Region galvanizes around polio eradication during the 67th Regional Committee
 Delegates listen to Regional Polio Director Dr Hamid Jafari’s presentation on polio eradication in the Eastern Mediterranean Region. Credit: WHO/EMRO
Delegates listen to Regional Polio Director Dr Hamid Jafari’s presentation on polio eradication in the Eastern Mediterranean Region. Credit: WHO/EMRO
Renewed political commitment drives likely formation of new subcommittee for polio eradication and outbreaks.
14 October 2020 – Yesterday the 67th Regional Committee for the Eastern Mediterranean discussed a resolution on polio, which includes the creation of a new ministerial regional subcommittee to focus on the most critical barriers standing in the way of polio eradication.
Following the certification of the African Region as free of wild poliovirus, the Eastern Mediterranean Region is the only region in the world still harbouring wild poliovirus. After a bruising 2019 where we saw wild poliovirus on the rebound in Afghanistan and Pakistan, 2020 dawned with high hopes that the programme would be able to shift gear and make up for lost ground. The COVID-19 pandemic put the brakes on those plans and added untold layers of complexity to the provision of health care, but it hasn’t destroyed the dream. The new subcommittee, if adopted, will be a strong demonstration of Member States’ political commitment and solidarity towards getting polio eradication back on track.
The risk of international spread of poliovirus remains a public health emergency of international concern. During 2020, the Region has experienced new outbreaks of vaccine-derived poliovirus in Sudan and Yemen, even as the outbreaks in Somalia, Afghanistan and Pakistan continue to paralyse children. The new subcommittee would aim to intensify support to these countries. An immediate priority is advocating for the domestic and international financial resources needed to close outbreaks and eradicate the disease once and for all.
In the next few months, the polio programme plans to roll out a new type 2 oral polio vaccine, specifically designed to tackle vaccine-derived outbreaks. This is likely to have a transformative effect on our abilities to protect children and stop outbreaks spreading further. But the introduction of a new vaccine does not negate the importance of other tactics to fight vaccine-derived polio, including high quality disease surveillance, building community vaccine acceptance and strengthening routine childhood immunization.
The messages the subcommittee would likely convey in its reports to WHO's governing bodies apply to all polioviruses: that routine and supplementary immunization systems must improve across the Region, and every child must receive the vaccines they need. The subcommittee would also work to promote political and social neutrality and facilitate access to all children living in conflict-affected areas.
The subcommittee would be made up of health ministers from interested Member States of the Region, with special invitations extended to representatives from Afghanistan and Pakistan. The group would meet four times a year.
During the Regional Committee meeting, the Governments of Egypt, Islamic Republic of Iran and Pakistan expressed a desire to lead the charge by joining the subcommittee. If the resolution is adopted, WHO will be inviting all ministers of health to express their interest in becoming members.
The Pakistan representative stated, “The Government of Pakistan welcomes and supports the establishment of a subcommittee of polio eradication. Dr Faisal Sultan, the Special Assistant to the Prime Minister on Health, has expressed his willingness to take part in the subcommittee, which will undoubtably provide an ideal platform to strengthen regional cooperation and support Afghanistan and Pakistan in successfully eradicating poliovirus across the shared epidemiological block.”
Dr Hamid Jafari, WHO Regional Director for Polio Eradication, thanked Member States for offering their support for the creation of the subcommittee, and the entire resolution, saying, “This is a crucial step forward to regain ground lost against the poliovirus in the last two years. Strong political commitment to the polio eradication goal is paramount for us to defeat this disease”.
In the run up to World Polio Day on 24 October, the adoption of the resolution would be a meaningful step forward towards achieving a polio-free future for all children in the Eastern Mediterranean Region. The WHO continues to emphasize the importance of high-quality immunization for every child, and advocates for access to every community in order to reach all children with vital health services.
Confronting outbreaks in Somalia
While the COVID-19 response dominates community health concerns, every missed opportunity for vaccination puts the fragile gains made against polio in Somalia at risk of being undone
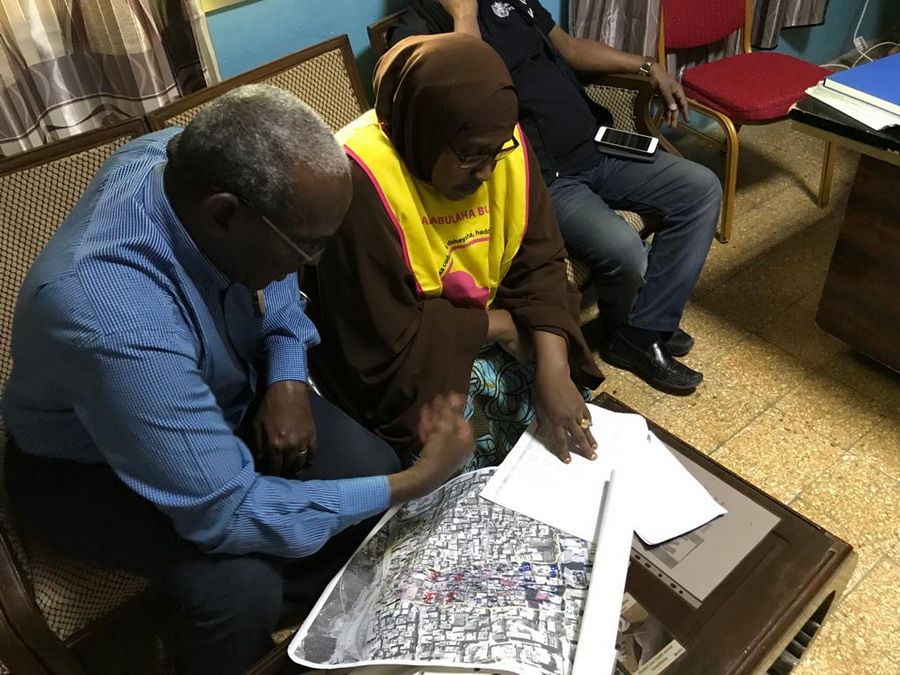
 Community surveillance teams for COVID-19 and acute flaccid paralysis speak to households about any individuals with symptoms in their area. The Somali polio team is currently steering the COVID-19 response and fighting ongoing polio outbreaks amid challenging conditions. Photo: WHO/Somalia
Community surveillance teams for COVID-19 and acute flaccid paralysis speak to households about any individuals with symptoms in their area. The Somali polio team is currently steering the COVID-19 response and fighting ongoing polio outbreaks amid challenging conditions. Photo: WHO/Somalia
22 July 2020 – For Somalis, COVID-19 is the most immediate crisis in a seemingly unending cycle of floods, food insecurity, conflict and outbreaks of vaccine-preventable diseases like measles, cholera and polio. Against this backdrop, WHO’s polio programme is working to steer the COVID-19 response and, more broadly, maintain vaccine immunity levels and improve access to health care. It’s no easy feat.
Dr Mohamed Ali Kamil, the outgoing WHO Polio Team Lead and COVID-19 incident manager for Somalia, is in awe of the commitment shown by health staff. He recently phoned a polio logistician diagnosed with COVID-19 who was experiencing symptoms to insist he stop working remotely from his sickbed. Dr Kamil recalls he said, “No sir, I will continue.”
Since the first COVID-19 case was diagnosed in Somalia on 16 March 2020, the polio programme has fought the pandemic from the ground up. Dr Kamil explains, “No other health programme has comparable expertise to serve the Somali population during the COVID-19 outbreak. During their time in the programme, members of the polio team have responded to many different disease outbreaks. This meant they were well placed and well trained to respond to COVID-19.”
“The polio programme has spent years building staff capacity and systems to implement vaccination campaigns and detect poliovirus in the community. In some ways, the team are the first and last line of defence.”
 Dr Mohamed Ali Kamil, the outgoing WHO Polio Team Lead and COVID-19 incident manager for Somalia, speaks to a polio vaccinator before the onset of the pandemic. Photo: WHO/Somalia
Dr Mohamed Ali Kamil, the outgoing WHO Polio Team Lead and COVID-19 incident manager for Somalia, speaks to a polio vaccinator before the onset of the pandemic. Photo: WHO/Somalia
The response includes education, case identification, contact tracing, case management and data support. As of June 2020, polio staff working as part of rapid response teams had reached 2.6 million people with messages about COVID-19 prevention. District Polio Officers within the teams have led the investigation of over 4500 people with suspected COVID-19 across the country. The country has set up 3 COVID-19 testing facilities and the polio structure established for the collection and shipment of stool samples from acute flaccid paralysis (AFP) cases has been used for the transportation of COVID-19 samples.
Throughout, polio personnel have continued their full-time work to end the circulating vaccine-derived poliovirus (cVDPV) outbreaks that have thus far paralyzed 16 children since 2017.
The team are driven by a humanitarian commitment to the Somali population, who have suffered over 30 years of protracted conflict and insecurity. At least 5.2 million people are in need of humanitarian assistance, and secondary and tertiary health care is virtually non-existent outside of a few large cities. Health literacy is low, and populations are highly vulnerable to diseases like polio, measles, cholera and now COVID-19. In November 2019, widespread flooding brought further turmoil and danger to Somali families.
The team’s work is made more difficult by the emotional toll wrought by the pandemic. To date at least 143 health workers have been identified with COVID-19 infection. In April, Ibrahim Elmi Mohamed, a District Polio Officer who spent 19 years striving for a polio-free Somalia, died of a COVID-19-related illness. His death, one of the many of frontline staff around the world due to COVID-19, remind us of the risks they face every time they go to work.
Challenges lie ahead to defeat polio
Dr Kamil is clear that the polio programme will require ongoing funding and the support of authorities, partners and communities in order to maintain polio activities amid the pandemic.
“To sustain the immunity gains we must implement a number of polio vaccination campaigns each year until the routine immunization programme can reach every Somali child with all polio vaccines. Somalia is extremely fragile and at high risk of becoming endemic for poliovirus if we do not maintain and support the polio infrastructure,” he says.
Since the cVDPV outbreaks were first detected in 2017, the programme has streamlined disease surveillance for cases of AFP and other preventable diseases, including by introducing mobile technology to record details of suspected cases. For the first time, environmental disease surveillance was introduced. Over 3 years, frontline health workers have implemented more than 15 polio campaigns, including integrated campaigns with the measles programme.
 A volunteer vaccinator gives 2 drops of the polio vaccine to a Somali child in August 2019. Despite efforts, many inaccessible areas remain where the programme cannot deliver vaccines. Photo: WHO/Ilyas Ahmed
A volunteer vaccinator gives 2 drops of the polio vaccine to a Somali child in August 2019. Despite efforts, many inaccessible areas remain where the programme cannot deliver vaccines. Photo: WHO/Ilyas Ahmed
Dr Kamil explains, “We still don’t know where the virus is coming from exactly. There are many inaccessible areas, where we cannot deliver vaccines or respond with immunization campaigns. We suspect that the virus is circulating among vulnerable children and communities living in these areas.”
Dr Kamil feels strongly that the polio programme has a duty to support other health interventions. He says, “COVID-19 shows what the frontline polio staff can achieve and the strength of surveillance and response systems.’’
Despite the challenges, Dr Kamil retains his belief that with ongoing funding and support, the cVDPV outbreaks in Somalia can be brought to a close. He reflects, “COVID-19 is a huge emergency in Somalia. Our staff are working flat out, and we expect to see many more cases, but at the same time we must continue to fight polio. The Somali community and the world deserve to be free of this disease.”
“We must reschedule our March polio vaccination campaign which was delayed because of the COVID 19 outbreak. We must do everything possible to keep health workers safe from COVID-19. It’s a hard situation, but we must not stop until we overcome both viruses.”
Training health workers to fight COVID-19 in Sudan
Polio personnel are putting in the hours to strengthen response
 Dr Niazy trains medical staff on handwashing during a COVID-19 training session in River Nile state. Photo: WHO/Sudan
Dr Niazy trains medical staff on handwashing during a COVID-19 training session in River Nile state. Photo: WHO/Sudan
28 May 2020 – The polio eradication programme has stepped up to help the Sudanese Ministry of Health limit spread of the COVID-19 virus. The programme is working in 14 states in the country supporting COVID-19 surveillance, information dissemination and training of health workers.
Dr Niazy Abd Alhameed Abd Alwahab, a National Medical Officer for the polio programme since 2013, is one of the personnel playing a key role. He and colleagues recently led 2 WHO COVID-19 trainings in River Nile state, one for rapid response teams and one for local hospital staff, in addition to supporting training run by the State Ministry of Health.
Thanks to the training, health workers in all 7 localities in the state are ready to help individuals who are showing symptoms of COVID-19. In total, more than 3000 rapid response team members have been trained across Sudan with support from polio National Medical Officers.
By early May, River Nile state had suffered 7 cases of COVID-19, with 2 fatalities. “The state is organized to respond,” Dr Niazy explains, “All patients are being treated in dedicated isolation facilities in hospitals, and medical staff are on high alert for more cases. We helped train teams so that they are able to serve the population.”
Training rapid response teams
A 5-day training of rapid response teams, funded by WHO, was targeted at 7 teams, one from each state locality. Of the 42 individuals trained, 30 were women and 12 were men. The teams have been created for the COVID-19 response. Each team contains individuals with the collective public health experience to contribute to local efforts to fight the virus, spearheading work in contact tracing and engagement with the community.
The first day of training was attended by the Director General Health of the State Ministry of Health and the Head of the Emergency Humanitarian Assistance department.
Dr Niazy explains that over the 5 days, participants gained a comprehensive understanding of Sudan’s COVID-19 surveillance and contact tracing systems, infection prevention and control practices, case management methods, and how to collect samples and arrange shipment to the national laboratory in Khartoum. Participants were also trained on how to use PPE safely and how best to wash their hands.
“Participants were encouraged to take part in interactive exercises to test and strengthen their knowledge, as well as take part in discussions,” he says.
“By the end of the training, all participants were fully trained and able to pass on their knowledge in their localities.”
Training local health staff
The polio programme also supported a 2-day COVID-19 training for 34 women and 22 men who work in state hospitals as doctors, laboratory technicians, or other medical personnel. The programme continues to support the State Ministry of Health with further local training, including for medical registrars.
Ongoing challenges
The situation in River Nile state is very challenging. There are chronic shortages of PPE, hand sanitizer and masks, and WHO is offering urgent support to help procure these. Severe shortages of fuel and currency are making response more difficult. Social norms in some communities dissuade individuals with COVID-19 symptoms from seeking medical assistance, and work must be carried out to build trust and ensure people with COVID-19 are found and offered care.
To serve the COVID-19 response and prevent virus spread, the polio eradication programme has had to scale back some of its usual work. Dr Niazy explains, “Vaccination campaigns are paused, and many private clinics are closed, some of the public health centres are turned into isolation centres as part of the response to this emergency. This makes detecting acute flaccid paralysis (AFP) more difficult, as health personnel are trained to report children with AFP who come to the health centres.”
Efforts are being made across the Eastern Mediterranean Region to minimize the impact of COVID-19 on the overall health of populations, during a time when many health activities cannot go ahead. In Sudan, a number of children do not have full immunity against polio, and it is critical that routine immunization continues where possible until vaccination campaigns can resume.
Dr Hoda Youssef Atta, acting WHO Representative, explains, “During the COVID-19 emergency the polio eradication programme is committed to providing expertise, training and medical skills to protect Sudan. However, as soon as it is safe to do so, we must scale up programme operations once more to protect vulnerable populations from polio.”
Somalia’s polio teams help combat COVID-19
 Polio programme staff are conducting disease surveillance for COVID-19 as well as educating communities on the symptoms of the virus, how to prevent transmission, and how to report suspected cases. ©WHO/Somalia4 May 2020 – “The road to the mountain village was rough. It’s only 50 kilometres, but it took more than 3 hours,” says Dr Fatima Ismail, a disease surveillance officer working in Somaliland. “We were bouncing in the car.”
Polio programme staff are conducting disease surveillance for COVID-19 as well as educating communities on the symptoms of the virus, how to prevent transmission, and how to report suspected cases. ©WHO/Somalia4 May 2020 – “The road to the mountain village was rough. It’s only 50 kilometres, but it took more than 3 hours,” says Dr Fatima Ismail, a disease surveillance officer working in Somaliland. “We were bouncing in the car.”
In early 2020, Dr Fatima’s team headed to a remote village near Djibouti to check on a small boy. The boy’s right arm and leg showed a kind of paralysis that sometimes indicates polio. “The village polio volunteer in this mountainous area, geographically inaccessible, found an acute flaccid paralysis (AFP) case,” Dr Fatima remembers.
When children show signs of this paralysis, it’s critical to get stool samples to a laboratory to determine whether they have polio. Polio teams ride camels in the desert or donkeys in the mountains when they have to. They brave bombs to get samples out of conflict zones to laboratories. In brutally hot climates, they plug mini-freezers into car dashboards to keep samples cool.
All over the world, polio surveillance systems that have been built up over decades track infection sources, evaluate symptoms and transport samples to the laboratory — despite distance, natural disasters, and sometimes war. Now, this network of disease surveillance — reaching into the most far-flung corners of the globe — is being tapped to address the COVID-19 pandemic.
“In Somalia, the polio programme pivoted its workforce of thousands of frontline staff to support the effort as the cases of COVID-19 spread. Rapid response teams — made up of disease surveillance officers, community health care workers and volunteers — were trained to educate people about the virus and to test suspected cases. By April 2020, the teams were deployed in the field,” said Dr Mamunur Malik, WHO Representative in Somalia.


