governorate, Iraq, June–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO supported Iraq’s Ministry of Health in implementing a comprehensive and multisectoral response plan, including surveillance; case management; water, sanitation and hygiene (WASH); logistics; and risk communication and community engagement (RCCE). WHO enhanced coordination among the relevant stakeholders for cholera prevention and response. WHO built the capacity of both the surveillance team and laboratory staff and provided them with updated technical guidelines as well as the required diagnostic kits.
WHO also supported the health authorities to monitor water quality in Iraq. In 2022, WHO trained 40 health workers on water quality monitoring. WHO also dispatched medicines and medical supplies to Sulaymaniyah governorate to support the regional health department in its response to the sudden cholera outbreak in the governorate. The package comprised medicines and medical supplies, including enough infusion sets, antibiotics and Ringer’s lactate solution to cover the needs of about 5000 people.
The WASH Cluster and sector response in Iraq primarily targeted 10 governorates, namely Duhok, Erbil and Sulaymaniyah in the Kurdistan region of Iraq, and Anbar, Baghdad, Basra, Diyala, Kirkuk, Ninewa and Salah al-Din in the federal region of Iraq. The WASH partners worked in these areas to meet the needs of internally displaced people in camps, returnees, and refugees in the affected governates. The response aimed to provide the WASH services needed by the affected populations and prevent and control cholera.
Lebanon
In 2022, Lebanon experienced its first cholera outbreak in almost 3 decades. The fragile health system – already affected by the economic and political crisis – was not ready to cope with such an outbreak. Responding to the cholera outbreak was therefore a more challenging task for the health ministry and its partners than for other cholera-endemic countries.
On 6 October 2022, the International Health Regulations national focal point notified WHO of 2 culture-confirmed cholera cases reported from the Akkar and North governorates. The outbreak started in week 42 of 2022 and cases showed an increasing trend until week 45, when the highest number of cases was reported. Cases showed a decreasing trend from week 46 to week 51, but the number of cases rose again in the last week of 2022.
From October to the end of December 2022, a total of 5422 suspected cholera cases, including 661 laboratory-confirmed cholera cases and 23 cholera-associated deaths (case fatality ratio [CFR]: 0.42%), were reported. Of the total cases, 29% were aged under 5 years, almost 53% were female, 29% were Syrian and only 19% of cases were admitted to hospital. At the national level, 20 of the 26 districts in Lebanon registered laboratory-confirmed cholera cases. Although the cumulative attack rate continued to be highest in the Akkar and North governorates, sporadic surges were reported in both the Baalbek-Hermel and Beqaa governorates.
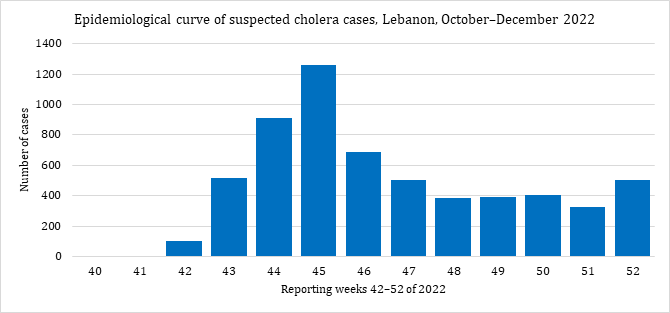 Fig. 6. Epidemiological curve of suspected cholera cases in Lebanon, October–December 2022
Fig. 6. Epidemiological curve of suspected cholera cases in Lebanon, October–December 2022
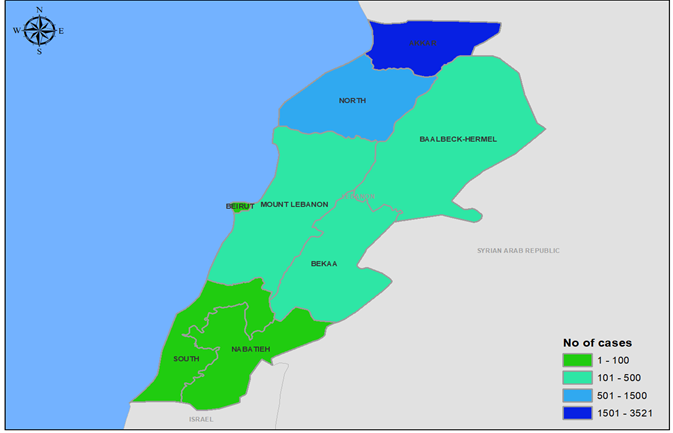 Fig. 7. Geographical distribution of suspected cholera cases by governorate, Lebanon, October–December 2022
Fig. 7. Geographical distribution of suspected cholera cases by governorate, Lebanon, October–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
Joint efforts and coordinated responses by WHO, Lebanon’s Ministry of Public Health, and partners to this outbreak proved effective, with the number of cholera cases significantly reduced through joint interventions and on-time response. WHO worked closely with the Joint National Health Sector Working Group to improve coordination and enhance response.
WHO supported surveillance and laboratories in terms of capacity-building, updating and provision of surveillance and case management guidelines, and provision of sample transport media and rapid diagnostic tests (RDTs). Laboratory directors and technicians were trained in bacteriological analysis.
Cholera treatment centres (CTCs), cholera treatment units (CTUs) and oral rehydration points (ORPs) were also set up, with the support of WHO, in cholera-affected areas.
To raise public awareness of the prevention, control and treatment of cholera, WHO worked closely with communities and partners by producing and distribution of information, education and communication materials such as child-friendly videos, brochures and leaflets.
WHO also supported an oral cholera vaccine (OCV) campaign. The first phase of the door-to-door OCV campaign, which was completed on 4 December 2022, saw 525 630 people receive a single dose. The target was to reach 600 000 people, giving an 87% coverage rate. The second phase of the OCV campaign, targeting high-risk areas, started on 17 December and over 80 000 people received a single dose of OCV. The Ministry of Public Health and partners intensified efforts to increase coverage and vaccine uptake, despite increased vaccine hesitancy and refusals. WHO continued to engage partners and advocate for joint efforts to sustain the cholera preparedness and response activities in Lebanon.
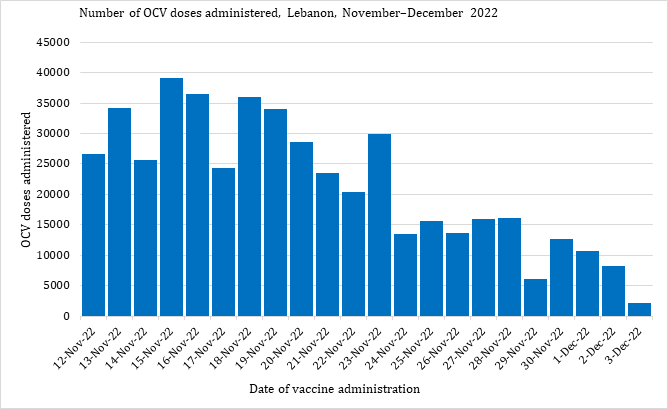 Fig. 8. Number of OCV doses administered, Lebanon, November–December 2022
Fig. 8. Number of OCV doses administered, Lebanon, November–December 2022
Pakistan
Although cholera is endemic in Pakistan, the last officially declared outbreak occurred following floods in 2010, with 168 confirmed cases reported. Since then, cholera cases have been reported in 5 of the last 11 years.
The 2022 cholera outbreak was first reported in Sindh province following laboratory confirmation of the first case on 15 January 2022. On 29 April 2022, Sindh’s Director-General for Health declared the cholera outbreak in Karachi. Cholera then started to spread, affecting more provinces. On 14 June 2022, Pakistan was hit by a devastating flood that affected more than 33 million people and displaced 500 000 people.
From January to December 2022, a total of 27 766 samples were tested, with 1002 laboratory-confirmed cholera cases. Pakistan also reported 43 cholera-associated deaths in 2022: 40 deaths in Balochistan and 3 in Khyber Pakhtunkhwa.
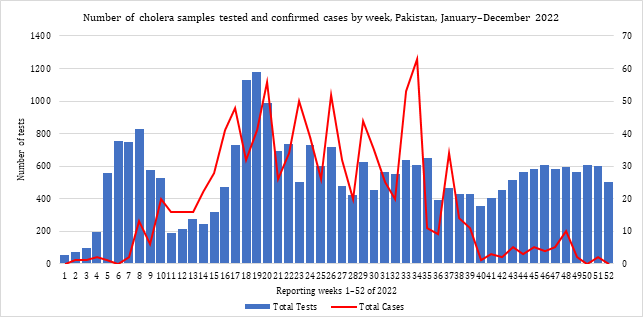 Fig. 9. Number of cholera samples tested and laboratory-confirmed cases by week, Pakistan, January–December 2022
Fig. 9. Number of cholera samples tested and laboratory-confirmed cases by week, Pakistan, January–December 2022
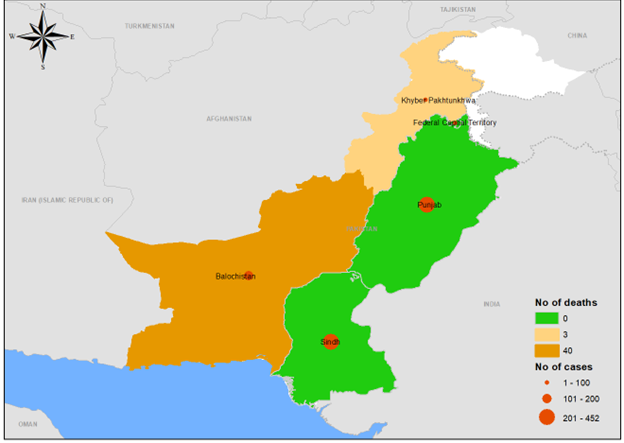 Fig. 10. Geographical distribution of suspected cholera cases by province, Pakistan, January–December 2022
Fig. 10. Geographical distribution of suspected cholera cases by province, Pakistan, January–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO supported the federal and provincial ministries of health in all response pillars: leadership and coordination, surveillance system, laboratory confirmation, case management, risk communication and community engagement (RCCE), water, sanitation and hygiene (WASH) and oral cholera vaccine (OCV). Examples of the support provided by WHO in Pakistan include the establishment of 813 surveillance sentinel sites for early detection of acute diarrhoeal cases; expansion of the number of technical laboratories for diagnosis of cholera from 6 to 38 laboratories; provision of Cary-Blair and sample transport media to outbreak-affected districts; development of a laboratory strategy; recruitment of human resources; and capacity-building of health workers.
With WHO support, an OCV campaign was also carried out in 4 provinces – Balochistan, Khyber Pakhtunkhwa, Punjab and Sindh –with more than 2.8 million people receiving a single dose of OCV (average coverage of 96%).
Table 1. Number of people who received OCV, Pakistan, 2022
|
Province |
No. targeted |
No. vaccinated |
Coverage (%) |
|
Balochistan |
754 784 |
675 916 |
89.6 |
|
Khyber Pakhtunkhwa |
383 531 |
415 984 |
108.5 |
|
Punjab |
1 196 939 |
1 144 058 |
95.6 |
|
Sindh |
590 878 |
571 823 |
96.8 |
|
Total |
2 926 132 |
2 807 781 |
96.0 |
Somalia
Somalia is considered one of the countries most affected by natural and human-made disasters. These emergencies have significantly undermined the health and well-being of millions of people in the country. According to WHO, more than 7.8 million people in 74 districts were affected by severe drought in 2022, with more than 1 million displaced from their homes. In addition, more than 4.3 million people faced severe food insecurity and over 6.4 million people lacked access to safe drinking water in 2022.
Further, the past 30 years of prolonged conflict, and the COVID-19 emergency, on top of political instability, climate change impacts, mass population displacement, poor water and sanitation infrastructure, and low awareness among the general population of prevention and control of infectious disease outbreaks, have created an environment conducive to the spread of infectious diseases, including cholera.
In 2022, a total of 15 653 suspected cholera cases, including 88 cholera-associated deaths (case fatality ratio [CFR]: 0.56%), were reported from 25 drought-affected districts. The number of suspected cases increased significantly from week 13 of 2022, with cases peaking in week 17. The number of suspected cases showed a decreasing trend from week 19 to week 30 of 2022, before switching back to an increasing trend for weeks 36 to 49 of 2022.
In total, 2200 samples were tested in 2022 at the National Public Health Laboratory in Mogadishu, of which 279 were positive for Vibrio cholerae O1 serotype Ogawa . Of the confirmed cases , 64% were children aged under 5 years and 48% were women. The highest incidences of confirmed cholera cases were reported in Daynile, Dharkenley, Kahda and Kismayo districts, while most of the deaths were reported from Daynile, Hawle Wadag, Kahda and Wanlaweyn districts.
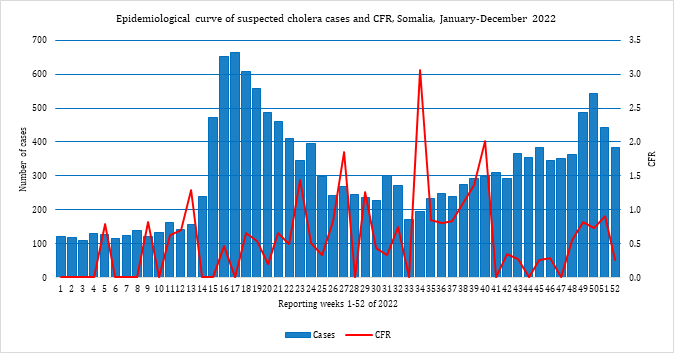 Fig. 11. Epidemiological curve of suspected cholera cases and CFR, Somalia, January–December 2022
Fig. 11. Epidemiological curve of suspected cholera cases and CFR, Somalia, January–December 2022
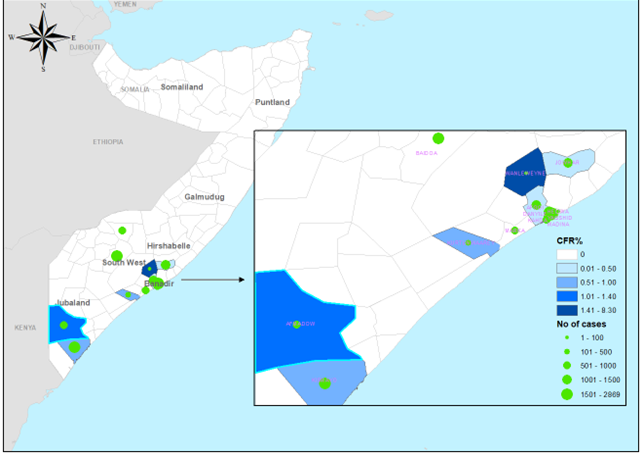 Fig. 12. Geographical distribution of suspected cholera cases and CFR by district, Somalia, January–December 2022
Fig. 12. Geographical distribution of suspected cholera cases and CFR by district, Somalia, January–December 2022
WHO, in close coordination with partners, supported Somalia’s Ministry of Health (MOH) and health system in all response pillars, including leadership and coordination, surveillance system, laboratory confirmation, case management, risk communication and community engagement (RCCE), water, sanitation and hygiene (WASH), and oral cholera vaccine (OCV) administration.
WHO conducted regular meetings and worked on improving coordination and response within the federal health authorities in Banaadir and the southern states . Following a WHO cholera risk assessment, the country was graded as very high risk. WHO also built the capacity of the surveillance and laboratory teams and provided them with updated guidelines, laboratory kits, sample transportation media and sample culture facilities. Samples were continually collected and sent to the National Public Health Laboratory in Mogadishu for culture and sensitivity studies as per the testing strategy. WHO also trained health workers in Somalia on cholera case management and provided case management, case investigation, and hygiene kits.
WHO worked closely with partners and the MOH to improve the WASH situation both in health facilities and in communities. In close coordination with the United Nations Children’s Fund (UNICEF) and MOH, WHO jointly worked on the provision of safe and clean drinking water to the country’s drought-affected districts. WHO technical experts supported the Health Cluster partners and MOH by providing health sensitization sessions targeting internally displaced people.
WHO also supported implementation of an oral cholera vaccine (OCV) campaign, during which 888 092 people aged 1 year and over received 2 doses of OCV, with 95% coverage in 9 districts (Table 2).
Table 2. Number of OCV doses administered by district, Somalia, 2022
|
District |
No. targeted |
No. vaccinated |
Coverage (%) |
|
Marka |
66 988 |
62 622 |
93 |
|
Afgoi |
97 196 |
93 371 |
96 |
|
Baidoa |
187 386 |
182 507 |
97 |
|
Dharkenley |
62 406 |
59 604 |
96 |
|
Daynile |
79 716 |
73 993 |
93 |
|
Hodan |
175 031 |
164 262 |
94 |
|
Jowhar |
57 578 |
56 512 |
98 |
|
Madina |
144 140 |
135 534 |
94 |
|
Wanlaweyn |
64 070 |
59 687 |
93 |
|
Total |
934 511 |
888 092 |
95 |
Syria
Basic infrastructure in Syria has been undermined by prolonged conflict, mass displacement, economic crisis, and political unrest. After almost 2 decades since the last confirmed case of locally transmitted cholera, the country experienced a cholera outbreak in 2022. This was alarming for other typically cholera-free countries in the Eastern Mediterranean Region, especially those countries neighbouring Syria. Previously, the last confirmed cholera case had been an imported case, reported in 2015 in Aleppo governorate, with no further local transmission documented.
The first case of the 2022 outbreak was detected on 22 August in Aleppo and confirmed on 25 August. On 10 September 2022, the Syrian Ministry of Health declared a cholera outbreak when 15 laboratory-confirmed cholera cases were reported from Aleppo governorate, including a single cholera-associated death. After that, cholera spread to all 14 governorates of Syria. From 25 August to 31 December 2022, a total of 70 220 suspected cholera cases were reported, with 102 associated deaths (case fatality ratio [CFR]: 0.15%), from the 14 governorates.
In 2022, a total of 4352 samples were tested using rapid diagnostic tests (RDTs), of which 1886 samples were positive for Vibrio cholerae. A total of 3336 stool samples were tested by culture and polymerase chain reaction (PCR) methods, of which 868 tested positive for V. cholerae, with a positivity rate of 26%. WHO supported antibiotics susceptibility in the country, where tests showed resistance for ampicillin, furazolidone, and nalidixic acid, and sensitivity for ciprofloxacin, azithromycin and trimethoprim/sulfamethoxazole.
The governorates most affected by the outbreak were Deir Al Zour (20 560 cases; 29.28% of the total cases), Edleb (17 784 cases; 25.33%), Raqua (14 372 cases; 20.47%) and Aleppo (14 064 cases; 20.03%). Additionally, 5037 suspected cases and 7 associated deaths were reported from camps for internally displaced people in northern Syria. Regarding age distribution, 44.58% of the suspected cases were aged under 5 years. Males accounted for 52% of all cases and females for 48%. Laboratory confirmation was carried out in 7 designated laboratories, including the Central Public Health Laboratory.
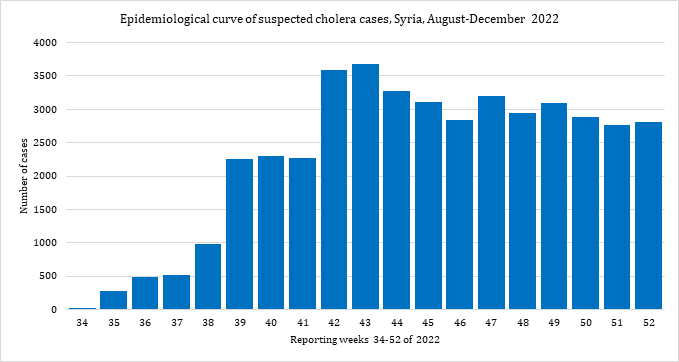 Fig. 13. Epidemiological curve of suspected cholera cases, Syria, August–December 2022
Fig. 13. Epidemiological curve of suspected cholera cases, Syria, August–December 2022
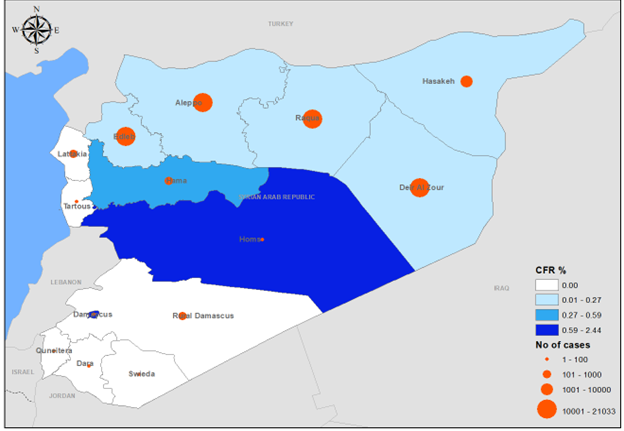 Fig. 14. Geographical distribution of suspected cholera cases and CFR by governorate, Syria, December 2022
Fig. 14. Geographical distribution of suspected cholera cases and CFR by governorate, Syria, December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO provided both technical and financial support to the health system of Syria in all outbreak response pillars: leadership and coordination; surveillance system; laboratory confirmation; case management; risk communication and community engagement (RCCE); water, sanitation and hygiene (WASH); and oral cholera vaccine (OCV). WHO trained health workers in various disciplines, including surveillance, laboratory confirmation, and case management, and provided them with technical guidelines and case management protocols.
To enhance active case finding and diagnose cholera on time, WHO supported Syria to establish a sample management system, including sample transportation, by ensuring the provision of sample transport media (Cary-Blair) and rapid diagnostic tests (RDTs) to health facilities in the country. WHO supported the establishment of cholera treatment centres (CTCs) and cholera treatment units (CTUs) and oral rehydration points (ORPs) across the affected areas, and provided them with the needed cholera kits, intravenous infusions and oral rehydration solution. WHO also worked closely with the WASH Cluster partners to provide safe drinking water and improve sanitation and hygiene for the prevention and control of cholera outbreaks.
Moreover, WHO supported Syria to receive 2 million doses of oral cholera vaccine (OCV) to implement a vaccination campaign (single-dose strategy) targeting 2 million people aged 1 year and over through 63 fixed facilities and 685 mobile teams. The campaign was implemented through fixed points as well as a door-to-door approach. About 1772 health workers were trained and deployed to deliver vaccination for this campaign, in addition to 36 supply officers and 97 supervisors from different levels will participate in the campaign. By end December 2022, more than 1 944 807 people aged 1 year and over (98% of the targeted population) were vaccinated against cholera in Syria.
In addition, on 29 December 2022, the International Coordinating Group (ICG) on Vaccine Provision approved 1 702 383 doses of OCV to conduct a reactive vaccination campaign (single-dose strategy) in northwest Syria targeting 3 subdistricts (A’zaz, Dana and Maaret Tamsrin).
Table 3. Number of people who received OCV, Syria, 2022
|
Governorate |
No. targeted |
No. vaccinated |
Coverage (%) |
|
Hasakeh |
395 423 |
399 948 |
101 |
|
Deir Ezzor |
750 000 |
763 601 |
102 |
|
Raqqa |
497 746 |
431 258 |
87 |
|
Aleppo |
350 000 |
350 000 |
100 |
|
Total |
1 993 169 |
1 944 807 |
98 |
Yemen
The cholera outbreak first reported in Yemen in October 2016 continued to affect the entire country in 2021 and 2022. A total of 21 178 suspected cholera cases, including 21 associated deaths (case fatality ratio [CFR]: 0.10%), were reported from Yemen in 2022. A total of 2282 rapid diagnostic tests (RDTs) were conducted, of which 657 were positive. The highest numbers of cases were reported in weeks 1 and 2 of 2022. After this period, the outbreak showed a decreasing trend overall, with few fluctuations in weeks 8, 20, 34 and 42 of 2022. The lowest number of cases was reported in week 51 of 2022.
WHO has supported health authorities in Yemen to prevent, control and manage the outbreak since cholera erupted in the country in 2016. WHO set up 28 public health emergency operations centres as part of the long-lasting response to the cholera outbreak in Yemen. WHO also provides cholera management kits to the existing cholera treatment centres (CTCs) or cholera treatment units (CTUs) in health facilities in Yemen.
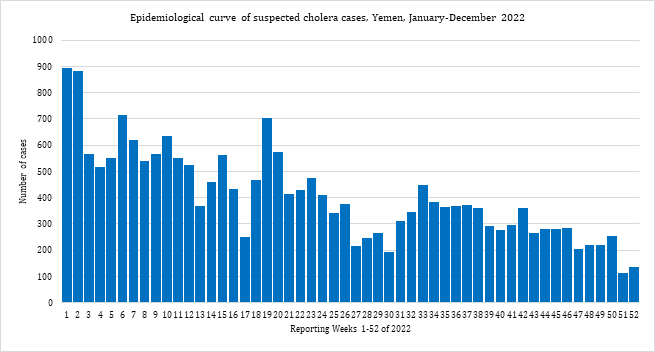 Fig. 15. Epidemiological curve of suspected cholera cases, Yemen, January–December 2022
Fig. 15. Epidemiological curve of suspected cholera cases, Yemen, January–December 2022
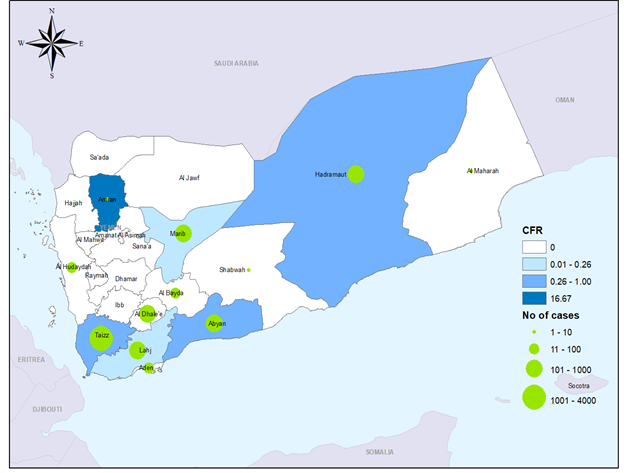 Geographical distribution of suspected cholera cases and CFR by governorate, Yemen, January–December 2022
Geographical distribution of suspected cholera cases and CFR by governorate, Yemen, January–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
3. Crimean-Congo haemorrhagic fever
Crimean-Congo haemorrhagic fever (CCHF) has been reported in the past few years from 4 countries of the Eastern Mediterranean Region: Afghanistan, Iraq, Oman and Pakistan. The largest CCHF outbreak in recent times, however, was reported from Iraq in 2022. In 2022, a total of 1759 suspected CCHF cases and 129 associated deaths (case fatality ratio [CFR]: 7.40%) were reported from 2 countries: Afghanistan (cases: 389; deaths: 15) and Iraq (cases: 1370; deaths: 114).
Afghanistan
Crimean-Congo haemorrhagic fever (CCHF ) is endemic in Afghanistan, with an upsurge in cases reported in 2018 and continuing to be reported until the end of 2022. From January to December 2022, a total of 389 suspected cases, including 103 laboratory-confirmed CCHF cases and 15 associated deaths (case fatality ratio [CFR]: 3.86%), were reported from 26 provinces across the country. Of the 389 suspected cases, 302 cases (77.4%) were male; all cases were aged over 5 years.
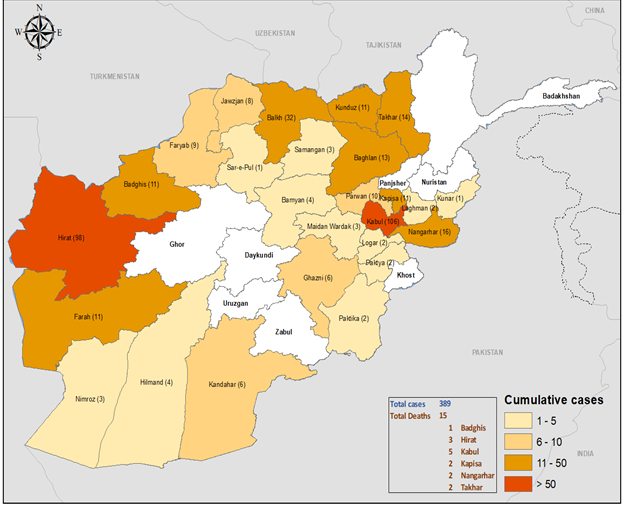 Fig. 17. Geographical distribution of suspected CCHF cases and deaths by province, Afghanistan, January–December 2022
Fig. 17. Geographical distribution of suspected CCHF cases and deaths by province, Afghanistan, January–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
Most of the cases in 2022 were reported from Kabul (106 cases; 27.0% of the total cases), Herat (98 cases; 25.2%) and Balkh (32 cases; 8.2%) provinces. The lowest numbers of cases were reported from Kunar (1) and Sari Pul (1) provinces. All reported deaths occurred in just 6 provinces, namely Kabul (5), Herat (3), Kapisa (2), Nangarhar (2), Takhar (2) and Badghis (1).
WHO continued to support Afghanistan’s Ministry of Public Health to strengthen multisectoral coordination and ensure the integration of outbreak response and control interventions. WHO supported both the surveillance and laboratory departments in Afghanistan by building the surveillance and laboratory teams’ capacities on case detection, outbreak investigation, sample collection, sample transportation and testing. WHO also ran training workshops for the surveillance support teams on outbreak response and case investigation.
WHO has continually supported the hospital system in Afghanistan in terms of the capacity-building of health workers on CCHF case management. In 2022, a total of 91 health workers were trained on CCHF case management in 33 provinces of the country. WHO supported health facilities and provided ribavirin and personal protective equipment (PPE) kits for CCHF case management.
Iraq
Crimean-Congo haemorrhagic fever (CCHF) is endemic in Iraq, and the first outbreak of the disease in the country was reported in 1979. Since then, 9 CCHF outbreaks have been reported in Iraq. Cases are usually reported in the summer season (July to September). In 2022, the biggest CCHF outbreak of the Eastern Mediterranean Region was reported in Iraq, with a total of 1370 suspected cases, including 380 confirmed cases and 114 associated deaths (case fatality ratio [CFR]: 8.3%).
The outbreak started in week 10 of 2022. Suspected cases showed an increasing trend from week 16, with the highest number of suspected CCHF cases reported in week 24 of 2022. The number of suspected cases started to show a decreasing trend from week 25 to week 28, while a significant increase in the number of cases was seen again in week 29 of 2022. Suspected cases showed a downward trend from week 30 to week 34. Suspected cases then increased slightly again after week 34 of 2022, with the outbreak showing a stabilizing trend for the rest of the year. The lowest number of cases was reported in week 52 of 2022.
In total, 114 deaths were reported among all CCHF cases in 2022, including 74 deaths among the confirmed CCHF cases. Dhi-Qar governorate reported the highest number of confirmed cases (155) and deaths (38) among the total confirmed cases. All governorates except Sulaymaniyah reported confirmed cases in 2022. Males accounted for more cases (60%) than females (40%). Adults were more affected, with the most affected age group those aged 25–44 years (35%) followed by those aged 15–24 years (24%) and 45–64 years (20%). Tick bites, contact with raw meat, and slaughtering of animals are considered the main risk factors for CCHF. Data analysis of CCHF cases in 2022 show that 16% of cases reported a history of a tick bite, 18% reported a history of contact with raw meat and 5% had a history of animal slaughtering.
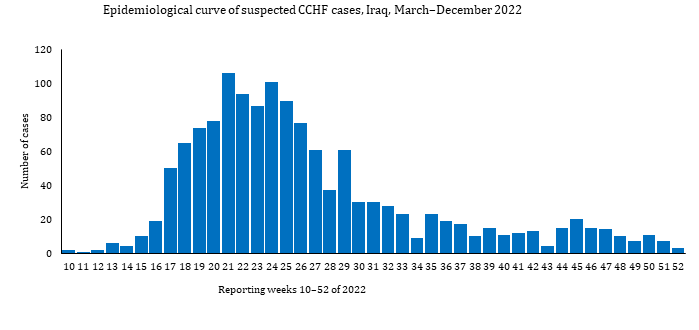 Fig. 18. Epidemiological curve of suspected CCHF cases, Iraq, March –December 2022
Fig. 18. Epidemiological curve of suspected CCHF cases, Iraq, March –December 2022
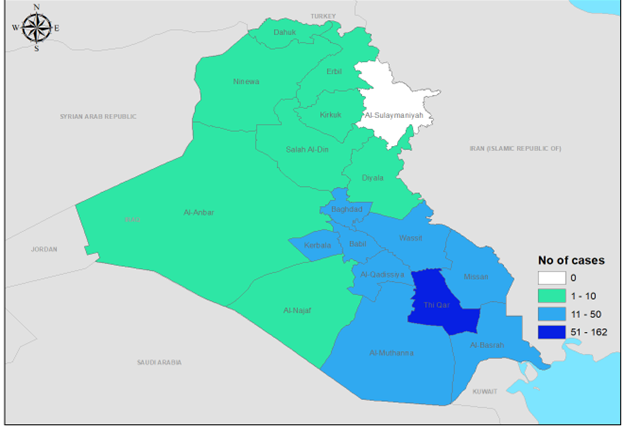 Fig. 19. Geographical distribution of CCHF cases by governorate, Iraq, March –December 2022
Fig. 19. Geographical distribution of CCHF cases by governorate, Iraq, March –December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO has been supporting Iraq’s Ministry of Health to strengthen CCHF surveillance, diagnostic capacity and outbreak response activities in terms of building rapid response team capacity and improving risk communication and community engagement (RCCE). WHO supported the CCHF laboratory with all the required diagnostic kits for diagnosis of CCHF and other viral haemorrhagic fevers. Information, education and communication materials were also distributed to raise public awareness of preventive measures to reduce the risk of CCHF transmission.
Médecins Sans Frontières (MSF), a WHO partner, supported case management and provided ribavirin to Iraqi health facilities in 2022.
4. Dengue fever
In 2022, a total of 100 432 dengue cases, including 164 associated deaths (case fatality ratio [CFR]: 0.002%) were reported from 6 countries of the Eastern Mediterranean Region: Afghanistan (suspected cases: 1266; deaths: 2), Oman (suspected cases: 579; deaths: 0), Pakistan (confirmed cases: 62 995; deaths: 62), Somalia (suspected cases: 5350; deaths: 18), Sudan (suspected cases: 5264; deaths: 37) and Yemen (suspected cases: 24 978; deaths: 45).
Afghanistan
Vector-borne diseases such as Crimean-Congo haemorrhagic fever (CCHF) and malaria are endemic to Afghanistan; however, dengue and chikungunya had not been reported in the country prior to 2018. Also, the presence of the vector Aedes aegypti – the main vector of dengue virus transmission – was not known in Afghanistan before 2018.
In 2018, the Ministry of Public Health (MOPH) conducted vector surveillance and collected samples, from Khost and Nangarhar provinces, that were morphologically identified as Ae. albopictus and Ae. aegypti. Afghanistan’s National Disease Surveillance and Response System had never reported dengue prior to 2019, when it reported the first 15 confirmed cases of dengue in the country.
Since 12 September 2021, Afghanistan has experienced a significant surge in suspected dengue cases. From September to December 2021, a total of 761 suspected cases were reported from 15 districts within Nangarhar province, with a single associated death. More than 90 of these suspected cases were confirmed by the Central Public Health Laboratory (CPHL) in 2021.
In 2022, Afghanistan reported 1266 suspected dengue cases, including 383 laboratory-confirmed cases and 2 associated deaths (case fatality ratio [CFR]: 0.16%). A total of 1246 samples were tested, of which 383 were positive (30.3%). The outbreak started in week 25 of 2022 and peaked in week 42 of 2022. Suspected cases showed a decreasing trend from week 49 to week 52 of the year. Of the 1266 suspected cases, 1242 cases (98.1%) were aged over 5 years and 294 cases (23.2%) were female.
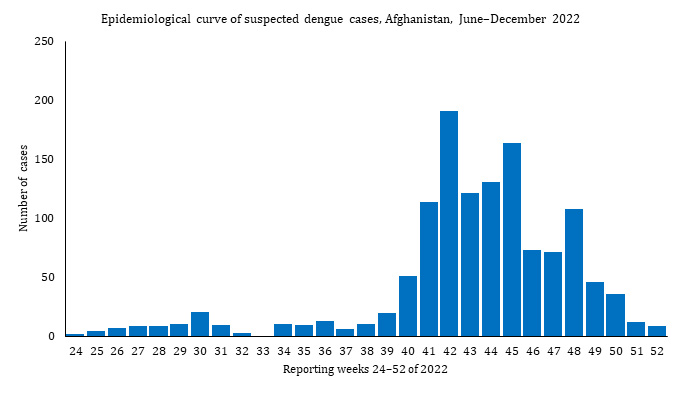 Fig. 20. Epidemiological curve of suspected dengue cases, Afghanistan, June–December 2022
Fig. 20. Epidemiological curve of suspected dengue cases, Afghanistan, June–December 2022
 Fig. 21. Geographical distribution of suspected dengue cases and deaths, Afghanistan, June–December 2022
Fig. 21. Geographical distribution of suspected dengue cases and deaths, Afghanistan, June–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO supported the MOPH in all response pillars , including surveillance systems, laboratory confirmation, vector control, case management, risk communication, community engagement (RCCE), and water, sanitation and hygiene (WASH). It provided 9 polymerase chain reaction (PCR) kits to the Nangarhar Regional Reference Laboratory in 2022. WHO also supported the MOPH in capacity-building of the surveillance and laboratory teams on outbreak investigation, sample transportation, and testing. Overall, 1000 kg of larvicides for vector control were provided to dengue hot spots in the country.
WHO supported health facilities with capacity-building for health workers and provided the required medicine for dengue case management. WHO also deployed experts for dengue surveillance, case management and vector control activities, and supported the development of a multisectoral costed response plan. Information, education and communication materials were distributed to raise public awareness of preventive measures to reduce the risk of dengue transmission.Oman
From 16 March to 13 August 2022, a total of 579 suspected dengue cases, with no associated deaths, were reported from Oman. Males accounted for 427 (73.7%) of these cases. The most affected age groups were those aged 20–40 years (330 cases; 57%), followed by those aged 41 years and above (212 cases; 37%). Most of the suspected cases were reported from Muscat governorate (538 cases; 93%); only 41 cases were reported by other governorates. All suspected dengue cases were epidemiologically linked to Muscat cases. Ninety cases (16%) were admitted to hospitals, and the common symptoms of those admitted were fever, body ache, headache and fatigue. Some cases also developed mild bleeding.
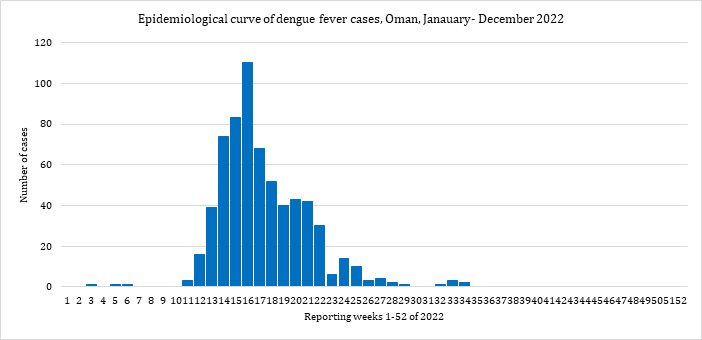 Fig. 22. Epidemiological curve of suspected dengue cases, Oman, March–August 2022
Fig. 22. Epidemiological curve of suspected dengue cases, Oman, March–August 2022
In 2021, a total of 293 579 suspected dengue cases were reported, including 47 439 laboratory-confirmed cases, and 236 associated deaths (case fatality ratio [CFR]: 0.5%).
Pakistan
Pakistan has been experiencing outbreaks of dengue over the past several years, affecting different parts of the country. The main vector of dengue virus transmission, Aedes aegypti, is well established in all parts of the country. All 4 types of dengue virus (DENV 1, DENV 2, DENV 3, DENV 4) have been reported in Pakistan.
In 2021, a total of 293 579 suspected dengue cases were reported, including 47 439 laboratory-confirmed cases, and 236 associated deaths (case fatality ratio [CFR]: 0.5%).
A dengue outbreak was reported in 2022, with a total of 62 995 confirmed dengue cases, including 62 associated deaths (CFR: 0.01%), from all provinces. The outbreak started in week 36 of 2022 and the highest number of cases was reported in week 42 of 2022. Cases showed a decreasing trend starting from week 43 of 2022, and the outbreak was over by week 47 of 2022. Almost 32% of the cases were reported from Sindh province, with 29% from Punjab (including the Islamabad Capital Territory), 25% from Khyber Pakhtunkhwa, and 14% from Balochistan.
WHO supported both of the federal and provincial ministries of health with the provision of case diagnosis and management guidelines throughout the country. Information, education and communication materials were distributed to raise public awareness of preventive measures to reduce the risk of dengue transmission.
WHO also deployed experts for dengue vector control activities, as well as for case management, laboratory investigation, and emergency risk communication. Support was also provided to the government through the timely arrangement of medical supplies for the management of severe cases by activation of the dengue management counter/corners in health facilities in the affected areas.
WHO has conducted strengthening of laboratory and hospital-based disease surveillance across all provinces in Pakistan; training of selected health care providers from all provinces; and training on vector surveillance and vector control, including source reduction during house visits. WHO also provided Pakistan with a total of 230 000 rapid diagnostic tests (RDTs) for dengue and other diseases, including malaria, acute watery diarrhoea, chikungunya, hepatitis A and hepatitis E.
Somalia
Somalia is a dengue-endemic country, with a few reported outbreaks, in 2011, 2013 and 2019. Dengue has been documented since 1985 among residents of a refugee camp near Hargeisa, as well as among journalists and aid workers involved in international humanitarian assistance in Somalia.
The 2022 outbreak started in mid-September, with an upsurge of suspected cases reported in the northern part of Somalia. From mid-September to 31 December 2022, Somalia reported a total of 5350 suspected dengue cases – most of which were reported from Somaliland – including 18 dengue-associated deaths (case fatality ratio [CFR]: 0.34%). Males accounted for more cases than females (52.1% versus 47.9%). The most affected districts in Somaliland were Hargeisa, Barao and Borama . In addition, the Banaadir region reported 34 suspected and 6 laboratory-confirmed dengue cases, along with a single dengue-associated death.
WHO has been supporting the country in all response pillars. Regular coordination meetings were convened with the Ministry of Health technical team and Health Cluster partners and a contingency plan for the prevention, control and management of dengue in Somalia was devised. A 3-level risk assessment for dengue in Somalia was conducted by a WHO team comprising WHO headquarters, regional office and country office personnel. The overall risk was classified as high nationally and regionally, and low globally.
WHO also scaled up disease surveillance for the timely detection of cases and listing the cases in a standard line list that was used to conduct a description of the cases reported. The WHO Regional Office for the Eastern Mediterranean arranged the capacity-building for frontline health workers on the management of dengue in Somalia. The WHO Somalia emergency technical team prepared and disseminated standard case management guidelines to frontline health workers to ensure appropriate management of cases.
Risk communication materials were translated, printed and distributed to all high-risk locations. Through Radio Ergo, WHO sensitized high-risk communities on the prevention of dengue. An estimated 2 million people, mostly in Mogadishu, were reached with these messages.
Further, rapid diagnostic tests (RDT) were provided to the 3 state-based laboratories. The kits were sufficient to test 5000 suspected cases of dengue and other arboviruses. Fogging of 2327 households – with an estimated 20 726 household members in total – was conducted to reduce the density of the vector responsible for transmitting dengue. WHO also supported the scaling up of vector surveillance in Mogadishu to establish the location of mosquito breeding sites for targeted interventions.
Sudan
Dengue is endemic in Sudan, and several outbreaks have been documented in the country – in 2010, 2013, 2017 and 2019. In 2022, a total of 5264 suspected dengue cases, including 817 laboratory-confirmed cases, were reported from Sudan. Among the total reported cases, 37 associated deaths were also reported (case fatality ratio [CFR]: 0.70%).
The outbreak started in week 31 of 2022 and the number of suspected cases significantly increased in week 40 of 2022. The highest number of suspected cases was reported in week 45, following which suspected cases showed a decreasing trend. The lowest number of suspected cases was reported in week 52 of 2022 .
The suspected cases and deaths were reported from 70 localities across 11 states, with an overall attack rate of 3.9 cases per 10 000 population. Most of the suspected cases were reported from North Kordofan state (27.4%), followed by North Darfur (26.1%), West Kordofan (21.0%), White Nile (13.3%) and Kassala (6.4%). Regarding the associated deaths, North Kordofan reported the most deaths, followed by Red Sea, West Kordofan and North Darfur.
Males accounted for 43% of the suspected cases and all age groups were affected, with 23% of cases in the 10–19 years age group. Most of the cases presented with fever (92%), followed by headache (81%), joint pain (78%), muscle pain (54%), backache (47%) and loss of appetite (47%). Less than 15% of cases presented with skin rash, bleeding and loss of consciousness.
A total of 1913 samples were collected for testing, of which 827 cases (43%) were positive. The highest positive results were from North Darfur State (632 confirmed cases; 76.4%), followed by North Kordofan (56 confirmed cases; 6.7%), West Kordofan (45 confirmed cases; 5.4%), White Nile (28 confirmed cases; 3.3%), Kassala (24 confirmed cases; 2.9%), Red Sea (22 confirmed cases; 2.6%), East Darfur (6 confirmed cases; 0.7%), South Darfur (5 confirmed cases; 0.6%), South Kordofan (5 confirmed cases; 0.6%) and West Darfur (4 confirmed cases; 0.4%).
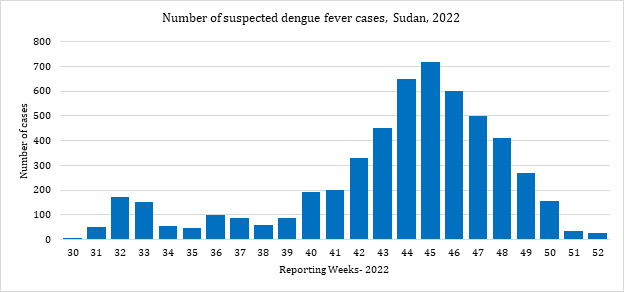 Fig. 23. Epidemiological curve of suspected dengue cases, Sudan, July–December 2022
Fig. 23. Epidemiological curve of suspected dengue cases, Sudan, July–December 2022
WHO has been supporting Sudan’s Ministry of Health in implementing response activities across all strategic pillars of response, including activating a public health emergency operations centre to oversee and coordinate all response activities; conducting capacity-building sessions; strengthening surveillance; enhancing laboratory capacity; and providing rapid diagnostic tests (RDTs).
Moreover, support was provided for early detection and confirmation, such as to implement integrated vector management. This included prevention of mosquito breeding by applying insecticides, as well as environmental management and modification to stop mosquitos from accessing egg-laying habitats. Community education on the risks of mosquito-borne diseases was also provided, along with community engagement to improve participation in and mobilization for sustained vector control.
Yemen
Dengue is also considered endemic to Yemen. The country’s first dengue outbreak, which was reported from the Shabwah governorate in January 2018, continued into 2021. In 2021, a total of 1061 cases, including 66 deaths, were reported from 14 governorates. Of 262 samples tested for dengue, 44 were positive. In 2022, Yemen reported 25 884 suspected dengue cases, including 45 dengue-associated deaths (case fatality ratio [CFR]: 18%) in the south of the country. Most of the total cases (59%) were male; half of all cases (50%) were aged 15–24 years.
The dengue outbreak in Yemen started in week 1 of 2022, with the number of cases significantly increasing in the south of the country in week 15 of 2022. The north of the country reported an increasing trend as of week 42 of 2022. The outbreak had several peaks, with the highest number of cases reported in week 43 of 2022 in the north of the country.
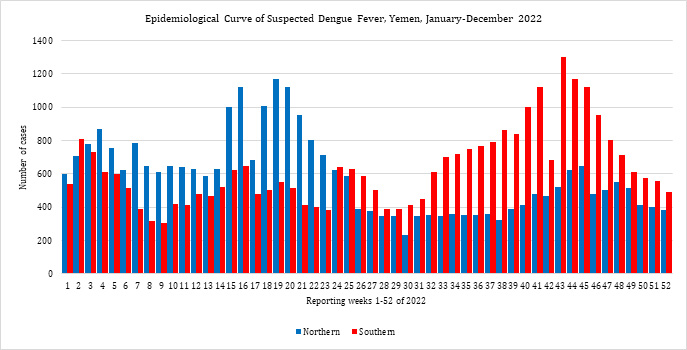 Fig. 24. Epidemiological curve of suspected dengue cases, Yemen, January–December 2022
Fig. 24. Epidemiological curve of suspected dengue cases, Yemen, January–December 2022
WHO supported Yemen to conduct disease surveillance through the electronic Diseases Early Warning System (eDEWS) because of disruption to the routine surveillance system. Regular technical and financial support was also extended for laboratory diagnosis and case confirmation, case management and vector control activities. WHO strengthened collaboration and coordination with national and international partners to conduct an integrated response and for optimal use of resources.
WHO also supported space fogging, larval detection, and control in high-incidence areas (Taiz, Hudaydah, Hajjah). Rapid response teams provided health education on vector prevention to affected households. Case management training was also provided to health workers in high-risk areas, as dengue cases are managed in the health facilities in the affected areas.
5. Diphtheria
Pakistan
Diphtheria cases have been reported from Pakistan in the last 3 consecutive years. A total of 339 and 333 suspected diphtheria cases were reported from the country in 2020 and 2021 respectively. In 2022, Pakistan reported a total of 351 suspected diphtheria cases, including 36 laboratory-confirmed cases and 46 diphtheria-associated deaths (case fatality ratio [CFR]: 13.11%), from 4 provinces.
The 2022 outbreak started in week 1 of 2022 and the number of suspected cases increased significantly from week 33 of 2022. The highest number of suspected cases was reported in week 42. The outbreak continued until the end of 2022, with noticeable increases in the number of suspected cases in weeks 40, 42, 43, 47 and 49. Suspected cases then showed a stabilizing trend in the last 4 weeks of the year.
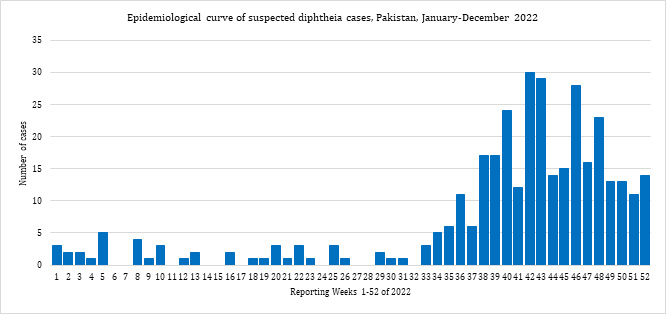 Fig. 25. Epidemiological curve of suspected diphtheria cases, Pakistan, January–December 2022
Fig. 25. Epidemiological curve of suspected diphtheria cases, Pakistan, January–December 2022
Most of the suspected cases (74.4%) were reported from Khyber Pakhtunkhwa, Sindh (16.0%) and Punjab (8.0%), while the smallest share of suspected cases was reported from Balochistan (1.4%). Most of the cases were aged over 5 years.
WHO supported both the federal and provincial ministries of health in all response pillars, including coordination, surveillance, case management, contact tracing and provision of diphtheria antitoxin. Appropriate prophylactic treatment is recommended to save lives and limit diphtheria transmission, while targeted vaccination campaigns in the most affected districts are crucial to interrupt diphtheria transmission.
6. Malaria
In 2022, a total of 3 606 981 malaria cases, including 262 associated deaths (case fatality ratio [CFR]: 0.01%), were reported from 4 countries of the Eastern Mediterranean Region: Djibouti (confirmed cases: 40 648; deaths: 0), Islamic Republic of Iran (suspected cases: 4425; deaths: 0), Pakistan (suspected cases: 937 906; deaths: 0) and Sudan (suspected cases: 2 624 002; deaths: 262).
WHO has been supporting the 4 countries with malaria outbreaks in 2022 across all response pillars from prevention, control, detection and diagnosis to outbreak management. WHO supported capacity-building for the surveillance, laboratory and hospital systems in these countries for active case finding, diagnosis and case management of malaria. WHO provided rapid diagnostic tests (RDTs) for early diagnosis of the cases, and in close coordination with partners, WHO supported the health ministries with the provision of antimalarial drugs as well as long-lasting insecticidal nets.
Djibouti
Djibouti is a malaria-endemic country, and reports of malaria cases from this country showed an increasing trend from 2011 to 2020. The highest number of cases was reported in 2020, following which the number of malaria cases declined in 2021 and 2022. In 2022, a total of 40 648 laboratory-confirmed malaria cases, with no associated deaths, were reported from Djibouti. Most of the reported cases were caused by Plasmodium falciparum (77% of cases), followed by P. vivax (23%). The primary vectors involved were the invasive Anopheles stephensi and An. arabiensis.
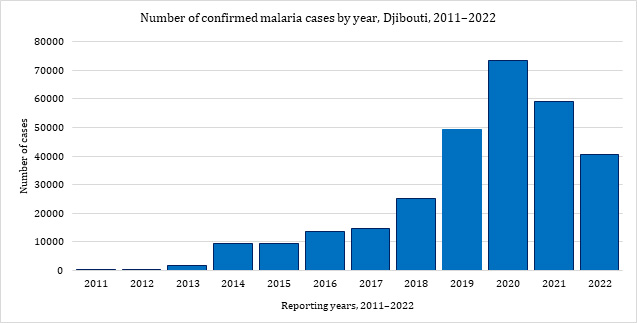 Fig. 26. Epidemiological curve of confirmed malaria cases per year, Djibouti, 2011–2022
Fig. 26. Epidemiological curve of confirmed malaria cases per year, Djibouti, 2011–2022
Islamic Republic of Iran
In 2022, the Islamic Republic of Iran reported 4425 suspected cases of malaria, including 1013 locally transmitted cases. Malaria outbreaks have been reported in the country since 2010 and the highest number of cases in the last 13 years was reported in 2022. The suspected cases were concentrated around the border area where the Sistan and Baluchestan province of the Islamic Republic of Iran meets the Balochistan province of Pakistan. Although malaria is endemic in the Islamic Republic of Iran, imported cases are regularly reported from this area due to cross-border movements.
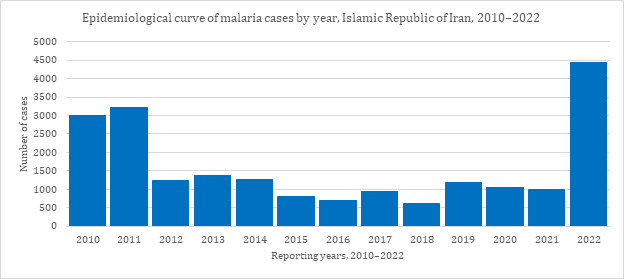 Fig. 27. Epidemiological curve of malaria cases by year, Islamic Republic of Iran, 2010–2022
Fig. 27. Epidemiological curve of malaria cases by year, Islamic Republic of Iran, 2010–2022
Pakistan
An alarming increase in malaria cases was reported following the floods in Pakistan that started in June 2022. Pakistan reported over 3.4 million suspected cases of malaria in 2022, compared with 2.6 million suspected cases reported in 2021. Over 937 906 cases were laboratory confirmed, of which 23% were due to Plasmodium falciparum, which is associated with the most severe and fatal cases. High-burden districts were in the Sindh, Balochistan and Khyber Pakhtunkhwa provinces.
Sudan
Sudan is a malaria-endemic country, but there was a significant increase in the number of suspected malaria cases in the last 3 months of 2022 compared with the same period in 2020 and 2021. In 2022, Sudan reported 2 624 002 suspected malaria cases, including 1 214 297 laboratory-confirmed malaria cases and 262 associated deaths (case fatality ratio [CFR]: 0.01%).
More than 120 000 laboratory-confirmed malaria cases were reported in January 2022, with a slight reduction in the number of cases in February 2022. The cases showed a decreasing trend from March to May 2022, with the lowest number of cases reported in May. The confirmed cases showed a stabilizing trend during June and July 2022, while the number of cases increased again in August, September and October 2022. The highest number of cases was reported in October, with cases then showing a decreasing trend in November and December 2022.
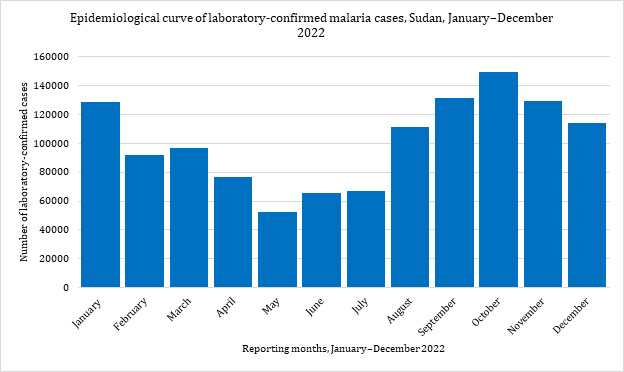 Fig. 28. Epidemiological curve of laboratory-confirmed malaria cases by month, Sudan, January–December 2022
Fig. 28. Epidemiological curve of laboratory-confirmed malaria cases by month, Sudan, January–December 2022
7. Measles
Globally, both the number of measles cases and the number of affected countries significantly increased in 2022. There was a 79% year-on-year increase in the number of measles cases globally in the first 2 months of 2022, with children aged under 5 years the most affected age group.
In the Eastern Mediterranean Region, a total of 143 735 suspected measles cases, including 588 associated deaths (case fatality ratio [CFR]: 0.41%), were reported from 8 countries in 2022: Afghanistan (suspected cases: 77 210; deaths: 388), Djibouti (suspected cases: 209; deaths: 0), Islamic Republic of Iran (suspected cases: 10 620; deaths: 0), Pakistan (suspected cases: 17 737; deaths: 117), Somalia (suspected cases: 17 361; deaths: 0), Sudan (suspected cases: 3310; deaths: 4), Syria (suspected cases: 6309; deaths: 2) and Yemen (suspected cases: 10 979; deaths: 77).
This acute increase in the number of measles outbreaks in the Region is alarming and indicates an urgent need to strengthen routine immunization programmes in the affected countries.
Afghanistan
In 2022, the Ministry of Public Health (MOPH) in Afghanistan reported 77 210 suspected measles cases, including 5787 confirmed cases, along with 388 associated deaths (case fatality ratio [CFR]: 0.50%), from all 34 provinces of the country. This represents a significant year-on-year increase in the number of suspected measles cases and associated deaths. In 2021, a total of 30 199 suspected measles cases, including 108 associated deaths (CFR: 0.36%), were reported from Afghanistan.
The 2022 outbreak started in week 1 of 2022 and the highest number of cases was in week 15 of 2022. The outbreak showed a decreasing trend between weeks 16 and 32 of the year. From week 32 to week 52 of 2022, the outbreak showed a stabilizing trend. The most affected provinces were Badakhshan (11.4% of all suspected cases ), Kabul (11%), Nangarhar (9.8%), Helmand (8.5%), Kunduz (7.3%), Takhar (5.1%) and Hirat (4.9%).
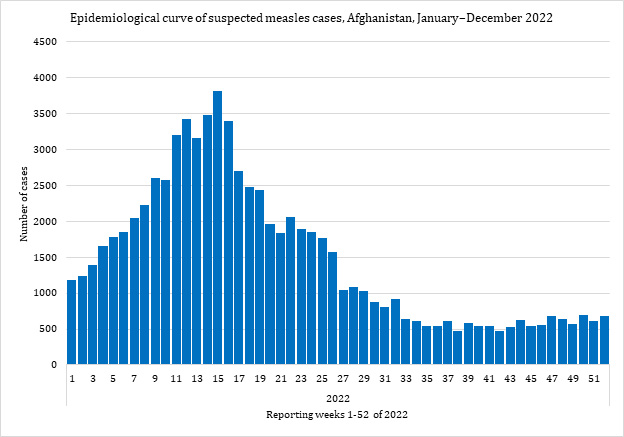 Fig. 29. Epidemiological curve of suspected measles cases, Afghanistan, January–December 2022
Fig. 29. Epidemiological curve of suspected measles cases, Afghanistan, January–December 2022
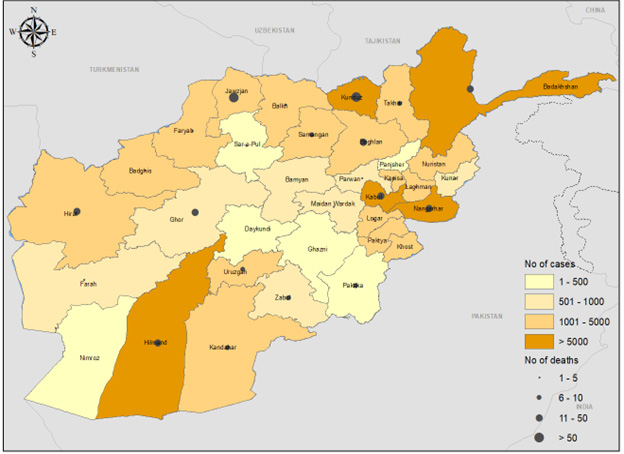 Fig. 30. Geographical distribution of suspected measles cases and deaths, Afghanistan, January–December 2022
Fig. 30. Geographical distribution of suspected measles cases and deaths, Afghanistan, January–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO supported the MOPH and partners to monitor and respond to the country-wide measles outbreak. From December 2021 to December 2022, about 11 million children (aged 6 months to 14 years) were vaccinated through 5 different measles outbreak response and national immunization campaigns across all 34 provinces. Additionally, a total of 593 measles kits were supplied to 28 provinces in 7 regions across the country to support case management.
Djibouti
In 2022, a total of 209 suspected measles cases were reported from Djibouti, including 39 laboratory-confirmed cases, with no associated deaths. WHO supported the country on both case management and a measles immunization campaign. The outbreak response campaign was conducted from 11 to 15 September 2022. The campaign targeted 45 400 children aged 6–59 months in 10 districts across 4 provinces.
Islamic Republic of Iran
In 2022, a total of 10 620 suspected measles cases, with no associated deaths, were reported from the Islamic Republic of Iran. From January to December 2022, a total of 10 146 samples were tested, of which 228 were positive. The outbreak started in January 2022 and the highest numbers of cases were reported in April and May of that year. The outbreak showed a stabilizing trend from July to December 2022.
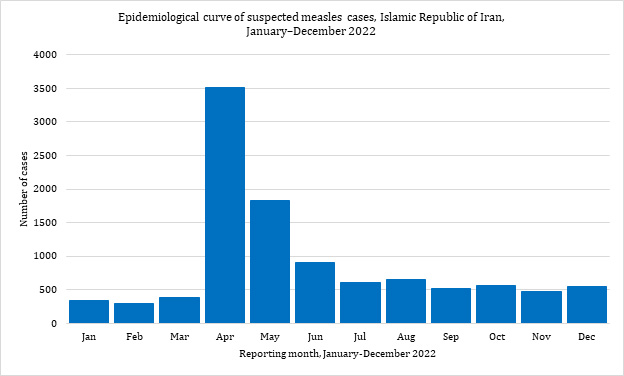 Fig. 31. Epidemiological curve of suspected malaria cases, Islamic Republic of Iran, January–December 2022
Fig. 31. Epidemiological curve of suspected malaria cases, Islamic Republic of Iran, January–December 2022
WHO supported a measles vaccination activities at the points of entry from Afghanistan and Pakistan. In addition, 655 000 child and adult Afghan refugees aged 9 months to 30 years living in the Islamic Republic of Iran were also vaccinated in 2022.
Syria
In 2022, cumulatively 6309 suspected measles cases and 3116 laboratory-confirmed measles cases, with 2 measles-associated deaths (case fatality ratio [CFR]: 0.04%), were reported from different districts of north-west Syria. Although measles cases were reported from the beginning of 2021, the number of cases significantly increased in 2022.
The outbreak showed an increasing trend for weeks 1 to 13 of 2022, however, trend of the suspected cases decreased from weeks 14 to 19 of the year. The highest number of cases was reported in week 22 of 2022. The number of cases reduced from week 27 to week 29 of 2022, followed by an overall stable trend with some fluctuation until week 29. There was then a further increase in the number of cases in the last 2 weeks of the year.
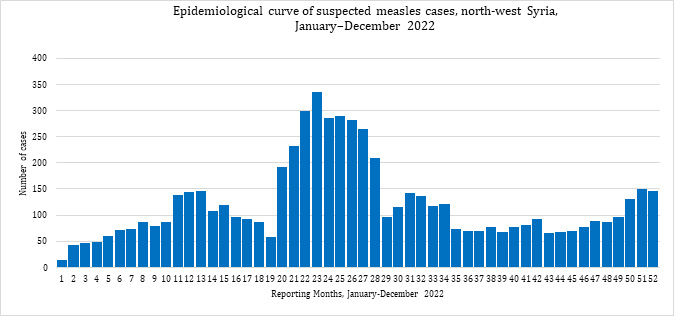 Fig. 32. Epidemiological curve of suspected measles cases, north-west Syria, January–December 2022
Fig. 32. Epidemiological curve of suspected measles cases, north-west Syria, January–December 2022
WHO supported the health system in Syria in 2022 with the management of measles cases. The measles outbreak campaign was conducted from 9 to 19 September 2022, targeting 535 668 children aged 6 to 83 months in north-west Syria with measles and rubella vaccine.
Pakistan
In 2022, a total of 17 737 suspected measles cases were reported from Pakistan, including 117 measles-associated deaths (case fatality ratio [CFR]: 0.66%). From January to December 2022, a total of 15 616 samples were tested, of which 6316 were positive. The outbreak started in January 2022 and the highest number of suspected cases was reported in March 2022. The number of cases showed a significant reduction after the month of June, with the lowest number of cases reported in August 2022. There was, however, then a slight increase in the number of cases from September to December 2022.
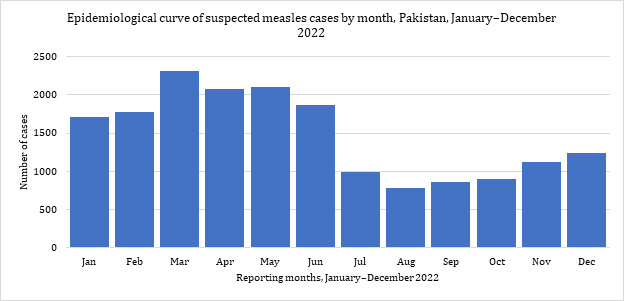 Fig. 33. Epidemiological curve of suspected measles cases, Pakistan, January–December 2022
Fig. 33. Epidemiological curve of suspected measles cases, Pakistan, January–December 2022
Somalia
Measles is endemic in Somalia, with recurrent upsurges of cases. In 2021, the number of suspected cases of measles increased in comparison to previous years (2596 suspected cases in 2020, 4442 suspected cases in 2019). This surge in cases is linked to a decrease in measles vaccination coverage of children aged under 5 years. In 2021, a total of 7494 suspected cases of measles were reported from 66 drought-affected districts, of which 80% of cases (5995 cases) were children aged under 5 years.
In 2022, a total 17 361 of suspected measles cases, including 9977 laboratory-confirmed cases and no associated deaths, were reported from Somalia. Although the outbreak started in week 1 of 2022, the highest number of cases was reported in week 9 of 2022. The outbreak continued with several spikes until week 21 of 2022, after which the cases showed a stable trend of 200–300 cases weekly until the end of the year.
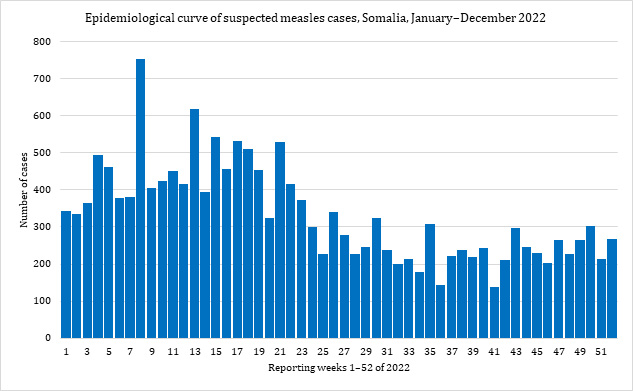 Fig. 34. Epidemiological curve of suspected measles cases, Somalia, January–December 2022
Fig. 34. Epidemiological curve of suspected measles cases, Somalia, January–December 2022
WHO supported the Federal Ministry of Health and partners to monitor and respond to the country-wide measles outbreak. Immunization activities to enhance measles vaccination coverage were conducted. A measles vaccination campaign, also covering vitamin A supplements, deworming, and oral poliovirus vaccine (OPV), was conducted from 16 to 21 October 2022. The campaign covered 2.6 million children aged 6 to 59 months in 71 districts across 5 southern governorates.
Sudan
In 2022, a total of 3406 suspected measles cases, including 1262 laboratory-confirmed cases and 13 associated deaths, were reported from Sudan (case fatality ratio [CFR]: 0.38%). Children aged under 5 years were the age group most affected by the measles outbreak, accounting for 65% of suspected cases. Most of the laboratory-confirmed cases were reported from the Red Sea, Kassala and East Darfur states.A measles outbreak was first detected at a primary health care centre in the Kario camp, East Darfur, in early 2022. By end December 2022, 17 of Sudan’s 18 states had reported either laboratory-confirmed or epidemiologically linked cases. Although the measles outbreak began in January 2022, the number of suspected measles cases significantly increased in March 2022. The peak of the outbreak was reported the same month. From June to August, the number of cases rose again, with a noticeable increase in September and October 2022, after which the number of cases had a reducing trend.
WHO supported Sudan’s surveillance system and provided updated surveillance, case management and laboratory guidelines. Surveillance and health workers were trained in active case finding and the management of measles cases in the health facilities. Risk communication and community engagement (RCCE) materials were distributed to the affected communities and to health workers.
8. Middle East respiratory syndrome (MERS)
From April 2012 to December 2022, a total of 2603 laboratory-confirmed cases of Middle East respiratory syndrome (MERS) were reported globally, with 935 associated deaths, giving a case fatality ratio (CFR) of 36%. These MERS cases were reported from 27 countries globally, 12 of which are in the Eastern Mediterranean Region. Most of the cases were reported from Saudi Arabia: 2195 cases, with 854 related deaths (CFR: 39%). Most of the global MERS cases (69%) were male, and the median age of the cases was 52 years (interquartile range: 38–65 years).
In 2022, a total of 9 MERS cases, including one associated death (CFR: 11.11%), were reported from 3 countries of the Eastern Mediterranean Region: Oman (cases: 2; deaths: 1), Qatar (cases: 2; deaths: 0) and Saudi Arabia (cases: 5; deaths: 0). A total of 20 cases were reported from the Region in 2021, while 60, 225 and 145 cases were reported from the Region in 2020, 2019 and 2018 respectively.
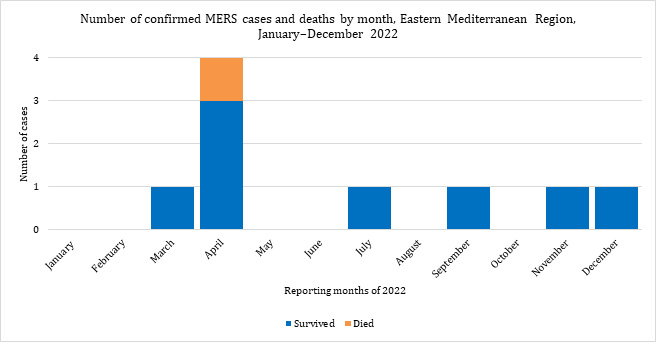 Fig. 35. Number of confirmed MERS cases and deaths by month, Eastern Mediterranean Region, January–December 2022
Fig. 35. Number of confirmed MERS cases and deaths by month, Eastern Mediterranean Region, January–December 2022
WHO continues to work with the ministries of health in affected and at-risk countries across the Region and with international partners to better understand transmission patterns and risk factors of Middle East respiratory syndrome coronavirus (MERS-CoV) infection in community and health care settings. WHO works closely with partners to develop improved measures to prevent human infections.
Despite a reduction in case detection, MERS-CoV is circulating in dromedary camels across large parts of the Middle East and Africa. Based on WHO’s regularly updated guidelines, individuals presenting with respiratory symptoms who have recently visited the Middle East must be asked whether they had any direct or indirect contact with dromedary camels. WHO continues to review and update, as necessary, all WHO information products and guidance materials.
9. Mpox (monkeypox)
Mpox (monkeypox) is a viral zoonosis (a virus transmitted to humans from animals) with symptoms like those seen in the past in smallpox patients, although it is clinically less severe.
In May 2022, multiple cases of mpox were identified in several non-endemic countries. Globally, more than 80 000 cases, including 80 mpox-associated deaths, were reported from May to December 2022. Most of the cases were reported by the United States of America (29 000), followed by Brazil (10 680), Spain (7514), France (4114), Colombia (4000), United Kingdom of Great Britain and Northern Ireland (3735), Mexico (3696), Peru (3711), Germany (3684) and Canada (1460).
In the Eastern Mediterranean Region, 80 laboratory-confirmed mpox cases were reported from across 10 countries, including one mpox-associated death from Sudan. Most of the cases were reported from Lebanon (24), followed by Sudan (18), United Arab Emirates (16), Saudi Arabia (8), Qatar (5), Morocco (3), Egypt (3), Bahrain (1), Islamic Republic of Iran (1) and Jordan (1).
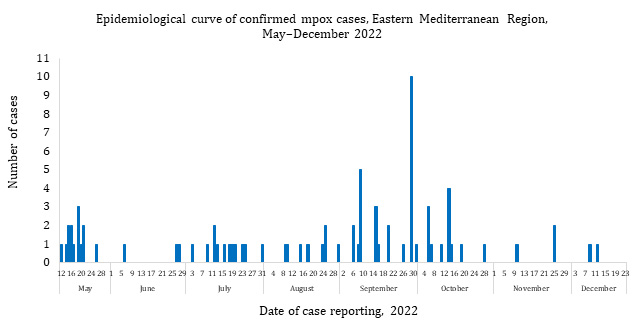 Fig. 36. Epidemiological curve of confirmed mpox cases, Eastern Mediterranean Region, May–December 2022
Fig. 36. Epidemiological curve of confirmed mpox cases, Eastern Mediterranean Region, May–December 2022
WHO support for countries affected by the mpox outbreak spanned all response pillars, including active surveillance of cases, contact tracing, provision of diagnostic kits to laboratories in the countries, technical and logistical support for case management, risk communication and community engagement (RCCE), and the updating and dissemination of technical guidelines and protocols.
WHO also worked closely with civil society in the outbreak-affected countries, as well as with the Islamic Advisory Group, to enhance preventive measures, case reporting and response in the affected countries.
Following publication of the WHO clinical management guidelines, a regional webinar (30 June 2022) and country-adapted case management training (July 2022) were developed and conducted. Context-specific information, education and communication materials on mpox were developed (in English and Arabic) and disseminated through various media platforms to enhance knowledge and promote healthy practices.
WHO also supported the development of outbreak response plans in the affected countries. Also, a joint Gulf Cooperation Council (GCC) and WHO risk assessment workshop was conducted on 9 and 10 October 2022 in Saudi Arabia. The main goal of this workshop was to review the current situation, assess the risk of mpox transmission in the Gulf region and develop region-specific recommendations to enhance mpox outbreak preparedness and response measures.
10. Poliomyelitis (polio)
In 2022, the Eastern Mediterranean Region reported 22 cases of wild poliovirus type 1 (WPV1) in Afghanistan (2) and Pakistan (20), as well as 57 WPV1-positive environmental samples (20 in Afghanistan and 37 in Pakistan).
As for circulating vaccine-derived poliovirus type 2 (cVDPV2), a total of 164 confirmed cases were detected in 2022, in Somalia (4), Sudan (1) and Yemen (159). In addition, 32 cVDPV2 environmental isolates were detected, in Djibouti (12), Egypt (6), Somalia (3), Sudan (1) and Yemen (10). No confirmed cases of circulating vaccine-derived poliovirus type 1 (cVDPV1) were reported in 2022.
All countries remain at risk of polio until the disease has been completely eradicated from the world. In 2021, the Global Polio Eradication Initiative launched the “Polio Eradication Strategy 2022–2026: Delivering on a promise”, which updates the previous strategy and aims to address emerging challenges.
The new strategy establishes 2 goals: the first is to interrupt wild poliovirus transmission in endemic countries; the second is to stop cVDPV transmission and prevent outbreaks in non-endemic countries. The strategy aims to achieve and sustain a polio-free world through a focus on implementation and accountability to reduce outbreak response times, increase vaccine demand, transform campaign effectiveness, expedite progress through expanded integration efforts, increase access in inaccessible areas, transition towards government ownership, and improve decision-making and accountability.
In 2022, WHO and the United Nations Children’s Fund (UNICEF) supported vaccination campaigns in the last 2 polio-endemic countries in the world , namely Afghanistan and Pakistan.
11. Coronavirus disease 2019 (COVID-19)
On 29 January 2020, the WHO Eastern Mediterranean Region reported the detection of its first COVID-19 cases.
COVID-19 continued to spread at the regional and global levels in 2022. By 31 December 2022, the global cumulative incidence had reached 651 922 986 reported cases and 6 669 794 associated deaths, giving a case fatality ratio (CFR) of 1.02%. By the same date, the 22 countries and territories of the Eastern Mediterranean Region had reported a total of 23 221 923 cases, representing about 3.56% of the global count, with 349 081 associated deaths (CFR: 1.5%).
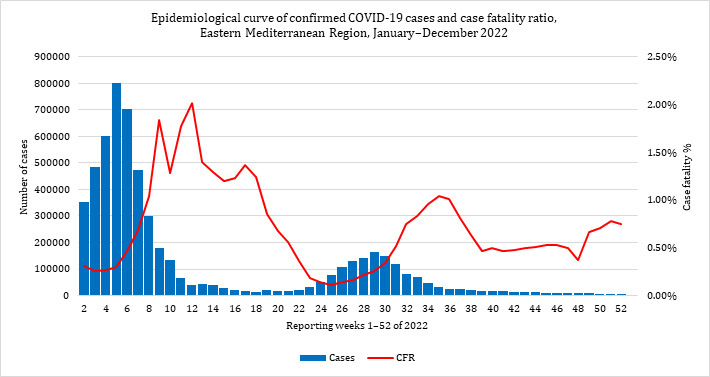 Fig. 37. Epidemiological curve of monthly confirmed COVID-19 cases and case fatality ratio (%), Eastern Mediterranean Region, January–December 2022
Fig. 37. Epidemiological curve of monthly confirmed COVID-19 cases and case fatality ratio (%), Eastern Mediterranean Region, January–December 2022
Most countries of the Region are in the community transmission phase. From the start of the outbreak to the end of 2022, the country that reported the highest number of cases in the Region was the Islamic Republic of Iran (7 561 140 cases; 32.56% of the Region’s total), followed by Iraq (2 464 997 cases; 10.62%) and Jordan (1 746 997 cases; 7.52%). Over the same period, the Islamic Republic of Iran also reported the highest number of COVID-19-associated deaths (144 685 deaths; CFR: 1.91%), followed by Pakistan (30 635 deaths; CFR: 1.94%) and Tunisia (29 284 deaths; CFR: 2.55%). The highest CFRs for this period were reported by Yemen (18.07%), followed by Sudan (7.84%) and Syria (5.51%), while the lowest CFRs were reported by the United Arab Emirates (0.22%), Bahrain (0.22%) and Qatar (0.14%).
In terms of testing, a total of 442 303 054 laboratory tests were conducted across the Region from the start of the outbreak to end December 2022. This includes 213 199 tests in week 52 of 2022, a 12% decrease compared with the previous week, when 241 837 tests were conducted. The highest number of polymerase chain reaction (PCR) tests were reported from the United Arab Emirates (197 950 426), followed by the Islamic Republic of Iran (54 738 231) and Saudi Arabia (44 940 564). The average positivity rate for the Region over this period was 5.25%. WHO recommends a positivity rate of about 3–12% as a general benchmark indicating adequate testing, which was achieved in most countries of the Region.
COVID-19 vaccination continued across the Region in 2022. A total of 844 957 683 doses had been administered across the 22 countries and territories to end December 2022. By that date, Pakistan had administered the highest number of COVID-19 vaccine doses (317 080 887), followed by the Islamic Republic of Iran (154 773 070) and Egypt (100 993 230). At the other end of the scale, the lowest numbers of doses of COVID-19 vaccine in the Region had been administered by Bahrain (3 476 633), Yemen (1 238 962) and Djibouti (338 051).
Table 4. Number of COVID-19 cases and deaths per million population, Eastern Mediterranean Region, as at 31 December 2022
|
Country/territory |
Cases |
Deaths |
Population |
Cases per million pop’n |
Deaths per million pop’n |
|
Afghanistan |
207 585 |
7849 |
39 835 428 |
5211.1 |
197 |
|
Bahrain |
696 614 |
1536 |
1 748 295 |
398 453.4 |
878.6 |
|
Djibouti |
15 690 |
189 |
1 002 197 |
15 655.6 |
188.6 |
|
Egypt |
515 533 |
24 802 |
104 258 327 |
4944.8 |
237.9 |
|
Iran (Islamic Republic of) |
7 561 140 |
144 685 |
85 028 760 |
88 924.5 |
1701.6 |
|
Iraq |
2 465 545 |
25 375 |
41 179 351 |
59 873.3 |
616.2 |
|
Jordan |
1 746 997 |
14 122 |
10 269 022 |
170 123 |
1375.2 |
|
Kuwait |
662 747 |
2570 |
4 328 553 |
153 110.5 |
593.7 |
|
Lebanon |
1 222 808 |
10 747 |
6 769 151 |
180 644.2 |
1587.6 |
|
Libya |
507 142 |
6437 |
6 958 538 |
72 880.5 |
925.1 |
|
Morocco |
1 271 595 |
16 294 |
37 344 787 |
34 050.1 |
436.3 |
|
Occupied Palestinian territory |
703 228 |
5708 |
5 222 756 |
134 646.9 |
1092.9 |
|
Oman |
399 154 |
4628 |
5 223 376 |
76 416.9 |
886 |
|
Pakistan |
1 575 805 |
30 636 |
225 199 929 |
6997.4 |
136 |
|
Qatar |
489 428 |
685 |
2 930 524 |
167 010.4 |
233.7 |
|
Saudi Arabia |
827 004 |
9518 |
35 340 680 |
23 400.9 |
269.3 |
|
Somalia |
27 310 |
1361 |
16 359 500 |
1669.4 |
83.2 |
|
Sudan |
63 686 |
4994 |
44 909 351 |
1418.1 |
111.2 |
|
Syria |
57 423 |
3163 |
18 275 704 |
3142 |
173.1 |
|
Tunisia |
1 147 645 |
29 285 |
11 935 764 |
96 151.8 |
2453.6 |
|
United Arab Emirates |
1 047 008 |
2348 |
9 991 083 |
104 794.2 |
235 |
|
Yemen |
11 945 |
2159 |
30 490 639 |
391.8 |
70.8 |
|
Total |
23 223 032 |
349 091 |
744 601 715 |
31 188.5 |
468.8 |
Table 5. Reported disease outbreaks in the WHO Eastern Mediterranean Region, 2022
|
Country |
Disease |
Cases |
Deaths |
Case fatality ratio (%) |
Event date |
|
Afghanistan |
Acute watery diarrhoea |
242 562 |
87 |
0.04 |
|
|
Iraq |
Cholera |
11 097 |
24 |
0.22 |
Jun-2022 |
|
Iran (Islamic Republic of) |
Cholera |
367 |
7 |
1.91 |
Jul-2022 |
|
Lebanon |
Cholera |
5422 |
23 |
0.42 |
Oct-2022 |
|
Pakistan |
Cholera |
1002 |
43 |
- |
Jan-2022 |
|
Somalia |
Cholera |
15 633 |
88 |
0.56 |
Jan-2022 |
|
Syria |
Cholera |
70 220 |
102 |
0.15 |
Sep-2022 |
|
Yemen |
Cholera |
21 178 |
21 |
0.10 |
Jan-2022 |
|
Afghanistan |
Circulating vaccine-derived poliovirus type 2 (cVDPV2) |
43 |
0 |
0 |
Jan-2021 |
|
Pakistan |
cVDPV2 |
8 |
0 |
0 |
Jan-2021 |
|
Somalia |
cVDPV2 |
5 |
– |
– |
Jan-2022 |
|
Sudan |
cVDPV2 |
1 |
– |
– |
Sep-2022 |
|
Yemen |
cVDPV2 |
159 |
– |
– |
Jan-2022 |
|
Afghanistan |
Crimean-Congo haemorrhagic fever (CCHF) |
389 |
15 |
3.86 |
Jan-2022 |
|
Iraq |
CCHF |
1370 |
114 |
8.32 |
Apr-2022 |
|
Afghanistan |
Dengue |
1266 |
2 |
0.16 |
Jun-2022 |
|
Oman |
Dengue |
579 |
0 |
– |
Mar-2022 |
|
Pakistan |
Dengue |
62 995 |
62 |
0.10 |
Sep-2022 |
|
Somalia |
Dengue |
5350 |
18 |
0.34 |
Sep-2022 |
|
Sudan |
Dengue |
5264 |
37 |
0.70 |
Jan-2022 |
|
Yemen |
Dengue |
24 978 |
45 |
0.18 |
Jan-2022 |
|
Lebanon |
Diphtheria |
34 |
0 |
0 |
Jan-2022 |
|
Pakistan |
Diphtheria |
351 |
46 |
13.1 |
Jan-2022 |
|
Lebanon |
Hepatitis A |
600 |
0 |
0 |
Jan-2022 |
|
Sudan |
Hepatitis E |
2576 |
24 |
0.01 |
Jun-2022 |
|
Occupation of Palestinian territory |
Hepatitis of Unknown origin |
2 |
0 |
0 |
Jan-2022 |
|
Qatar |
Hepatitis of Unknown origin |
2 |
0 |
0 |
Jan-2022 |
|
Pakistan |
HIV |
192 |
2 |
1.04 |
Jun-2022 |
|
Morocco |
legionnaires |
3 |
0 |
0 |
Jun-2022 |
|
Pakistan |
Leishmaniasis |
8000 |
0 |
0 |
Mar-2022 |
|
Djibouti |
Malaria |
40 648 |
– |
– |
Jan-2022 |
|
Iran (Islamic Republic of) |
Malaria |
4425 |
– |
– |
Jan-2022 |
|
Pakistan |
Malaria |
937 906 |
– |
– |
Sep-2022 |
|
Sudan |
Malaria |
2 624 002 |
262 |
0.01 |
Jan-2022 |
|
Afghanistan |
Measles |
77 210 |
388 |
0.50 |
Jun-2022 |
|
Djibouti |
Measles |
209 |
0 |
0.00 |
Jun-2022 |
|
Iran (Islamic Republic of) |
Measles |
10 620 |
0 |
0.00 |
Jan-2022 |
|
Pakistan |
Measles |
17 737 |
117 |
0.66 |
Jan-2022 |
|
Somalia |
Measles |
17 361 |
0 |
0.0 |
Mar-2022 |
|
Sudan |
Measles |
3310 |
4 |
0.12 |
Jan-2022 |
|
Syria |
Measles |
6309 |
2 |
0.04 |
Jan-2022 |
|
Yemen |
Measles |
10 979 |
77 |
0.70 |
Mar-2022 |
|
Syria |
Meningitis |
1573 |
2 |
0.01 |
May-2022 |
|
Oman |
Middle East respiratory syndrome (MERS) |
1 |
0 |
0.00 |
Apr-2022 |
|
Qatar |
MERS |
2 |
0 |
0.00 |
Mar-2022 |
|
Saudi Arabia |
MERS |
5 |
0 |
0.00 |
Apr-2022 |
|
Bahrain |
Mpox (monkeypox) |
1 |
0 |
0.00 |
Sep-2022 |
|
Egypt |
Mpox |
3 |
0 |
0.00 |
Sep-2022 |
|
Iran (Islamic Republic of) |
Mpox |
1 |
0 |
0.00 |
Aug-2022 |
|
Jordan |
Mpox |
1 |
0 |
0.00 |
Sep-2022 |
|
Lebanon |
Mpox |
24 |
0 |
0.00 |
Jun-2022 |
|
Morocco |
Mpox |
3 |
0 |
0.00 |
Jun-2022 |
|
Qatar |
Mpox |
5 |
0 |
0.00 |
Jul-2022 |
|
Saudi Arabia |
Mpox |
8 |
0 |
0.00 |
Jul-2022 |
|
Sudan |
Mpox |
18 |
1 |
5.56 |
Aug-2022 |
|
United Arab Emirates |
Mpox |
16 |
0 |
0.00 |
May-2022 |
|
Afghanistan |
Pertussis |
993 |
15 |
1.51 |
Jan-2022 |
|
Afghanistan |
Poliomyelitis (polio) |
2 |
– |
– |
Jan-2022 |
|
Pakistan |
Polio |
20 |
– |
– |
Apr-2022 |
|
Syria |
Respiratory illness |
165 |
26 |
15.76 |
Dec-2022 |
|
Tunisia |
Shigellosis |
100 |
1 |
1 |
Jul-2022 |


