Background
In 2021, the World Health Organization (WHO)’s Eastern Mediterranean Region continued to witness the ongoing coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). By the end of the year more than 12 million cases were reported cumulatively, including 194 245 associated deaths from all 22 countries of the Region, revealing a case-fatality ratio (CFR) of 1.8%.
Furthermore, 31 major outbreaks due to emerging infectious diseases occurred in 11 countries of the Region including acute watery diarrhoea in Afghanistan, cholera in Somalia and Yemen, Crimean-Congo haemorrhagic fever in Afghanistan, Iraq and Pakistan, dengue in Afghanistan, Pakistan, Sudan and Yemen, diphtheria in Sudan and Yemen, extensively drug-resistant (XDR) typhoid fever in Pakistan, hepatitis E virus in Sudan, measles in Afghanistan, Somalia and Syria, and wild polio virus in Afghanistan and Pakistan. Seven countries had continuing outbreaks of circulating vaccine-derived poliovirus type 2 (VDPV2) during 2021, including Afghanistan, Djibouti, Egypt, Pakistan, Somalia, Sudan, and Yemen (combined cVDPV1 and cVDPV2). 17 sporadic MERS cases were reported from Saudi Arabia and United Arab Emirates (15 and 2, respectively). More than 398 140 reported cases and more than 682 associated deaths resulted from these 28 outbreaks, which were monitored while technical, management and logistical support was provided to detect, confirm, and respond to these outbreaks (Fig. 1).
 The Regional Office continues providing technical support to affected countries to contain the outbreaksThe WHO Regional Office for the Eastern Mediterranean continued to provide technical support to affected countries to contain the outbreaks, prevent geographical spread and mitigate their impact through application of appropriate public health interventions using evidence-based control measures. The likelihood of the emergence and rapid transmission of high-threat pathogen diseases has increased in recent time, as there are many countries affected directly or indirectly by acute or protracted humanitarian emergencies, which have led to a fragile health systems with poor health service provision; and unusually high numbers of internally displaced persons (IDPs) and refugees living in overcrowded, overburdened spaces, with little or no access to basic health care services and environmental infrastructure. The other risk factors contributing to the emergence and rapid spread of epidemic diseases in the Region include rapid or unplanned urbanization, climate change, increased human–animal interaction, and health system constraints, such as weak infectious disease surveillance and limited laboratory diagnostic capacities.
The Regional Office continues providing technical support to affected countries to contain the outbreaksThe WHO Regional Office for the Eastern Mediterranean continued to provide technical support to affected countries to contain the outbreaks, prevent geographical spread and mitigate their impact through application of appropriate public health interventions using evidence-based control measures. The likelihood of the emergence and rapid transmission of high-threat pathogen diseases has increased in recent time, as there are many countries affected directly or indirectly by acute or protracted humanitarian emergencies, which have led to a fragile health systems with poor health service provision; and unusually high numbers of internally displaced persons (IDPs) and refugees living in overcrowded, overburdened spaces, with little or no access to basic health care services and environmental infrastructure. The other risk factors contributing to the emergence and rapid spread of epidemic diseases in the Region include rapid or unplanned urbanization, climate change, increased human–animal interaction, and health system constraints, such as weak infectious disease surveillance and limited laboratory diagnostic capacities.
The WHO Health Emergencies Programme in the Region works on the prevention, preparedness, detection and response to high-threat pathogens and other public health hazards and emergencies. While these areas of work remain a top priority for WHE, available resources especially in national ministries of health, were repurposed in order to boost the COVID-19 pandemic response and minimize the impact of the pandemic on societies and economies.
In response to the second goal of WHO's Thirteenth General Programme of Work (GPW13) to make “one billion more people better protected from health emergencies”, and its second programme budget outcome of “epidemics and pandemics prevented”, the Infectious Hazard Prevention and Preparedness (IHP) programme within WHE continued to provide technical support to affected countries to prevent or contain outbreaks through the application of proven and appropriate evidence-based public health control measures for priority pandemic- or epidemic-prone diseases.
IHP maintains disease-specific epidemiological data received from country offices and ministries of health on major disease outbreaks through its central database ‒ the Outbreak and Public Health Event Portal (OPHEP). This online portal is used to monitor disease outbreak trends in the Region and the progress of response measures.
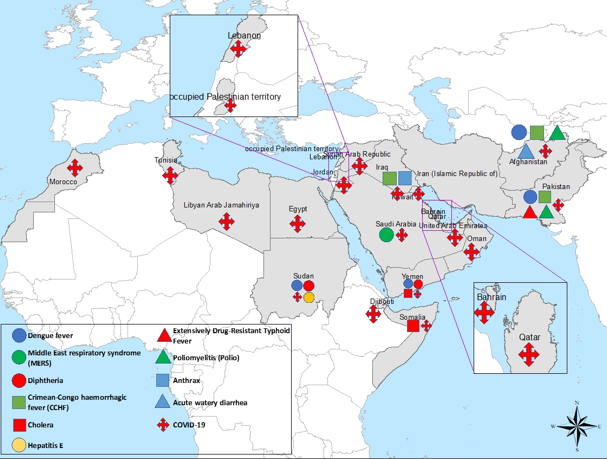
Fig. 1. Countries of WHO’s Eastern Mediterranean Region reporting infectious disease outbreaks in 2021
Challenges
WHO and other partners have faced multiple challenges in the provision of technical support to countries to improve their capacities to respond to these emerging and re-emerging infectious disease outbreaks. Most significantly, the majority of outbreak-affected countries were experiencing acute or protracted emergencies with disrupted or under-performing health systems, such as in Libya, Somalia, Sudan, Syria and Yemen. In other countries, such as Afghanistan and Pakistan, financial and capacity issues impacted the performance of their health systems.
 The high frequency of natural disasters was a major challenge in increasing the number of outbreaksProlonged insecurity and inaccessibility in countries with complex emergencies (such as Iraq, Somalia, Syria and Yemen) usually resulted in the delayed implementation of key planned activities and the under-utilization of committed resources, potentially leading to the rapid spread of high-threat pathogens to other areas. The high frequency of natural disasters (such as floods, droughts and heavy rains) was another major challenge, aggravating the existing situation and increasing the number of outbreaks. With persistent demand from countries for greater technical, logistical and financial support to tackle the outbreaks, it was sometimes difficult to find the required funding, technical staff and supplies. Many countries in the Region are lacking necessary political commitment and investment to improve preparedness, prevention and mitigation in the event of a major disease outbreak or pandemic.
The high frequency of natural disasters was a major challenge in increasing the number of outbreaksProlonged insecurity and inaccessibility in countries with complex emergencies (such as Iraq, Somalia, Syria and Yemen) usually resulted in the delayed implementation of key planned activities and the under-utilization of committed resources, potentially leading to the rapid spread of high-threat pathogens to other areas. The high frequency of natural disasters (such as floods, droughts and heavy rains) was another major challenge, aggravating the existing situation and increasing the number of outbreaks. With persistent demand from countries for greater technical, logistical and financial support to tackle the outbreaks, it was sometimes difficult to find the required funding, technical staff and supplies. Many countries in the Region are lacking necessary political commitment and investment to improve preparedness, prevention and mitigation in the event of a major disease outbreak or pandemic.
The COVID-19 pandemic has not spared the Eastern Mediterranean Region, with a rapid growth in the number of people infected with the new coronavirus SARS-CoV-2 in 2021. The impact has been the overburdening of health care systems, loss of life and livelihoods, as well as costly repurposing of health care services and capacities to address the growing pandemic. While vaccination efforts continue to grow, COVID-19 still poses a significant threat to regional economies and health systems, while particularly affecting the most vulnerable members of society.
Another challenge has been the lack of integrated response plans within affected countries, and this can lead to fragmented response efforts to contain outbreaks. Some outbreaks required the involvement of multiple ministries for infrastructure development (such as clean water supply, sanitation and disaster preparedness) and improvement of preparedness and response capacities. The lack of public awareness on preventative measures against common infectious diseases, such as cholera and vector-borne diseases, contributed to the rapid spread of these outbreaks.
Recommendations
Governments and all stakeholders should allow local partners and donor organizations to access emergency-affected areas and provide essential health services.
Ensure continuous engagement with external partners and donors to build trust, encourage the pooling of resources and help build consensus on division of responsibilities, thus avoiding wastage and duplication of efforts and resources. Local partners should be engaged to provide logistical support within country, if WHO is not present.
Comprehensive joint preparedness and response strategies should be developed through coordination between governments and external partners to enable a coordinated response and the pooling of resources. Countries facing multiple vector-related outbreaks should develop integrated plans for optimal use of resources and simultaneous control. Countries facing repeated waterborne outbreaks should update or develop comprehensive national cholera control plans aligned with “Ending cholera: a global roadmap to 2030”.
Regular evaluations (external, internal and joint) should be conducted to assess the impact of response activities and identify and address gaps. Prioritization of issues should be based on threat perception and sensitivity, with resources allocated accordingly. New efficient tools should be developed and adapted for capacity-building in case diagnosis, investigation and prevention.
The COVID-19 response should be reinforced at the regional, national, subnational, and community levels, particularly by strengthening existing partnerships and multisectoral collaboration, addressing misinformation, improving surveillance and reporting, encouraging research, innovation, and information-sharing, maintaining essential health services, and building capacity in infection prevention and control.
Public health laboratory capacities should continue to expand across the Region for all infectious disease pathogens, and to test for SARS-CoV-2 and sequence the virus.
Social mobilization and risk communication efforts for adherence to public health and social measures should be improved, reinforced and maintained during outbreaks alongside the implementation of control measures such as vaccine rollouts.
Fair and equitable distribution of COVID-19 vaccines, COVID-19 diagnostic tests, therapeutics, and personal protective equipment (PPE) must be ensured.
Specific efforts are required to:
Strengthen infectious disease surveillance systems;
Improve diagnostic capacities and laboratory systems;
Strengthen infection prevention and control, especially among health care workers;
Improve clinical case management to minimize mortality;
Improve risk communications and engagement with communities;
Strengthen rapid response capabilities for more timely response and containment; and
Conduct operational research on high-threat infectious diseases to improve preparedness, particularly through studies on the burden of disease, modelling and forecasting.
Disease outbreaks responded to in 2021 by country
Acute watery diarrhoea
Afghanistan
Between 12 September and 31 December 2021, a total of 4 915 cases of acute watery diarrhoea have been reported by the surveillance system. Of these 4625 cases (94.1%) are from Kabul province (including Kabul city and Sarobi district), 231 cases (4.7%) from Kandahar, 24 cases (0.5%) from Zabul, and 35 cases (0.7%) are reported from Laghman province. Among the total reported cases 50.2% are males and 49.8% are females. Thirty-one percent of cases aged between 15 and 29 years old, while under 5 years children account for 17.3% of cases. A total of 273 specimens have been collected from cases (179 from Kabul city, 26 from Sarobi district, 19 from Nangarhar, 11 from Kapisa, 15 from Laghman, 15 from Kandahar and eight samples from Zabul provinces). To date, a total of eight deaths associated with a CFR of 0.16% have been reported (six from Kabul city and two from Sarobi district).
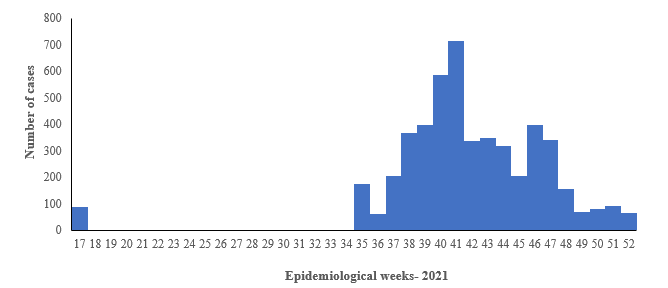
Fig 2. Number of acute watery diarrhea cases reported in, Afghanistan
WHO is providing support to the Ministry of Public Health and other line ministries to enhance disease surveillance and laboratory confirmation, map hotspots, strengthen risk communication and community engagement, promote vaccination, enhance coordination for water, sanitation and hygiene (WASH) activities and share guidelines for case management to reduce morbidity and mortality from disease.

Fig. 3. Geographical distribution of acute watery diarrhoea cases reported in 2021, Afghanistan
Cholera
Somalia
Cholera is a disease endemic to Somalia. Since December 2017, when the first cholera cases were laboratory-confirmed in Beletweyne district of the Hiraan region following heavy rains, the outbreak spread to 27 districts in four regions located in the river basins of Jubba and Shabelle. The outbreak has continued since then. The failure of the deyr (October to December 2021) rainfall season has intensified severe drought which affected over 3.2 million people in 66 out of the 74 districts, of whom 245 000 are internally displaced. Lack of access to clean and sufficient water and hygiene services, are reportedly on the rise, as the drought worsens, and more people are displaced into congested settlements. During 2021 (January to December), a total of 4577 suspected cholera cases, including 36 associated deaths, were reported (CFR = 0.8%). Most of the reported cases were from the Banadir region. From December 2017 to November 2021, a total of 20 875 suspected cholera cases, including 118 related deaths (CFR 0.57%), were reported from eight regions, namely Banadir, Bay, Bari, Gedo, Hiran, Lower Jubba, Middle Shabelle and Lower Shabelle. The districts with the highest cumulative number of cases are Daynile (2706, 12.9%), Madina (2572, 12.3%) and Hodan (2521, 12.1). A total of 721 stool specimen were collected since the start of the outbreak. Of which only 235 were laboratory confirmed for Vibrio cholerae, serotype Ogawa. (Fig. 4). Fig. 6 shows the geographical distribution of suspected cholera cases reported from Somalia in 2021.
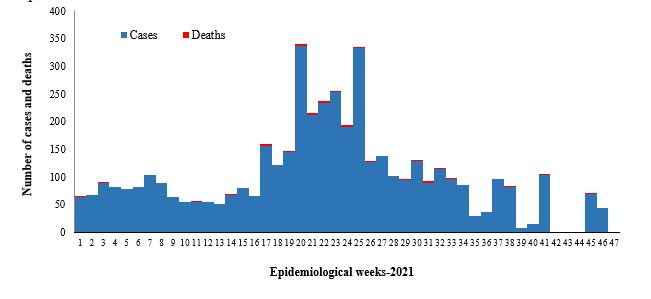
Fig. 4. Suspected cholera cases and deaths reported in Somalia, weeks 1-47, 2021
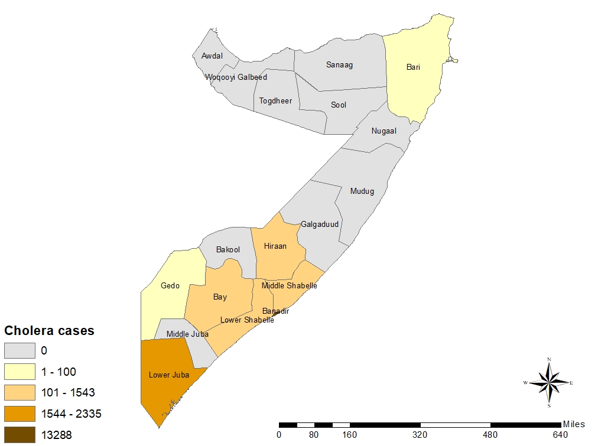
Fig. 5. Geographical distribution of suspected cholera cases reported from Somalia in 2021
WHO has continued to support the Government of Somalia since the start of the outbreak in 2017. The overall reduction in the number of new cholera cases as compared to the beginning of the outbreak is attributed to enhanced implementation of preventive interventions, including oral cholera vaccination campaigns, distribution of risk communication materials and the strengthening of WASH activities in hotspots. Disease surveillance is being managed with the support of WHO through an electronic system known as the Early Warning Alert and Response Network (EWARN). WHO and the Ministry of Health continuously monitored outbreak trends through EWARN to promptly investigate and respond to all alerts.
Yemen
The cholera outbreak reported in Yemen since October 2016 continued to affect the entire country in 2021. Although the trend was on the increase at the beginning of the year with the number of cases continuing to be reported at a steadily declining pattern level until week 11, after that a slight increase was observed in week 12 and then started declining until week 16-2021. The cumulative number of suspected cholera cases reported from January to December in 2021 was 48546 with 16 associated deaths (CFR = 0.06%). During 2021, a total of 151 stool specimens were tested. Out of these, 27 were laboratory confirmed for Vibrio cholerae. The results are pending for few of the samples. (Fig. 6). Fig. 7 shows the geographical distribution of suspected cholera cases reported from Yemen in 2021.
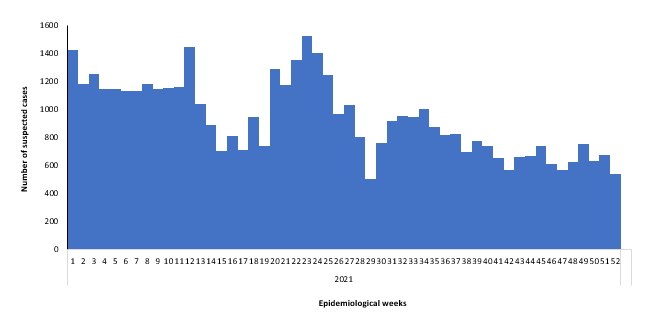
Fig. 6. Suspected cholera cases reported in northern governorate, Yemen, 2021
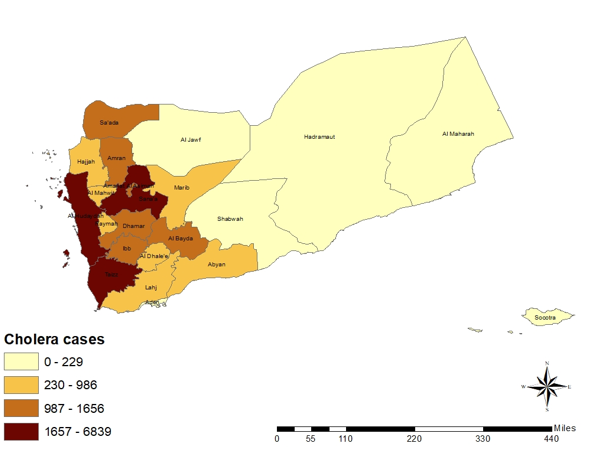
Fig. 7. Geographical distribution of suspected cholera cases reported from Yemen in 2021
The health system in Yemen has been severely weakened as a result of the ongoing conflict. WHO is supporting the Ministry of Public Health and Population in multiple ways, including enhancing disease surveillance through EWARN, providing rapid diagnostic and laboratory testing kits, mapping hotspot areas, implementing WASH activities, administering oral cholera vaccines to high-risk populations, providing supportive medicines and conducting case management training.
In 2021 support was also provided for cholera case management, laboratory investigation, oral cholera vaccination campaigns and upgrading electronic Disease Early Warning System (eDEWS) surveillance. However, the outbreak has still not been well contained due to the complexity of the situation, including lack of infrastructure, limited resources and inadequate staffing.
Crimean-Congo haemorrhagic fever
Afghanistan
Crimean-Congo haemorrhagic fever is endemic to Afghanistan, with an upsurge in cases reported in 2018 and continuing to report till the end of 2021. From January to December 2021, a total of 87 which shows a 47% decrease in number of suspected cases reported in 2020 (184). Similarly, a 33% decrease has also been observed in the reported associated deaths as in 2021 a total of five deaths (CFR 5.7%) has been reported and during 2020 a total of 15 associated deaths were reported in the country. The number of reported cases peaked in week 30-2021 (Fig. 8). Most of the cases were reported from Herat (36% of the reported cases) and Kabul (23%) provinces (Fig. 9).
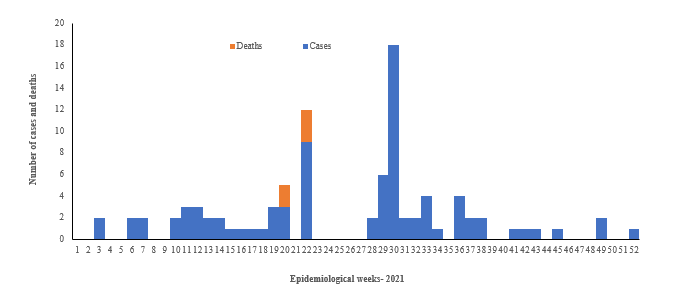
Fig. 8. Crimean-Congo haemorrhagic fever cases and deaths reported from Afghanistan, weeks 1-52, 2021
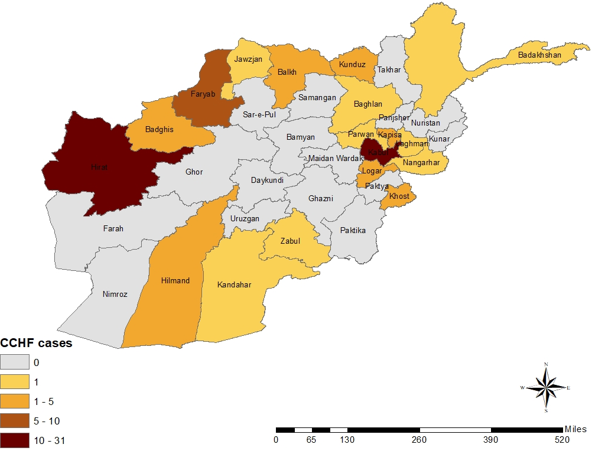
Fig. 9. Geographical distribution of Crimean-Congo haemorrhagic fever cases reported from Afghanistan in 2021
WHO continued to support the Ministry of Public Health of Afghanistan to strengthen multisectoral coordination and ensure the integration of outbreak response and control interventions. The frequency of reporting was increased to daily reporting to enhance surveillance, and health awareness was raised by targeting high-risk areas through the sharing of information, education and communication materials. The capacities of rapid response teams in outbreak response were built with a focus on Crimean-Congo haemorrhagic fever. Operational plans to accelerate the response were developed.
Pakistan
Crimean-Congo haemorrhagic fever also remains endemic to Pakistan, where the country has experienced a number of outbreaks during the last few years. Initially, cases were reported from its established foci, such as Balochistan, but other provinces and areas are currently reporting as well. The frequent unmonitored movement of animals and animal products remains the major cause of the spread of the virus throughout the country. In 2021, a total of 28 confirmed cases were reported (Fig. 10).
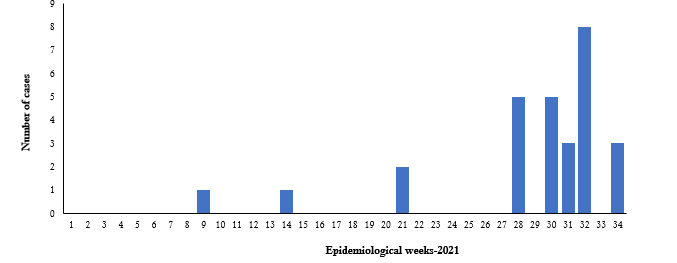
Fig. 10. Laboratory-confirmed cases of Crimean-Congo haemorrhagic fever in 2021, Pakistan
WHO extended support to Pakistan to enhance coordination in detecting Crimean-Congo haemorrhagic fever, as well as building laboratory capacity to confirm suspected cases. Laboratory kits and training were provided to the central public health laboratory. Some gaps were identified in surveillance and response measures during periodic reviews and WHO is engaged with the Government to strengthen the measures currently in place.
Iraq
Crimean-Congo haemorrhagic fever is endemic in Iraq. It was first reported in 1979. Eight epidemics have been reported since then. In 2010, 10 suspected cases were reported with eight associated deaths (CFR 80 %). Sporadic cases have been reported since then. Cases are usually reported in summer season (July to September). Most of the cases are reported from southern governorates.
In 2021, 33 suspected cases of Crimean-Congo haemorrhagic fever were reported with 13 deaths (CFR 39%). 18 cases were laboratory confirmed by PCR (35.5% positivity) among which the CFR reached 43%. outbreak started to be reported in week 19 and peaked between week 27 and 38. Male-to-female ratio = 0.9. The most affected age group > 25-45 years, 31%. 38.4% of confirmed cases said they had history with animals. Most of the cases were reported from in Thi-qar governorate (80%). Cases were reported from Ninewa, Erbil, Baghdad, Bable, Diyala and Al Anbar.
WHO is supporting the Ministry of Health to strengthen surveillance, diagnostic capacity and outbreak response activities in terms of building rapid response team capacity and improving risk communication and community engagement. Information, education and communication materials were distributed to raise the awareness of the general public on prevention measures to reduce risks.
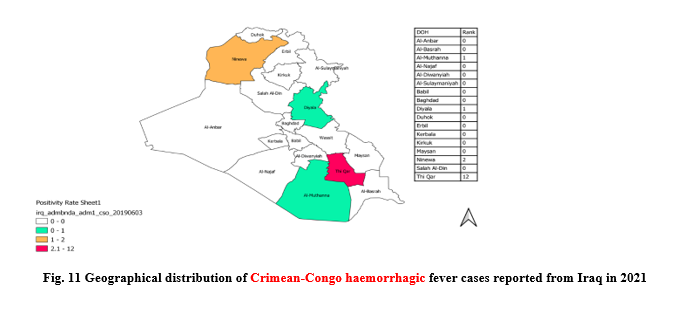
Fig. 11 Geographical distribution of Crimean-Congo haemorrhagic fever cases reported from Iraq in 2021
Dengue fever
Afghanistan
Afghanistan is endemic for vector-borne diseases such as Crimean-Congo haemorrhagic fever and malaria. Other vector-borne diseases like dengue fever and chikungunya were not reported and the presence of the vector Aedes aegypti had not been established before 2018 when, the Ministry of Public Health conducted vector surveillance and collected samples from Khost and Nangarhar provinces, which were morphologically identified as A. albopictus and A. aegypti. There have been no dengue reports by the National Disease Surveillance and Response System in Afghanistan in the past. In 2019, the national surveillance and response system in Afghanistan reported the first 15 confirmed cases of dengue.
Since 12 September 2021, Afghanistan has experienced a significant surge in suspected dengue fever cases. Between September and December 2021, a total of 761 suspected cases have been reported from 15 districts within Nangarhar province with one associated death leading to 0.13% CFR. Out of these total suspected cases, more than 90 have been confirmed by PCR from the Central Public Health Laboratory. To date only one death has been reported.
The trend of reported cases showed a peak during week 40 with 104 suspected cases of dengue fever in a single week and since then the number of reported cases has shown a continuous decline (Fig. 11). Among these reported cases males are more affected (60%), while the most affected age group is 15–29 years.
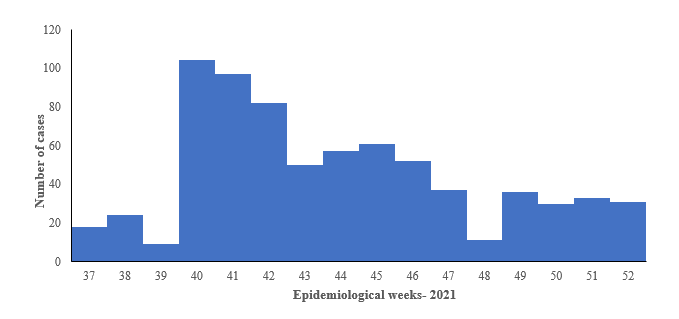
Fig. 12. Suspected dengue fever cases in 2021, Afghanistan
WHO supported the Government with the provision of case diagnosis and management guidelines throughout the country. Information, education and communication materials were distributed to raise the awareness of the general public on prevention measures to reduce risks. WHO also deployed experts for dengue surveillance, case management and vector control activities, and provided support in developing a multisectoral costed response plan.
Pakistan
Pakistan has been experiencing outbreaks of dengue fever for the past several years, affecting different parts of the country on a regular basis. The main vector of dengue virus transmission, Aedes aegypti, is well established in all parts of the country. As of January to December 2021, the total number of reported suspected dengue cases are 293 579 and the total laboratory confirmed cases are 47 439. Total number of reported deaths are 326. Among 47 439 confirmed cases, Punjab province reported the highest number of confirmed cases (n-22 007) which constitutes 46% of total cases in the country, Khyber Pakhtunkhwa reported the second highest number of dengue cases (n-10 613) at 22% of total cases in the country, Sindh reported (n-6638) 14%, Balochistan reported (n-2269) 5% confirmed cases, while ICT (Islamabad) reported (n-4219) 9% confirmed cases, AJK reported (n-1693) 4% of confirmed cases of total cases in the country.
Three hundred and twenty-six (326) deaths are reported from Pakistan in which 264 deaths (81%) with a case-fatality rate of 1.2% are reported from Punjab in which district Lahore reported 184 deaths (56.4% of the country), 28 deaths reported from Sindh, 23 deaths from Islamabad (ICT), 10 deaths from Khyber Pakhtunkhwa province and 1 death from AJK, overall the case-fatality rate of the country remains 0.7.
Cases declined after sharp raise observed from week 36 to 43, peak was observed in week 43 with total 8439 confirmed cases. In week # 51 the cases dropped to 221 after week 50 with 530 confirmed cases in the country. During week-51 Sindh province reported (n-106) confirmed cases followed by Punjab reported (n-75), Balochistan reported (n-31), Khyber Pakhtunkhwa reported (n-8), Islamabad (ICT) reported (n-1) and Azad Jammo Kashmir (AJK) reported zero cases.
Overall due to the winter season dengue transmission has declined, especially in the northern parts of the country whereas the cases transmission at Karachi and coastal districts of Balochistan the transmission is continue but at lower proportions which will continue until the last week of this year.
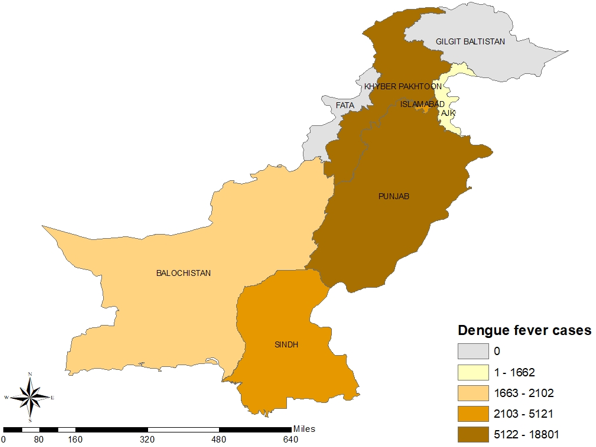
Fig. 13. Geographical distribution of confirmed dengue fever cases reported from Pakistan in 2021
WHO supported the Government with the provision of case diagnosis and management guidelines throughout the country. Information, education and communication materials were distributed to raise the awareness of the general public on prevention measures to reduce risks. WHO also deployed experts for dengue vector control activities, as well as for case management, laboratory investigation and emergency risk communication. Support was also provided to the Government through the timely arrangement of medical supplies for management of severe cases (including fluids and crystalloids).
Sudan
On 5 October 2021, the Federal Ministry of Health reported an increase in the numbers of dengue fever cases confirmed in Sudan. The first reported case was in August in a Kassala city resident who was visiting Khartoum where the illness was diagnosed. A 3-week break occurred between the first and second reported cases, following which incidence increased across central and southern states. In2021, the Federal Ministry of Health reported a total of 738 cases and four deaths (CFR 0.54%), with 153 specimens confirmed by RT-PCR at the National Public Health Laboratory. The highest number of cases were reported during week 45 where 70 cases were reported (Fig. 14). Fig. 15 shows the geographical distribution of confirmed dengue fever cases reported from Pakistan in 2021.
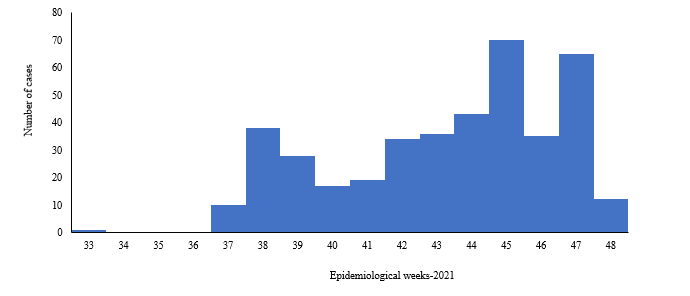
Fig. 14. Dengue fever cases reported in 2021, Sudan
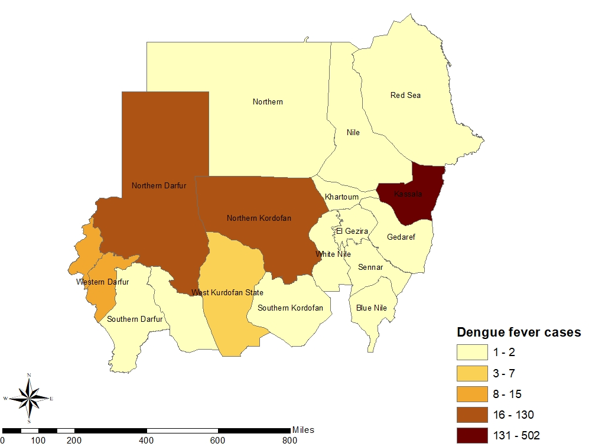
Fig. 15. Geographical distribution of confirmed dengue fever cases reported from Sudan in 2021
Regular technical and financial support is also being extended for laboratory diagnosis and confirmation, case management and vector control activities. Efforts are under way to strengthen the surveillance system for better case detection, as well as mapping hotspot areas for targeted population to control the outbreak. Collaboration is continuing with national and international partners to conduct an integrated response and for optimal utilization of resources.
Yemen
A dengue fever outbreak was reported from the Shabwah governorate of Yemen in January 2018, which continued into 2021. From epidemiological week 1-47 2021, a total of 1061 cases, including 66 deaths (CFR = 6.2%), was reported from 14 governorates. A total of 262 samples were tested and out of this total 44 were laboratory confirmed. Owing to the presence of Aedes mosquitoes in the country and other contributing factors such as heavy rains, disruption in regular water supply and underperforming health and vector control systems, a continuous reporting cases was observed during the start of 2021 until week 47. A peak in reported cases was observed during week 6 where 250 cases were reported. (Fig. 16).
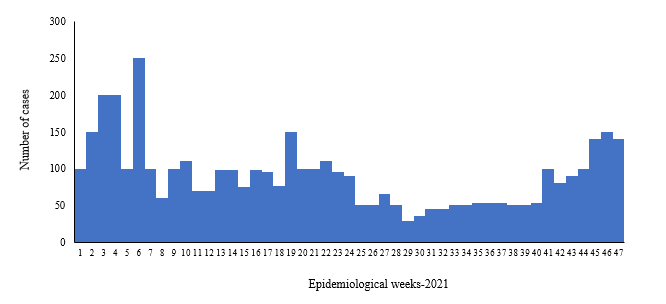
Fig. 16. Suspected dengue fever cases reported from Yemen in 2021
WHO is supporting the Government to conduct disease surveillance through the electronic Diseases Early Warning System (eDEWS) due to disruption of the routine surveillance system. Regular technical and financial support is also being extended for laboratory diagnosis and confirmation, case management and vector control activities. Efforts are under way to strengthen the surveillance system for better case detection, Collaboration is continuing with national and international partners to conduct an integrated response and for optimal utilization of resources.
Diphtheria
Sudan
On 16 February 2021, surveillance officers in South Darfur state reported five probable diphtheria cases among nomads to the expanded programme on immunization at the federal level. During the investigation of the said diphtheria alert the team found 14 probable cases and 11 deaths among children under 15 years of age reported from Buram locality with clinical manifestations similar to diphtheria. Samples were collected from three probable cases and sent to the national public health laboratory. One case was confirmed by culture on 25 February while the other two cases were confirmed by PCR test on 28 February. Through active case finding, cases were detected, tested and managed clinically. A coverage survey for 90 houses around the cases was conducted to identify the vaccination status in the affected locality (Table 1).
Table 1. Vaccination coverage survey for targeted age group, South Darfur, Sudan, 2021
|
Age group |
Not vaccinated |
Partially vaccinated |
|
< 1 year |
40 |
8 |
|
1-7 years |
96 |
9 |
|
8-15 years |
57 |
10 |
The Ministry of Health, in collaboration with WHO, conducted a limited campaign was conducted to vaccinate total of 772 children (399 with the pentavalent vaccine and 373 with the tetanus-diphtheria vaccine). A community awareness campaign on immunization was conducted to enhanced health-seeking behaviour.
Yemen
In October 2017, Yemen began experiencing an outbreak of diphtheria that spread to most districts in 23 governorates. By December 2021, a total of 7874 suspected cases were reported with 500 related deaths (CFR = 6.3%), including 700 laboratory-confirmed cases. From January to December 2021 a total of 1109 cases were reported with 67 associated deaths (CFR = 6%) (Fig. 17). The most affected age group was 5‒14 years.
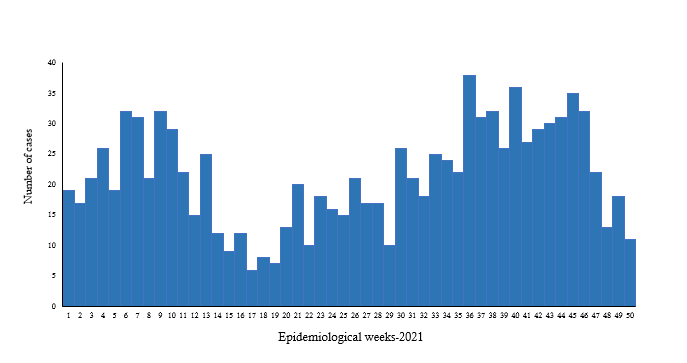
Fig. 17. Diphtheria cases reported in Yemen, 2021
WHO provided support to the local health authorities in disease surveillance and laboratory confirmation of suspected cases through the provision of logistical and technical resources. In addition to routine immunization activities, supplementary immunization campaigns were conducted to protect those people at high risk for diphtheria.
Extensively drug-resistant typhoid fever
Pakistan
Since November 2016, Pakistan has continued to report cases of extensively drug-resistant (XDR) typhoid fever after cases were first detected in the district of Hyderabad in Sindh province. Cases continued to be reported from other districts of Sindh province, with most (72%) being reported from Karachi district (Fig. 18). Up until August 2021, a total of 21 198 cases were reported from different districts of Sindh province (Table 1), of which 2348 cases were reported during 2021.
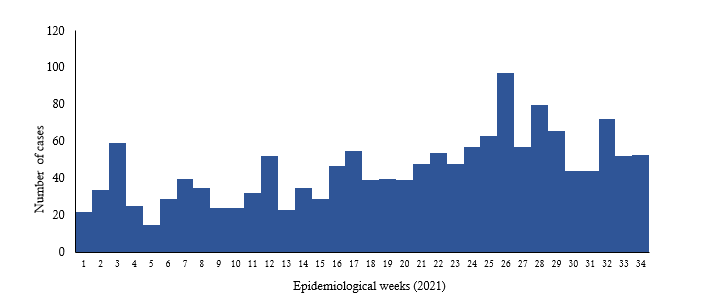
Fig. 18. Extensively drug-resistant typhoid fever cases reported in Karachi, Pakistan in 2021
|
Year |
Karachi |
Hyderabad |
Other districts |
Total |
|
2016 |
0 |
12 |
0 |
12 |
|
2017 |
175 |
485 |
4 |
664 |
|
2018 |
3712 |
891 |
207 |
4810 |
|
2019 |
7088 |
1645 |
998 |
9731 |
|
2020 |
2510 |
708 |
415 |
3633 |
|
2021 |
1792 |
375 |
181 |
2348 |
|
Total |
15277 |
4116 |
1805 |
21198 |
Table 2. Extensively drug-resistant typhoid fever cases reported from December 2016 to August 2021, Sindh, Pakistan
The number of suspected cases of XDR typhoid fever increased during each successive year (only one province, Sindh, reported cases), with the highest number reported in 2019 (9731). WHO extended support for laboratory confirmation of suspected cases and the preparation of case management guidelines for confirmed cases. Pakistan became the first country in the world to introduce the WHO-approved typhoid conjugate vaccine in its Expanded Programme on Immunization on 18 November 2020. During 2021, vaccination was carried out in Sindh (955 742) and Punjab province (1 009 108).
Hepatitis E
Sudan
Since week 22-2021, a total of 1944 hepatitis E virus cases, including 24 associated deaths reported in Sudan, with CFR: 1.23%. Of the total reported number of cases; Gedarif state represent 74.2% followed by South Darfur at 18.0% then North Darfur at 4.3%. 95.3% of Gedarif state cases reported from Ethiopian refugee camps constituted 70.7% of Sudan’s total cases. 87.5% of the total deaths reported from North Darfur state (CFR: 25.3%). In addition 62.0% of North Darfur state reported deaths were associated with pregnancy and 77% were from one health facility in Dar Al-Salam locality. (Fig. 19). Fig. 20 shows the geographical distribution of hepatitis E cases in 2021.
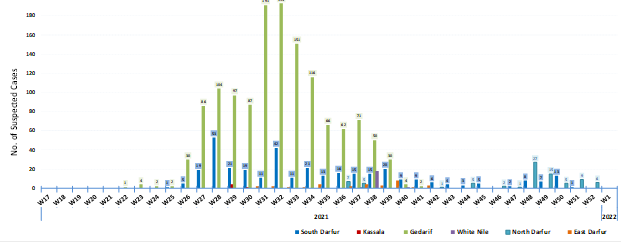
Fig. 19. Distribution of HEV suspected cases by week of reporting, Sudan 2021
WHO continues to collaborate with the Ministry and partners to support the implementation of prevention and control strategies to contain the outbreak of HEV. Response activities have focused on the application of WASH strategies. Water quality monitoring is ongoing in affected areas. Water chlorination protocols have been strengthened in all refugee and IDP sites, while hygiene promotion messaging on safe water chain, proper food handling, hand washing, drinking chlorinated water and using latrines is ongoing. Surveillance and laboratory capacities have been strengthened in all affected areas.
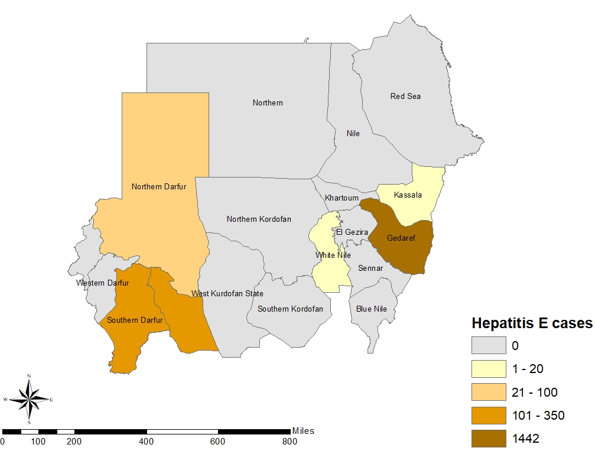
Fig. 20. Geographical distribution of the Hepatitis E cases reported from Sudan in 2021
Measles
Afghanistan
The Ministry of Public Health in Afghanistan has reported 30 199 suspected measles cases with 108 associated deaths since the beginning of year 2021 with a case-fatality ratio of 3.6%. This recent outbreak has been reported from all the provinces of the country. In total, 3362 samples were collected and out of these total 2458 were laboratory confirmed. The highest number of cases were reported during the epidemiological week 17 in which 1087 cases were reported from 34 provinces of the country. (Fig. 21). Fig. 22 shows the geographical distribution of reported cases in 2021.
A weak immunization programme in the country and inadequate surveillance due to lack of access to health services in security-compromised areas led to low population immunity against measles resulting in excessive build-up of susceptible children.
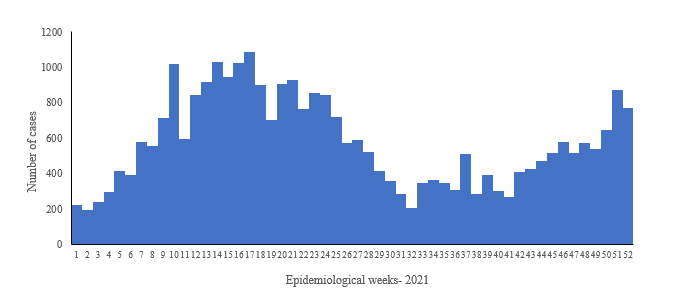
Fig. 21. Distribution of measles cases by week of reporting, Afghanistan 2021
WHO supported the Ministry of Public Health and partners in monitoring and responding to the countrywide measles outbreak. Due to the limited number of doses available hotspot mapping was conducted and six provinces were selected to be vaccinated urgently. A measles campaign was conducted during December 2021 in the six provinces namely Ghazni, Ghor, Helmand, Kandahar, Paktika and Balk. In these selected provinces 1.4 million children aged 9–59 months were vaccinated (children above 6 months were given VIT-A). This campaign was implemented using a fixed site approach (site to site/mosque to mosque) and the next nationwide measles immunization campaign will be conducted in the first quarter of 2022.
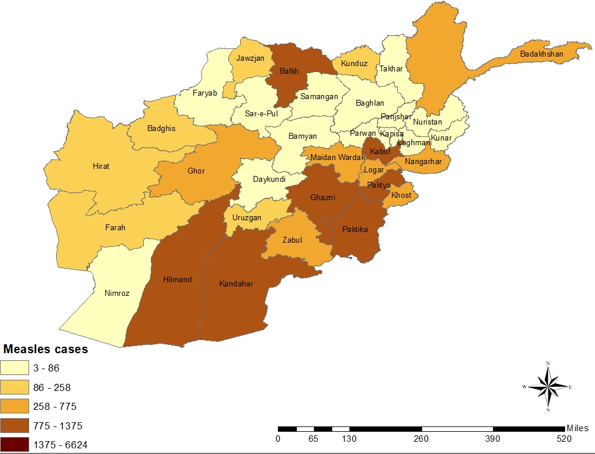
Fig. 22. Geographical distribution of the measles cases reported from Afghanistan in 2021
Somalia
Measles is endemic in Somalia with recurrent upsurge of cases. In 2021, The number of suspected cases of measles have increased in comparison to previous years (2596 in 2020, 4442 in 2019). This surge in cases is linked to a decrease in measles vaccination coverage of children below five years of age. Since epidemiological week 1 of 2021, a total of 7494 suspected cases of measles were reported from 66 drought-affected districts of whom 77.9% (3222) are children below five years. The regions reporting the most cases include Bay (2467), Banadir (2458), Lower Juba (771), Middle Shabelle (340), Hiran (338), and Mudug (292). The four measles laboratories of the country tested 1262 samples collected from affected regions in 2021. 959 samples (75.9%) were positive for measles IgM. Among confirmed cases, 82% of patients are under the age of 5 years and 52% are male.
WHO supported the Federal Ministry of Health and partners in monitoring and responding to the countrywide measles outbreak. Immunization activities to enhance measles immunization coverage were conducted. A total of 42 418 (78.5%) out of the targeted 53 239 children aged under one year received one dose of measles-containing vaccine (MCV) in drought-affected districts in October 2021. From October 2018 to October 2021, the measles vaccination coverage ranged between 58% and 84% per month compared to the national target of 95%. Essential medicine for managing the life-threatening medical condition in the drought-affected districts were distributed. WHO trained community health care workers to be deployed to cover drought-affected districts to conduct active measles case search and another epidemic disease at the lower level of the community. WHO has deployed 82 rapid response teams (3 each team with a total of 246 individuals) one in each team in the response is trained for sample handling for epidemic-prone disease cases, alert verification, sample collection and investigation.
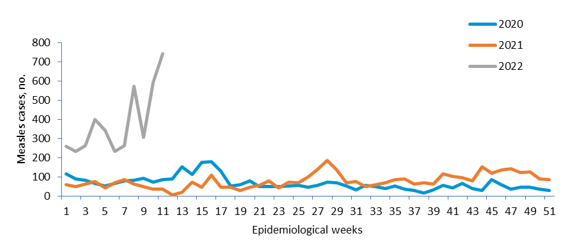
Fig. 23. Trends of measles cases reported in drought-affected districts of Somalia, 2020–2022
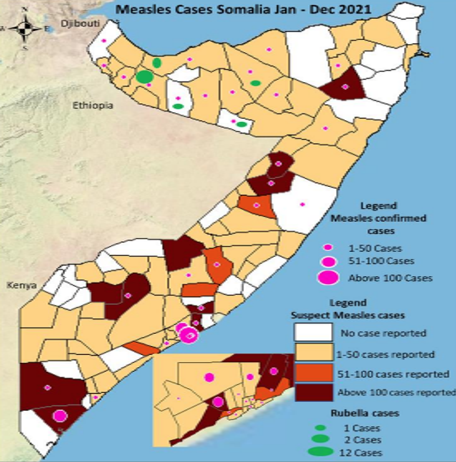
Fig. 24. Geographical distribution of the measles cases reported from Somalia in 2021
Northwest Syria
In December 2021 numbers of suspected measles cases reported to the Early Warning, Alert and Response Network (EWARN) in areas of northwest Syria accessible to WHO cross-border presence in Gaziantep, Turkey increased and continued to increase thereafter, out of the 45 suspected measles cases notified, 32 cases were investigated: three cases were discarded (negative), and 29 cases were confirmed positive: 3 epi-linked and 26 laboratory-confirmed positive for measles IgM.
In 2021, a total of 334 suspected cases of measles were notified to EWARN; 289 measles cases were reported between January and November, and 45 cases were reported in December. The highest case load was reported from Aleppo governorate with 44 suspected cases (97%) in December; with Al Bab districts being the highest affected district, 21 case (48%); Afrin 15 cases (34%), Jarabulus and Azaz 3 cases each (7%); 55% of suspected cases were below 5 years of age; female to make ratio was 1.1, 64% of the investigated cases were not vaccinated, and 3% were of unknown vaccination status.
WHO supported the outbreak response activities through regional and country office technical support to implementing and operational partners; WHO held trainings and workshops on measles and vaccine preventable diseases surveillance, case management, infection prevention and control (IPC), active case-finding, risk communication and community engagement activities, and has worked closely with actors under the health cluster to ensure provision of vitamin A capsules and implementation of a limited measles vaccination campaign in the most affected district, Al Bab, in addition to revitalization of the Surveillance, Outbreak Preparedness and Response Taskforce under the health cluster leadership. A rapid risk assessment exercise was conducted, and an measles-containing vaccine vaccination campaign targeting all of northwest Syria is being prepared for July 2022.
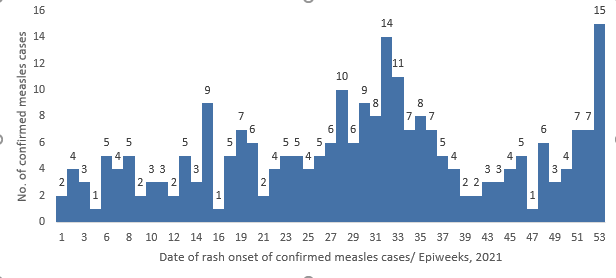
Fig. 25. Distribution of the confirmed measles cases reported from northwest Syria in 2021
Middle East respiratory syndrome (MERS)
Saudi Arabia and United Arab Emirates
MERS cases continued to be reported sporadically throughout 2021, mostly from Saudi Arabia. During this year, a total of 17 laboratory-confirmed cases were reported as compared to 61 cases in 2020, 223 in 2019, 147 in 2018 and 250 in 2017. Of the total cases reported in 2021, Saudi Arabia reported 15 cases while United Arab Emirates reported 2 cases (Fig. 26) No MERS hospital and household cluster outbreaks were reported in 2021. 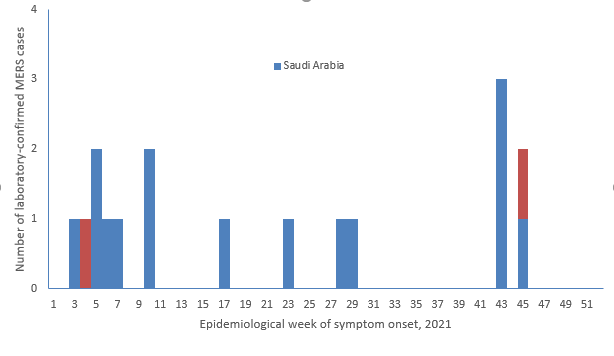
Fig. 26. MERS cases and death reported in the Region by week of symptom onset, 2021
Poliomyelitis (polio)
In 2021, the Region reported five cases of wild poliovirus type 1 (WPV1) in Afghanistan (4) and Pakistan (1), in addition to 66 WPV1 positive environmental samples (one in Afghanistan and 65 in Pakistan). For circulating vaccine derived poliovirus type 2 (cVDPV2); A total of 118 confirmed cases were detected from Afghanistan, Pakistan, Somalia and Yemen in 2021, while 104 cVDPV2 environmental isolates were also detected in Afghanistan, Djibouti, Egypt, Islamic Republic of Iran, Pakistan, Somalia and Yemen. Yemen had also confirmed 3 cases of circulating vaccine derived poliovirus type 1 (cVDPV1) as a continued outbreak from 2020. Collectively, seven countries had continuing outbreaks of cVDPV2 during 2021, including Afghanistan, Djibouti, Egypt, Pakistan, Somalia, Sudan and Yemen (combined cVDPV1 and cVDPV2); in addition to high-risk events of cVDPV2 inIslamic Republic of Iran and cVDPV3 in Palestine. Nationwide or targeted vaccination campaigns were conducted to interrupt poliovirus transmission (Fig. 27).
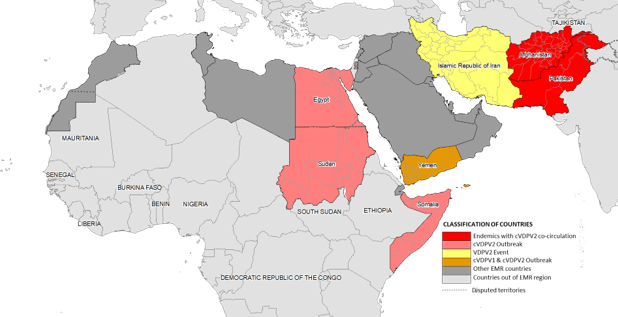
Fig. 27. Classification of countries according to the outbreaks in the Eastern Mediterranean Region, 2021
All countries remain at risk of polio until the disease has been completely eradicated from the world. In 2021, the Global Polio Eradication Initiative (GPEI) launched the Polio Eradication Strategy 2022–2026, Delivering on a Promise, a revision of the earlier strategy and aimed at addressing emerging challenges. The strategy establishes two goals: 1) to interrupt wild poliovirus transmission in endemic countries; and 2) to stop cVDPV transmission and prevent outbreaks in non-endemic countries. The strengthened plan aims to achieve and sustain a polio-free world through a focus on implementation and accountability, emphasizing cutting outbreak response times, increasing vaccine demand, transforming campaign effectiveness, working systematically through integration, increasing access in inaccessible areas, transitioning towards government ownership, and improving decision-making and accountability.
Coronavirus disease 2019 (COVID-19)
On 31 December 2019, WHO was informed of the detection of a cluster of pneumonia of unknown aetiology in Wuhan City, Hubei Province of China. A novel coronavirus (tentatively named 2019-nCoV) was identified as the causative virus on 7 January 2020. Due to its rapid proliferation in China, this new deadly pathogen posed a significant global threat and an Emergency Committee was convened by WHO’s Director General under the International Health Regulations (IHR 2005). COVID-19 was declared a Public Health Emergency of International Concern (PHEIC) on 30 January 2020.
On 29 January 2020, WHO’s Eastern Mediterranean Region reported the detection of its first 2019-nCoV cases. On 11 February 2020, WHO announced “COVID-19” as the official name of the new disease. On 11 March, WHO described the COVID-19 outbreak as a pandemic due to concerns over the geographical spread of the disease, as it already affected countries on all continents.
In 2021, countries in the Region experienced an increase in reported cases and deaths related to COVID-19. The total of 12 219 208 confirmed cases represented more than double the number reported in 2020, which stood at 4 941 451. A higher number of deaths was also reported compared to the previous year (194 245 in 2021 compared to 121 488 in 2020). However, the CFR reported was lower in 2021 (1.8%) compared to 2020 (2.5%). Two waves of the pandemic were observed in 2021 across the Region (Fig. 28). The first wave started in epi-week 5 with a gradual increase until its peak in epi-week 15 with 387 375 reported cases. A steady decline followed with the implementation of strict public health and social measures by governments. The second wave started around week 24, peaking in week 32 with 501 055 cases: the highest recorded number of cases.
Since the beginning of the outbreak, the country that has reported the highest number of total cases in the Region is the Islamic Republic of Iran (6 195 403 cases; 36% of the Region’s total), followed by Iraq (2 093 891; 12.2%) and Pakistan (1 296 527; 7.5%). The Islamic Republic of Iran also reported the highest number of COVID-19 deaths (131 639; CFR 2.1%) in the Region, followed by Pakistan (28 941; CFR 2.2%) and Tunisia (25 586; CFR 3.5%). The highest CFRs were reported by Yemen (19.6%) and Sudan (7.1%), while the lowest were reported by Qatar (0.25%), the United Arab Emirates (0.28%) and Bahrain (0.49%).
In terms of testing, 294 992 406 laboratory PCR tests have been conducted since the start of the outbreak across the Region. This includes 5 537 220 tests in week 52 of 2021, showing a 9.6% increase compared to the previous week (5 053 882 tests conducted in week 51). The United Arab Emirates reported the highest cumulative number of PCR tests conducted (111.2 million), followed by the Islamic Republic of Iran (42.1 million) and Saudi Arabia (33.3 million). The average positivity rate for the Region is 5.8%.
In terms of laboratory capacities, 15 countries reported having domestic genome sequencing capabilities to detect SARS-CoV-2 variants of concern. The other seven countries received WHO support to sequence abroad and are receiving support to strengthen local sequencing capacity using MiniOn technology.
Meanwhile, COVID-19 vaccination continues across the Region. The total number of doses administered as of 31 December 2021 in the Region’s 22 countries is 537 963 306. Pakistan has administered the highest number of doses (156 623 021), followed by the Islamic Republic of Iran (119 325 720) and Egypt (56 694 353). On the contrary, the total number of administrated doses in Djibouti has only reached 133 933, and in 659 712 in Yemen. Seven countries succeeded to vaccinate more than 40% of their target population, while five countries are still falling behind with less than 10% of target population fully vaccinated.
Since the start of the pandemic, a total of five variants of concern were reported across the Region. Among these variants, four were reported in 2021 (see Table 3). The Delta variant was mainly associated with increased disease severity while the Omicron variant showed high transmissibility. In total, 14 countries of the Region had reported the detection of the Omicron variant in 2021.
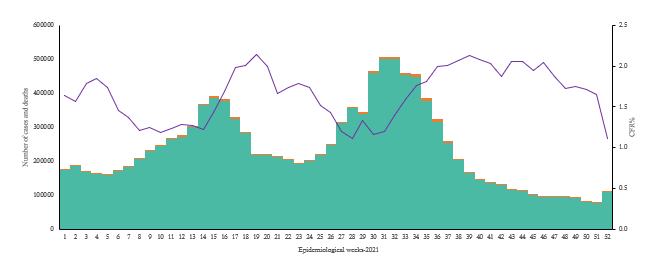
Fig. 28. Distribution of daily COVID-19 cases, deaths and CFR in the Region, epidemiological week 1-52, 2021
WHO has continued to provide support to countries through the development and dissemination of various technical guidance documents to strengthen capacities for surveillance, laboratory, clinical management, IPC and risk communication and community engagement, to improve detection and response capacities. WHO also helped procure personal protective equipment (PPE) and testing kits, conduct online training, and accelerate research and development through the solidarity trials and unity studies to help test and develop therapeutics, diagnostics and vaccines.
Nearly 2 years have passed since the first report of a COVID-19 case detected in the Region. At the time, the WHO Regional Office for the Eastern Mediterranean had activated the Incident Management Support Team (IMST) structure to support and coordinate readiness and response efforts. The IMST provided linked the headquarter-level IMST and WHO country offices for a methodical response both at the regional level and through technical support to countries in the Region. Since its establishment, the IMST has coordinated the COVID-19 response by providing strategic, operational and technical support to countries. In December 2020, the IMST structure was revised to by adding the COVID-19 vaccine pillar, to adapt to the evolving COVID-19 situation and response.
Coordination, leadership, strategic and technical guidance, surveillance, capacity-building, logistics, research, and innovation to adapt to the everchanging situation, are the main roles of the IMST. With over US$ 483 million mobilized for the regional COVID-19 response in 2020, the Regional Office had secured the highest amount of funds and had the highest utilization rate of funds received among WHO regional offices. The Dubai logistics hub had dispatched a record-breaking value of supplies in 2020 (US$ 58.9 million) in 2020, serving as the largest repository of medical equipment and supplies in the world.
Communicating effectively with WHO country offices, partners, communities and other stakeholders was an essential part of the response, including providing accurate and timely information to the general public especially regarding mask wearing, fighting the the “infodemic”, and combatting vaccine hesitancy. External communication and risk communication and community engagement were paired with regular technical guidance tailored to the regional situation. Guidance to countries included interim guidance documents, COVID-19 response review missions, training courses and webinars. In addition, the IMST developed technical tools to improve data management and analysis, including through interactive dashboards and modelling tools, to assist countries in implementing the most effective measures nationally and sub-nationally.
To strengthen its technical support to countries, the IMST deployed experts to conduct initial assessment missions in eight countries in early 2020, followed by and review missions of the COVID-19 response in four countries in late 2020: Afghanistan, Pakistan, Tunisia, and Lebanon. In 2021, three COVID-19 response review missions were conducted to Jordan, Somalia, and Saudi Arabia. The purpose of these missions was to identify and document strengths and areas for improvement while supporting ministries of health to review and assess their national COVID-19 response. In the missions, experts reviewed background documents, engaged with key stakeholders and conducted site visits. Technical and operational advice was given to stakeholders throughout, and recommendations were then made in the context of the emergency response and for longer term health system strengthening.
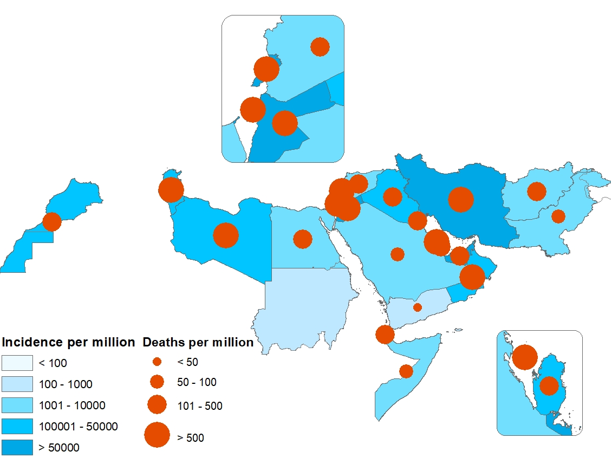
Fig. 29. Geographical distribution of COVID-19 cases and deaths per million reported from the Region, January to December 2021
Influenza activity in the Region during the COVID-19 pandemic
Influenza continues to pose a persistent threat in its epidemic and pandemic forms. In 2021, a decline in influenza activity has been seen in the Region, a trend witnessed in other parts of the world as well. However, compared to 2020, the year (2021) also saw a revival of attention towards influenza surveillance.
Before the COVID-19 pandemic, around 19 countries in the Region had functional sentinel influenza surveillance systems that were regularly reporting epidemiological and virologic data to WHO global and regional platforms. However, in 2021 only 11 countries were reporting their data for many reasons, mainly difficulties in maintaining influenza surveillance due to overwhelmed staff and/or diversion of influenza staff to respond to the COVID-19 pandemic.
In the 2020–2021 season, despite the fact that the number of enrolled patients at sentinel sites has maintained high levels as shown in Fig. 30; however, there has been a remarkable decline in the number of specimens tested for influenza (44 764 specimens out of 166 576 enrolled patients) when compared to previous seasons. This can be explained by a high volume of patients with respiratory symptoms presented at health care facilities during the COVID-19 pandemic; nonetheless, these patients were not being tested for influenza, instead health professionals have been focusing on COVID-19 diagnostics, overlooking influenza. On another note, countries in other WHO regions that maintained the systematic testing of influenza during the pandemic, still witnessed a decrease or absence of influenza activity. Hence, it is not surprising to see how a non-influenza pandemic virus, with similar mode of transmission to that of influenza viruses, can partially mitigate the spread of seasonal influenza. This decline in influenza virus activity has been observed in the Region, as well as in several WHO regions.
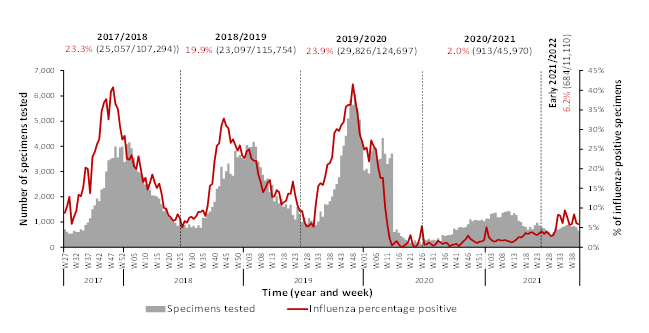
Fig. 30. Number of enrolled patients, tested specimens, and percent positive influenza specimens by analytical period, countries in the Region, from 2016 to 2017 until 2020 to 2021
Interventions against SARS-CoV2 transmission may explain to some extent the low influenza activity witnessed globally. The IPCs and NPIs measures that are being adopted to prevent the spread of COVID-19 in communities are similar to those recommended for other respiratory diseases, such as influenza, hence the decrease in influenza activity during the pandemic period.
One important point to highlight, though, is the solid infrastructure of the sentinel influenza surveillance system that played a major role in many countries of the Region in the early response to the pandemic. This infrastructure can be represented by the sentinel network being readily available for use for COVID-19 isolation and collection of specimens, trained and experienced influenza personnel (on IPC measures, specimen collection and handling, recording and reporting data), capacitated laboratories and national influenza centres in testing influenza and other viral pathogens, available influenza guidelines/SOPs, and the use of influenza pandemic preparedness plans by countries and their adoption (after a few amendments) and implementation at the beginning and throughout of the pandemic.
Table 3. Infectious disease outbreaks reported from countries of the Region in 2021
|
Disease |
Country |
First reported case |
Last reported case |
Total cases* |
Deaths |
CFR (%) |
|
Acute watery diarrhoea |
Afghanistan |
September 2021 |
December 2021 |
4915 |
8 |
0.16 |
|
Cholera |
Somalia |
January 2021 |
December 2021 |
4577 |
36 |
0.8 |
|
Yemen |
January 2021 |
April 2021 |
25 956 |
16 |
0.06 |
|
|
Crimean-Congo haemorrhagic fever |
Afghanistan |
January 2021 |
December 2021 |
87 |
5 |
5.7 |
|
Pakistan |
January 2021 |
December 2021 |
28 |
- |
|
|
|
Iraq |
May 2021 |
December 2021 |
45 |
13 |
29 |
|
|
Dengue fever |
Afghanistan |
September 2021 |
December 2021 |
761 |
1 |
0.13 |
|
Pakistan |
January 2021 |
November 2021 |
41 500 |
228 |
0.09 |
|
|
Sudan |
October 2021 |
December 2021 |
738 |
4 |
0.54 |
|
|
Yemen |
January 2021 |
November 2021 |
1061 |
66 |
6.2 |
|
|
Diphtheria |
Sudan |
February 2021 |
December 2021 |
11 |
14 |
78 |
|
Yemen |
January 2021 |
December 2021 |
7874 |
500 |
6.3 |
|
|
Pakistan |
January 2021 |
August 2021 |
1792 |
- |
- |
|
|
Hepatitis E |
Sudan |
May 2021 |
December 2021 |
1944 |
24 |
1.2 |
|
Measles |
Afghanistan |
January 2021 |
December 2021 |
30199 |
108 |
3.6 |
|
Somalia |
January 2021 |
December 2021 |
7494 |
- |
- |
|
|
Northwest Syria |
January 2021 |
December 2021 |
334 |
- |
- |
|
|
Middle East respiratory syndrome
|
Saudi Arabia |
January 2021 |
December 2021 |
10 |
3 |
30 |
|
Saudi Arabia |
January 2021 |
December 2021 |
2 |
1 |
50 |
|
|
Saudi Arabia |
January 2021 |
December 2021 |
1 |
1 |
100 |
|
|
Saudi Arabia |
January 2021 |
December 2021 |
2 |
1 |
100 |
|
|
Saudi Arabia |
January 2021 |
December 2021 |
1 |
0 |
|
|
|
United Arab Emirates |
January 2021 |
December 2021 |
01 |
- |
- |
|
|
United Arab Emirates |
January 2021 |
December 2021 |
01 |
|
|
|
|
Poliomyelitis (WPV1/cVDPV) |
Afghanistan |
January 2021 |
December 2021 |
4 |
- |
- |
|
Pakistan |
January 2021 |
December 2021 |
1 |
- |
- |
|
|
Poliomyelitis (cVDPV) |
Djibouti |
January 2021 |
December 2021 |
|
|
|
|
Egypt |
January 2021 |
December 2021 |
|
|
|
|
|
Somalia |
January 2021 |
December 2021 |
|
|
|
|
|
Sudan |
January 2021 |
December 2021 |
|
|
|
|
|
Yemen |
January 2021 |
December 2021 |
|
|
|
|
|
COVID-19 |
Afghanistan |
January 2021 |
December 2021 |
52 586 |
2211 |
4.2 |
|
Bahrain |
January 2021 |
December 2021 |
105526 |
5145 |
4.9 |
|
|
Djibouti |
January 2021 |
December 2021 |
189387 |
1042 |
0.6 |
|
|
Egypt |
January 2021 |
December 2021 |
7825 |
128 |
1.6 |
|
|
Islamic Republic of Iran |
January 2021 |
December 2021 |
247513 |
14121 |
5.7 |
|
|
Iraq |
January 2021 |
December 2021 |
4969258 |
76383 |
1.5 |
|
|
Jordan |
January 2021 |
December 2021 |
1498449 |
11345 |
0.8 |
|
|
Kuwait |
January 2021 |
December 2021 |
768911 |
8819 |
1.1 |
|
|
Lebanon |
January 2021 |
December 2021 |
266551 |
1534 |
0.6 |
|
|
Libya |
January 2021 |
December 2021 |
546427 |
7374 |
1.3 |
|
|
Morocco |
January 2021 |
December 2021 |
287990 |
4223 |
1.5 |
|
|
Occupied Palestinian territory |
January 2021 |
December 2021 |
523899 |
7461 |
1.4 |
|
|
Oman |
January 2021 |
December 2021 |
315157 |
3405 |
1.1 |
|
|
Pakistan |
January 2021 |
December 2021 |
176741 |
2617 |
1.5 |
|
|
Qatar |
January 2021 |
December 2021 |
813755 |
18757 |
2.3 |
|
|
Saudi Arabia |
January 2021 |
December 2021 |
106694 |
373 |
0.3 |
|
|
Somalia |
January 2021 |
December 2021 |
193495 |
2654 |
1.4 |
|
|
Sudan |
January 2021 |
December 2021 |
18818 |
1203 |
6.4 |
|
|
Syrian Arab Republic |
January 2021 |
December 2021 |
21258 |
1761 |
8.3 |
|
|
Tunisia |
January 2021 |
December 2021 |
38844 |
2186 |
5.6 |
|
|
United Arab Emirates |
January 2021 |
December 2021 |
587286 |
20846 |
3.5 |
|
|
Yemen |
January 2021 |
December 2021 |
554115 |
1495 |
0.3 |
*Includes both suspected and laboratory-confirmed cases


