Somalia responds swiftly to measles outbreak in Jubaland State
9 August 2020 – The health system of any country needs a surveillance system that can collect information on and detect alerts of epidemic-prone diseases. When a number of cases threatens to turn into an outbreak or epidemic, the surveillance system sounds an alarm that triggers a chain of immediate public health interventions.
Somalia's Early Warning and Alert Network (EWARN) is again proving its value as a real-time early warning disease alert system, as in June 2020, WHO was alerted to a possible measles outbreak in a camp for internally displaced people (IDPs) in Jubaland State and shared this information with the State Ministry of Health. On initial investigation, Somalia's EWARN system reported 11 cases of children with rashes and high-grade fever, typical symptoms of measles, in Kismayo.
Initial phase of outbreak response rolled out following field investigation
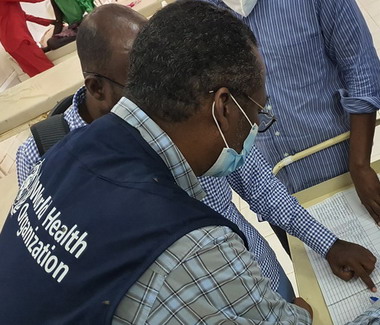
As soon as the alert was shared, a team from the WHO Somalia country office, the Ministry of Health in Kismayo, and Health Cluster1 partners took swift action to further verify and investigate the alert, confirm the diagnosis and develop an effective response plan in the event that the alert turned out to be a “true” outbreak.
Between 18 and 25 July 2020, a WHO team was deployed in Kismayo. Together with the Ministry of Health of Jubaland State and a local health partner, field investigations were carried out in the Dalhiiska IDP camp, Warshada Hargaha IDP camp, Farjano, Gulwada, Shaqalah sections, Kismayo General Hospital, and a number of health facilities. The field investigations, led by WHO, identified a total of 400 suspected cases of measles reported from the Jubaland State that met the case definition of measles. Most of the infected children were under-5 years of age from the camps with no history of vaccination against measles. These cases were reported from June to the end of July this year. A total of 7 samples collected from the suspected cases tested positive for measles at the Central Public Health Laboratory in Mogadishu. The tests were conducted using enzyme-linked immunosorbent assay (ELISA).
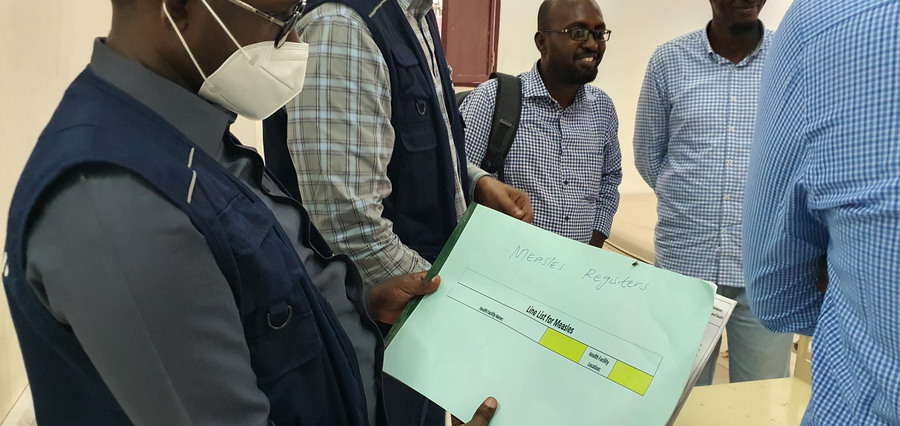
Once the outbreak was laboratory-confirmed, a response plan was drawn up. As part of this plan, the Kismayo General Hospital, one of the largest health facilities in the state of Jubaland, introduced a new isolation centre offering 20 beds for measles patients. Concurrently, WHO and Health Cluster partners provided support to strengthen case management for each patient, and helped manage the collection and testing of samples from children with symptoms. They retrained health workers on the use of case definitions and to record data using a standardized line-list in order to better understand the size of the outbreak and its geographic extent. Meanwhile, the Ministry of Health in Jubaland convened a meeting with all key partners, including the United Nations Children’s Fund (UNICEF) and WHO, to ensure all outbreak response efforts were coordinated.
Unvaccinated children due to ‘drop-outs’
Kismayo has been an epicentre for outbreaks of vaccine-preventable diseases, such as measles, in the past for a variety of reasons.
“Host to a large population of internally displaced people from neighbouring, insecure regions where access to health care is limited, we knew there could be many unvaccinated children in Kismayo and other districts. We need to boost immunization among these unvaccinated children from vulnerable and underserved families so that they remain safe,” said Mukhtar Abdi, Expanded Programme on Immunization (EPI) Manager for the Federal Government of Somalia.
Other key challenges faced in the state include a large number of drop-outs, or children who have not received all the vaccinations they require, among host communities and IDPs, coupled with limited routine immunization due to inaccessibility and presumably lack of demand for vaccines.
Additionally, the ongoing COVID-19 pandemic has had an impact on Somalia’s fragile health care system and immunization services. For instance, the vaccination coverage of pentavalent 3, which protects children against diphtheria, Haemophilus influenzae type B, hepatitis B, tetanus and whooping cough, which stood at 77% in 2019, dropped to 56% in June 2020.
Data driving decisions
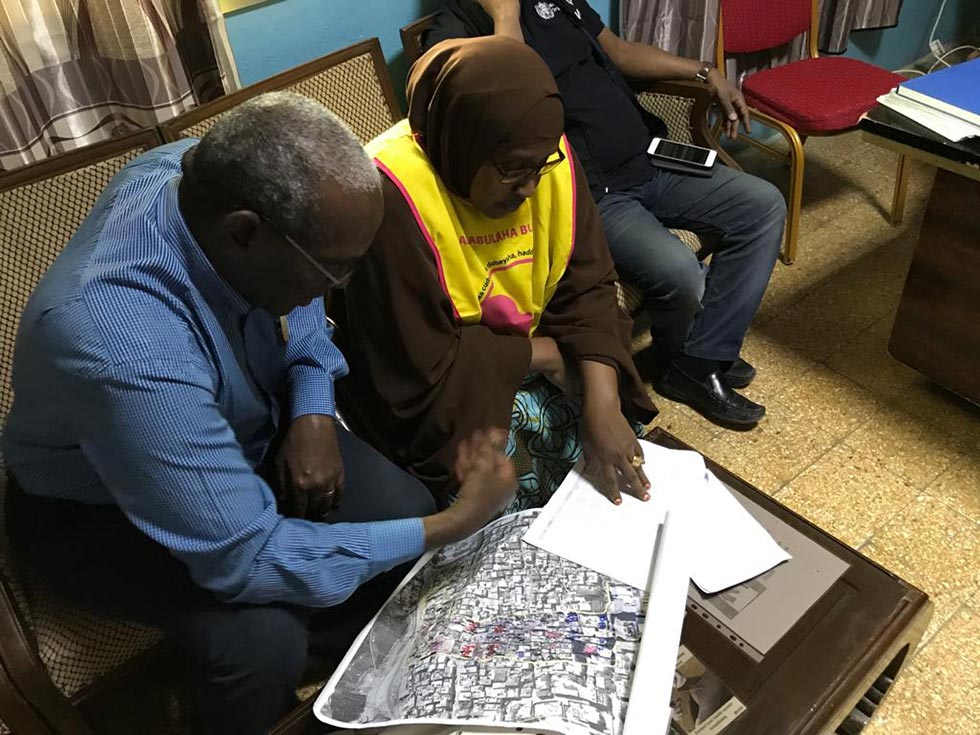
To address these challenges, health authorities, WHO and partners are using data to guide decisions they make. During outbreaks like this, epidemiological information, on the age of children, for instance, helps decide the target age for children to be vaccinated.
“Together with our partners, we have been collecting data that guides all our decisions. For instance, currently, the district of Guulwade has the largest number of cases, followed by Farjano, Shaqalah and the IDP camps. Our efforts will focus on immunizing children in these areas first,” Idris Hassan Mohamud, Director-General, Ministry of Health, Jubaland State, added.
Greater collaboration needed
“In addition to monitoring the situation closely and boosting children’s immunity in Lower Juba, to stop outbreaks from recurring, we really need to strengthen collaboration among institutions addressing immunization in Lower Juba. I am happy to say there are many agencies working in Lower Juba, but greater collaboration is needed,” said Dr Mamunur Malik, WHO Representative in Somalia. “I would like to welcome any partners who can provide support in this and other interventions to contact us and work toggether to give Somali children a healthy and bright future.”
In the coming days, health authorities will work with WHO and partners to roll out the next phase of a robust response to further curb the spread of the outbreak. Interventions being considered include strengthening collaboration with health agencies working in Lower Juba, offering measles vaccines and vitamin A to children, particularly those living in IDP camps, and mobilizing communities to understand the benefits of vaccination to create demand among caregivers across the state. Efforts will also include strengthening coordination by activating a subnational taskforce to bring all partners on board and maximize limited resources, and organizing outreach services to boost routine immunization for measles and other vaccine-preventable diseases.
EWARN detecting COVID-19 cases
The EWARN has, once again, proven its value in timely detecting an outbreak in a fragile context. WHO is expanding the coverage of EWARN in Somalia during the COVID-19 pandemic era to better track the disease, with the generous support and contributions of donors. The system is able to track and monitor other health threats too, as proven in the timely detection of this measles outbreak in Kismayo.
The recent concern of WHO and other international agencies on the significant drop in routine immunization, against diseases like measles, among vulnerable communities during the pandemic continues to be a cause for concern, as outbreaks of measles and other vaccine-preventable diseases will continue to occur and recur if swift and timely action is not taken to address the steady drop in routine immunization.
Related links
Somalia expands surveillance to better track COVID-19 outbreak
Children missing out on routine vaccinations in Somalia amid COVID-19 fears
1 Somalia’s Health Cluster is a network of national and international organizations working in the health sector across the country, under the leadership of WHO Somalia.
Note: GAVI, the Vaccine Alliance, provides support to the EPI programme in Somalia, run jointly by WHO and Somalia’s health authorities.
Children missing out on routine vaccinations in Somalia amid COVID-19 fears

29 July 2020 – In the recent past, 25-year-old Zahra Mohamud* had visited the Hawadle maternal and child health centre in Hargeisa regularly to have her older son Ibrahim* vaccinated against the most common childhood diseases. However, since the COVID-19 outbreak in Somalia, Zahra has been afraid to take her 7-month-old second son Jama* for routine vaccination at the centre fearing that she or her children might be infected with COVID-19. Her fear was perhaps justified as in health facilities in low-income countries, physical distancing and handwashing is not always possible, and not everyone can necessarily afford to buy masks.
“I have heard so many COVID-19 prevention messages that have advised us to avoid gathering in public places,” Zahra said. “Now I am afraid we could get COVID-19 from a health facility too.” Zahra explained that she would only visit a health facility if she thought it was safe. “Many parents are staying at home and not getting their children vaccinated,” added Zahra.
Even in countries with well-functioning health systems, families share the same fears as Zahra’s, and are afraid of contracting COVID-19 from health facilities which has resulted in a low uptake of regular health services.
Unfortunately, if caregivers like Zahra stop visiting health facilities to seek regular health services, children will bear the consequences of these decisions. A joint analysis of WHO and UNICEF country offices shows that by the end of June 2020, an estimated 108 000 children under one year of age in Somalia might have missed out on their first dose of measles vaccines, and close to 96 000 might have missed out on their third doses of pentavalent vaccines. In the long term, this could translate to children living compromised lives, with low immunity, and becoming more prone to catching and spreading infectious diseases. This can pose a threat to the country, region and world.
Plummeting routine immunization rates in children
In 2020, Somalia set a target of 620 000 children aged under one year for routine immunization to receive vaccines against childhood tuberculosis, polio, diphtheria, pertussis, tetanus, hepatitis B, Haemophilus influenza type B and measles. This means around 55 000 children under one year of age should be vaccinated each month. However, due to the COVID-19 pandemic, Somalia has witnessed a drop in immunization, both in outreach by health service providers and uptake by parents/caregivers.
Data gathered by the WHO and UNICEF country offices show that immunization rates plummeted from March to May 2020, rising slightly again in June, possibly due to lockdowns being eased and people being able to move more freely. Immunization rates also dropped from June 2019 to the same month this year.

COVID-19 spurs changes in programming
In 2020, the Federal Government of Somalia was forced to postpone all planned, regular large-scale health campaigns that aimed to offer eligible children measles and polio vaccines, vitamin A supplements and deworming tablets in their homes. This included 2 rounds of polio campaigns aimed at stopping the spread of circulating vaccine-derived poliovirus (cVDPV2), by reaching around 1.6 million children under the age of 5 in the southern and central regions of Somalia, and an integrated measles-polio campaign in Banadir, targeting around 300 000 children to protect them from measles and the paralyzing effects of polio.
Being proactive to avoid regressing
In a country already facing threats such as the locust invasion, recurring extremes of drought and floods, and insecurity in some states, the health system across Somalia is still fragile and health resources are limited.
If regular immunization is not continued and stepped up in the coming months, Somalia stands a high chance of reversing some of the health gains made in child health in the last few decades. The country risks witnessing outbreaks of vaccine preventable diseases, with additional children prone to contracting diphtheria, pertussis, tetanus, measles and circulating vaccine-derived polioviruses.
To avoid this situation, Dr Mamunur Malik, WHO Representative in Somalia, has reaffirmed WHO's commitment to redouble efforts to protect children from these vaccine-preventable diseases.
“The slowdown in routine immunization rate is a stark reminder to all of us of what could unwind in the coming months. Protecting the lives of children against preventable diseases should not be compromised while we respond to COVID-19. If we miss out on such a high number of children receiving life-saving vaccines, we face another public health dilemma. The outbreaks from other vaccine-preventable diseases will unfold and reverse other health gains,” Dr Malik explained. “WHO Somalia is working with the Ministry of Health, UNICEF and GAVI to resume routine immunization services and conduct accelerated immunization activities in the hotspots, to boost children’s immunity in these high-risk districts and communities.
“Evidence shows that children from displaced, evicted and other vulnerable families already have limited access to life-saving vaccinations. With a virus like COVID-19 in the picture, they are more likely to miss out on required immunization if we don’t intervene now,” said Dr Malik.
“We are first earmarking areas that need more attention. Due to its population density, frequent movement of people and the largest number of internally displaced camps in Somalia, Banadir is the most vulnerable region for the swift spread of all kinds of vaccine-preventable diseases, followed by Lower and Middle Shabelle,” said Dr Farid Muhammad, Medical Officer for the Expanded Programme on Immunization at the WHO country office in Somalia.
Ongoing efforts to improve vaccination coverage
To maintain expected standards of safety within health facilities, so that caregivers like Zahra feel safe during visits, WHO has been working with the Somali Government and partners such as the UNICEF to provide personal protective equipment (PPE) to health care providers in all public and private health facilities. Health facilities are being equipped with hand sanitizers for both health care seekers and providers to use. These facilities are also being advised to organize triaging stations so that high-risk health care seekers are recognized.
Other measures being taken include assessing the current state of routine immunization, incorporating COVID-19 prevention in plans and building the capacity of Somalia’s health workforce.
“Training health personnel is integral in stopping the spread of diseases,” said Dr Umar Al-Umra, Medical Officer, EPI and Health System Strengthening, WHO Somalia. “WHO is working with the health ministries to assess skill gaps and conduct EPI training sessions for health personnel, including COVID-19 prevention in these sessions.”
So far, 3345 community health workers have been trained and deployed as members of integrated community surveillance and rapid response teams to address the COVID-19 pandemic. These teams are disseminating messages on the importance of routine immunization and encouraging parents to vaccinate their children against vaccine-preventable diseases. At the same time, WHO has teamed up with partners to increase risk communication around COVID-19, so people understand how to keep safe.
WHO aims to boost immunization and surveillance activities further by continuing efforts to roll out supportive supervision where possible. In addition to these interventions, WHO and partners will work to strengthen surveillance of vaccine-preventable diseases and roll out an immunization strategy for urban areas, where large numbers of people live close to each other.
Note: GAVI, the Vaccine Alliance, provides support to the EPI programme in Somalia, run jointly by WHO and Somalia’s health authorities.
*Name changed to protect identity.
Confronting outbreaks in Somalia
While the COVID-19 response dominates community health concerns, every missed opportunity for vaccination puts the fragile gains made against polio in Somalia at risk of being undone
 Community surveillance teams for COVID-19 and acute flaccid paralysis speak to households about any individuals with symptoms in their area. The Somali polio team is currently steering the COVID-19 response and fighting ongoing polio outbreaks amid challenging conditions. Photo: WHO/Somalia
Community surveillance teams for COVID-19 and acute flaccid paralysis speak to households about any individuals with symptoms in their area. The Somali polio team is currently steering the COVID-19 response and fighting ongoing polio outbreaks amid challenging conditions. Photo: WHO/Somalia
22 July 2020 – For Somalis, COVID-19 is the most immediate crisis in a seemingly unending cycle of floods, food insecurity, conflict and outbreaks of vaccine-preventable diseases like measles, cholera and polio. Against this backdrop, WHO’s polio programme is working to steer the COVID-19 response and, more broadly, maintain vaccine immunity levels and improve access to health care. It’s no easy feat.
Dr Mohamed Ali Kamil, the outgoing WHO Polio Team Lead and COVID-19 incident manager for Somalia, is in awe of the commitment shown by health staff. He recently phoned a polio logistician diagnosed with COVID-19 who was experiencing symptoms to insist he stop working remotely from his sickbed. Dr Kamil recalls he said, “No sir, I will continue.”
Since the first COVID-19 case was diagnosed in Somalia on 16 March 2020, the polio programme has fought the pandemic from the ground up. Dr Kamil explains, “No other health programme has comparable expertise to serve the Somali population during the COVID-19 outbreak. During their time in the programme, members of the polio team have responded to many different disease outbreaks. This meant they were well placed and well trained to respond to COVID-19.”
“The polio programme has spent years building staff capacity and systems to implement vaccination campaigns and detect poliovirus in the community. In some ways, the team are the first and last line of defence.”
 Dr Mohamed Ali Kamil, the outgoing WHO Polio Team Lead and COVID-19 incident manager for Somalia, speaks to a polio vaccinator before the onset of the pandemic. Photo: WHO/Somalia
Dr Mohamed Ali Kamil, the outgoing WHO Polio Team Lead and COVID-19 incident manager for Somalia, speaks to a polio vaccinator before the onset of the pandemic. Photo: WHO/Somalia
The response includes education, case identification, contact tracing, case management and data support. As of June 2020, polio staff working as part of rapid response teams had reached 2.6 million people with messages about COVID-19 prevention. District Polio Officers within the teams have led the investigation of over 4500 people with suspected COVID-19 across the country. The country has set up 3 COVID-19 testing facilities and the polio structure established for the collection and shipment of stool samples from acute flaccid paralysis (AFP) cases has been used for the transportation of COVID-19 samples.
Throughout, polio personnel have continued their full-time work to end the circulating vaccine-derived poliovirus (cVDPV) outbreaks that have thus far paralyzed 16 children since 2017.
The team are driven by a humanitarian commitment to the Somali population, who have suffered over 30 years of protracted conflict and insecurity. At least 5.2 million people are in need of humanitarian assistance, and secondary and tertiary health care is virtually non-existent outside of a few large cities. Health literacy is low, and populations are highly vulnerable to diseases like polio, measles, cholera and now COVID-19. In November 2019, widespread flooding brought further turmoil and danger to Somali families.
The team’s work is made more difficult by the emotional toll wrought by the pandemic. To date at least 143 health workers have been identified with COVID-19 infection. In April, Ibrahim Elmi Mohamed, a District Polio Officer who spent 19 years striving for a polio-free Somalia, died of a COVID-19-related illness. His death, one of the many of frontline staff around the world due to COVID-19, remind us of the risks they face every time they go to work.
Challenges lie ahead to defeat polio
Dr Kamil is clear that the polio programme will require ongoing funding and the support of authorities, partners and communities in order to maintain polio activities amid the pandemic.
“To sustain the immunity gains we must implement a number of polio vaccination campaigns each year until the routine immunization programme can reach every Somali child with all polio vaccines. Somalia is extremely fragile and at high risk of becoming endemic for poliovirus if we do not maintain and support the polio infrastructure,” he says.
Since the cVDPV outbreaks were first detected in 2017, the programme has streamlined disease surveillance for cases of AFP and other preventable diseases, including by introducing mobile technology to record details of suspected cases. For the first time, environmental disease surveillance was introduced. Over 3 years, frontline health workers have implemented more than 15 polio campaigns, including integrated campaigns with the measles programme.
 A volunteer vaccinator gives 2 drops of the polio vaccine to a Somali child in August 2019. Despite efforts, many inaccessible areas remain where the programme cannot deliver vaccines. Photo: WHO/Ilyas Ahmed
A volunteer vaccinator gives 2 drops of the polio vaccine to a Somali child in August 2019. Despite efforts, many inaccessible areas remain where the programme cannot deliver vaccines. Photo: WHO/Ilyas Ahmed
Dr Kamil explains, “We still don’t know where the virus is coming from exactly. There are many inaccessible areas, where we cannot deliver vaccines or respond with immunization campaigns. We suspect that the virus is circulating among vulnerable children and communities living in these areas.”
Dr Kamil feels strongly that the polio programme has a duty to support other health interventions. He says, “COVID-19 shows what the frontline polio staff can achieve and the strength of surveillance and response systems.’’
Despite the challenges, Dr Kamil retains his belief that with ongoing funding and support, the cVDPV outbreaks in Somalia can be brought to a close. He reflects, “COVID-19 is a huge emergency in Somalia. Our staff are working flat out, and we expect to see many more cases, but at the same time we must continue to fight polio. The Somali community and the world deserve to be free of this disease.”
“We must reschedule our March polio vaccination campaign which was delayed because of the COVID 19 outbreak. We must do everything possible to keep health workers safe from COVID-19. It’s a hard situation, but we must not stop until we overcome both viruses.”
Developing the building blocks of public health ─ strengthening laboratory capacity in Somalia
13 July 2020 – “I had heard of diseases like Ebola before but thankfully they had never reached Somalia. When the COVID-19 pandemic struck countries around the world this year, my heart sank. When I saw how quickly COVID-19 was spreading, I thought Somalis would be in trouble. Other countries were beginning to go into lockdown everywhere and we had no capacity or skills to test patients for the virus,” says Dr Sahra Isse Mohamed, Director of the National Public Health Reference Laboratory. “But we were pleasantly surprised — within a record time of 3 weeks since the first case was reported, WHO, along with international and national partners, such as Medipark Diagnostics, a private laboratory in Mogadishu, teamed up with us to ensure that we built our own capacity to test for the virus.”
 Dr Sahra Isse Mohamed, Director of the National Public Health Reference Laboratory in Mogadishu, introduces UN officials to laboratory personnel and shows them testing facilities. UN Photo/Steven Candia
Dr Sahra Isse Mohamed, Director of the National Public Health Reference Laboratory in Mogadishu, introduces UN officials to laboratory personnel and shows them testing facilities. UN Photo/Steven Candia
Strengthening laboratory capacity
On 16 March 2020, after a Somali doctor, who returned from China, was confirmed as ‘patient zero’ or the first person to be confirmed with COVID-19 in Somalia, WHO and key international partners took swift, bold steps to upgrade Somalia’s diagnostic capacity. While a swab sample from patient zero was sent to the Kenya Medical Research Institute (KEMRI) in Kenya for testing, concurrently, WHO, with funding support from the Italian Agency for Development Cooperation, supported Somalia’s Ministry of Health to procure the real-time reverse transcription polymerase chain reaction (rRT-PCR) machine to test for COVID-19 samples at the National Public Health Reference Laboratory in Mogadishu. WHO purchased 2 similar machines to set up 2 additional testing laboratories for COVID-19 — one in Hargeisa, Somaliland, and the other one in Garowe, Puntland.
WHO has further expanded the testing capability of these 3 laboratories by automating the process of viral ribonucleic acid (RNA) extraction, a vital step in testing before the virus is detected in a biological sample. Considered the ‘gold standard’ for testing of COVID-19 samples, these 3 laboratories currently have the capacity to test over 1200 samples a day. One machine of this kind can test around 360 samples a day, which can be increased if required. Such molecular testing laboratories perform under a strict biosafety level (biosafety level-2), which necessitated WHO to procure the required laboratory equipment to maintain strict biosafety levels.
WHO is also providing budgetary support for hiring additional laboratory technologists to keep these laboratories functional and for operational costs and providing other consumable supplies on a regular basis to ramp up testing. In addition, 2 international virologists have been deployed for the testing laboratory in Hargeisa, Somaliland, since April this year to oversee the effective functioning of the laboratory.
WHO has trained laboratory technicians to conduct COVID-19 tests, with a focus on maintaining high standards. The Organization provided protective gear, testing kits and other laboratory supplies for the laboratory personnel working in these laboratories.
 Laboratory technicians running tests at the National Public Health Reference Laboratory in Mogadishu. UN Photo/Steven Candia
Laboratory technicians running tests at the National Public Health Reference Laboratory in Mogadishu. UN Photo/Steven Candia
“In the beginning, our laboratory staff were rushing out to test people from the community,” said Dr Sahra, “Now, trained personnel from WHO and the Ministry of Health are collecting samples from people presenting with COVID-19 symptoms and their contacts. WHO also provides support by storing samples in coldchains, in the right conditions, and sending them to any of the 3 laboratories nearby. This has really helped us, as we can focus on quality testing and training our staff.
We are now able to test for COVID-19 and other diseases ourselves, and are hoping we can keep expanding the laboratory network from 3 nationwide to one laboratory in every state, to reach more Somalis. Even though we have really been encouraged by the support we have received so far, we can still do more to fight diseases in the country,” added Dr Sahra. “It was a dream for us to have a PCR laboratory and we achieved this. We can now strive to receive international accreditation.”
Acknowledging the role of laboratories and personnel
In their efforts to show support to Somali health workers and the ongoing response to COVID-19 in Somalia, the WHO Somalia Representative Dr Mamunur Malik and the UN Secretary-General’s Special Representative for Somalia Mr James Swan visited the National Public Health Reference Laboratory in Mogadishu on 29 June 2020. They met with laboratory personnel and commended them for their dedication, hard work and professionalism in the response to the ongoing pandemic.
“Well-equipped, well-functioning laboratories are key building blocks for any health system and disease surveillance system,” said Dr Malik. “Thanks to the timely support of donors and partners, Somalia has been able to step up efforts to diagnose COVID-19 and assist people who are infected. The building of such in-country testing capability, rapidly, has helped us to monitor and track the virus spread in the community. We will continue to support these laboratories even further to build their capability to test, diagnose and respond to other infectious diseases, including all high-threat pathogens, using the same molecular testing facilities that we have supported in these 3 laboratories. We also take this opportunity to continue to express our gratitude to Somalia’s health professionals for working selflessly to protect Somalis.”
Somali women playing a key role
Explaining how difficult it has been for her to work under pressure in the last 4 months, Dr Sahra added with a smile, “I am happy to say that half of our team consists of qualified Somali women. Besides, even our Minister of Health, who is in charge of health in the country, is a lady.”
As of 11 July 2020, Somalia had 3051 confirmed COVID-19 cases; 1264 people have recovered from COVID-19, and 92 Somalis have lost their lives to the newly discovered virus.
Note
The following agencies and donors have provided support to the National Public Health Reference Laboratory: the Italian Agency for Development Cooperation (AICS), Medipark Diagnostics Laboratory, UN Development Programme (UNDP), UN Support Office for Somalia (UNSOS), UN World Food Programme (WFP) and US Agency for International Development (USAID).


