Limb Reconstruction Centre launched to assist patients with gunshot injuries in Gaza
5 March 2020, Gaza Strip - Today the World Health Organization in partnership with the Ministry of Health launched a Limb Reconstruction Centre for Gaza Strip, providing hundreds of Palestinians injured with gunshot wounds, with permanent specialized and centralised care.
Based at Nasser Medical Complex in Khan Yunis and generously funded with UK aid, EU humanitarian aid, by the Swiss Agency for Development and Cooperation, the United Nations oPt Humanitarian Fund and the Spanish Agency for International Development Cooperation, the new Centre features a 32-bed ward, two dedicated operating theatres, and 25 specialized multidisciplinary staff (including four orthopedic surgeons, psychologists and physiotherapists).
“The Limb Reconstruction Centre is a new centre of care and excellence, which will provide better quality, faster and more sophisticated treatment and rehabilitation to patients with gunshot injuries sustained during the Great March of Return. It will cater for a wide range of patient needs from wound care, surgery, infection control and physiotherapy to mental health support,” said Dr Gerald Rockenschaub, WHO’s Head of Office for the occupied Palestinian territory.
“This Centre will help transform the lives of those affected by preventing disabilities and amputations, and also restore dignity and hope to those patients who have been left powerless, unable to function and support their families and communities in what is already a difficult environment,” said Mr Jamie McGoldrick, Humanitarian Coordinator for the oPt.
Since the start of the Great March of Return in the Gaza Strip from March 2018 to 31 December 2019, 33,141 injuries and 322 deaths (including 65 children) have been reported. More than 7,951 suffered from gunshot wounds, and 88% of these presented limb wounds.
''The Great March of Return demonstrations in the Gaza Strip, has not only caused tremendous suffering for many families in Gaza but also has placed enormous strain on Gaza’s already under-resourced and over-burdened health care system. Gaza health facilities are facing a critical shortage of essential medicines and supplies, as well as a lack of specialised doctors and nurses. This new Centre will help to address some of these challenges through providing specialised treatment and support for patients requiring limb reconstruction surgery,'' said the EU Representative Sven Kühn von Burgsdorff.
''Today is yet another occasion to recall that the situation in Gaza remains fragile and unpredictable. It is the time to turn the page. Only a political solution can bring fundamental change and put an end to the violence, suffering and hardship,'' he added.
Six hundred patients have already been identified as being in need of limb reconstruction surgery (according to the Ministry of Health as of February 2020) and hundreds more wait to be assessed. Already more than 40 patients have been operated on since the Centre began operation in December 2019.
Gunshot injuries are complicated, expensive and difficult to treat: they can take up to two years to treat per patient; involve four to five surgeries for bone, muscles, soft tissue and nerves; and often involve serious bone infections. Rates of bone infection are extortionately high and an increasing number of patients are showing signs of antibiotic resistance, which increases the chance of amputation and the risk of infection to other patients. A dedicated osteomyelitis (bone infection) treatment centre, built by Médecins Sans Frontières-France in 2020, will be located adjacent to the Limb Reconstruction Centre and complement it.
While there have been medical missions for limb reconstruction in Gaza in the past, there hasn’t been a centralised service which provides permanent and dedicated operating theatres and resources from a multidisciplinary team. This Centre will help coordinate specialized limb reconstruction treatment to rationalize human resources, time, equipment and costs and also establish a patient database to unify information used by all partners deploying emergency medical teams for limb reconstruction services. The Limb Reconstruction Center will also facilitate much-needed training to upskill Gaza’s medical professionals, paving the way for a new generation of trained medical professionals in Gaza. Visiting specialist medical teams will focus their interventions in a centralized structure, maximizing training opportunities for younger resident staff.
Also at Nasser Medical Complex, WHO has installed a CT Scanner, funded by EU humanitarian aid, which will benefit an estimated 11,000 patients per year.
Background information:
The Limb Reconstruction Centre is a vital part of WHOs’ trauma and emergency care programme, which is working with the Ministry of Health (MoH) and partners on an extensive series of interventions that aim to improve the management of traumatic injuries, from the point of injury, at the prehospital level all the way to hospital care, including emergency departments and surgery, to rehabilitation and recovery. With the generous support of donors, since the start of GMR demonstrations in 2018, this programme has helped establish and upgrade 10 Trauma Stabilization Points (TSPs) in critical zones in Gaza with the Palestinian Red Crescent Society (PRCS) and MoH to reduce the burden on the overloaded hospitals substantially. At the TSPs, wounded patients receive life-saving care close to the point of injury and saved on average 1200 lives in a year (from 30 March 2018 to 30 March 2019).
As part of the trauma pathway, in 2020 WHO will:
- upgrade six trauma hospitals in Gaza and four in the West Bank to create a trauma response network, providing a range of interventions, from improved infrastructure, provision of supplies, training and clinical coaching for all doctors and nurses working at the emergency departments
- build on the success of the TSPs, by expanding them to the Eastern Mediterranean region to respond to conflict related trauma in the region
- support the PCRS to centralize all ambulance movements through a new ambulance dispatch centre
- provide training for surgeons on acute surgery in the six trauma hospitals to improve damage control surgery through basic principles of control of haemorrhage, prevention of contamination and protection from further injury
- provide training to PRCS and MoH staff to provide frontline care in an acute emergency
- support the running costs and supplies for the Limb Reconstruction Centre.
The World Health Organization (WHO) is appealing for US$ 20 million over three years to provide life- and limb-saving interventions to large numbers of injured patients and to build on the previous success of the WHO supported interventions and ensure better health outcomes for Palestinians through strengthened continuum of care along the trauma pathway.
For more information, please contact:
Alice Plate, WHO Communications Specialist, occupied Palestinian Territory
+972 54 6153900 |
WHO doctor awarded for helping the mothers and babies of Gaza, December 2019
 WHO obstetrician and gynaecologist Dr Nashwa Skaik, leads the pioneering Early Essential Newborn Care project which assists with 75 per cent of all births in Gaza , has been awarded WHO Director General’s Award of Excellence for her work. Credit: WHO
WHO obstetrician and gynaecologist Dr Nashwa Skaik, leads the pioneering Early Essential Newborn Care project which assists with 75 per cent of all births in Gaza , has been awarded WHO Director General’s Award of Excellence for her work. Credit: WHO
29 December 2019, Gaza - “Families and in particular, mothers and infants, are the essence of any society and they should never be neglected. I am immensely honoured and grateful to this recognition, which is a true reflection of the global and regional efforts to improve mother and newborn health in all settings. This reward is a huge push forward to myself and the team in our office,” WHO’s obstetrician and gynaecologist in Gaza Dr Nashwa Skaik reflects after receiving the WHO Director General’s Award of Excellence for her work managing a pioneering maternal and newborn healthcare project in the Gaza Strip to prevent and treat the key causes of newborn death and diseases.
In Palestine, babies aged less than one-month old account for 50 per cent of deaths in children under five. Half of these baby deaths occur in the first day of life, mainly from complications related to prematurity, birth asphyxia, and infection.
Based on international evidence, Dr Nashwa and colleagues at the World Health Organisation, rolled out the Early Essential Newborn Care project in 2017 with the Ministry of Health in Gaza to ensure that quality essential care is provided during critical moments around birth, in addition to care for premature, low-birthweight and sick babies.
The project has strengthened the Ministry of Health’s system from the bottom up, by coaching local clinical staff with a package of simple and cost effective evidence-based interventions during childbirth and immediately after, and focusing on the elimination of harmful and outdated practices in the first 24 hours of life. This includes reshaping policy and guidelines; managing supplies and staff and providing health information.
The project now covers 75 per cent of all births in Gaza in maternity and neonatal units in four targeted hospitals and widespread adoption has resulted in significant improvements since 2017 in key areas including:
early and exclusive breastfeeding take up improved from 21% to 52.5% from 2017 to 2019. These practices, where the infant receives breastmilk within one hour of birth and infant only receives breastmilk without additional food or drink, are known to lower newborn deaths by 22%. Breastfeeding protects the baby from common childhood illnesses such as diarrhoea and pneumonia and may also have longer-term health benefits, such as reducing the risk of overweight and obesity in childhood and adolescence.
babies receiving sustained skin-to-skin (STS) contact, increased from 0 to 35% from 2017 to 2019. This practice, when a baby is laid directly on their mother’s bare chest shortly after birth, is essential to prevent temperature losses and diseases that lead to infection and death. Among infants who received this care, there is a reduction in newborn admission to intensive care due to respiratory problems by 5% in Gaza. In addition, it helps parents bond with their babies supports better physical and developmental outcomes for the baby.

Caption: WHO obstetrician and gynaecologist Dr Nashwa Skaik, leads the pioneering Early Essential Newborn Care project which assists with 75 per cent of all births in Gaza, has been awarded WHO Director General’s Award of Excellence for her work.
Dr Skaik said she treasures the opportunities she gets at the World Health Organization, “They are like no other place. I enjoy my everyday work with the team and the space I am given to be more creative and innovative. We try our best to deliver high quality and unique care to all mothers and babies in Gaza which ensure they thrive and survive despite the difficult circumstances.”
The WHO team congratulates Dr Skaik and colleagues in Gaza for their dedication and achievements to improving the lives of mothers and babies in Gaza.
WHO mobile clinic donated by Japan joins Iran’s emergency fleet

Tehran, 3 December 2019, With support from Japan, WHO has delivered a mobile clinic to the Islamic Republic of Iran to improve access of vulnerable people -- especially those displaced or affected by floods -- to essential lifesaving health services.
The mobile clinic joined the country’s emergency medical service fleet, and will provide outreach services to populations and communities where health facilities do not exist, are not functional or are inaccessible. As the clinic moves from area to area, vulnerable and often displaced communities will be able to receive access to life-saving health services.
Services provided by the clinic include diagnosis, treatment, immunization, early disease detection, control and response services, referral of critical cases to advanced care, and detection of possible outbreaks of diseases. The mobile clinic is accompanied by a medical team and pharmaceutical supplies to cover a range of essential health services for children, women and elderly.
Expressing his gratitude to the government of Japan for the donation of the mobile clinic, Head of the National Emergency Medical Organization (NEMO) Dr Pirhossein Kolivand stated that the increasing collaboration between NEMO, WHO and the Government of Japan will improve humanitarian aid to the people of Iran in many areas related to public health.

WHO Representative in the Islamic Republic of Iran Dr Christoph Hamelmann reiterated that during recent years, WHO’s collaboration with NEMO has grown substantially, as demonstrated during the successful response to the widespread floods in Iran in 2019. Support from the Government of Japan in an Emergency Aid Grant worth US$ 700,000 allowed WHO to meet urgent health needs of people affected by the floods.
“Japan was among the first nations that expressed readiness to support WHO in providing humanitarian assistance to flood-affected areas. We truly appreciate the commitment and practical support of the people of Japan,” Dr Hamelmann added.
Ambassador of Japan H. E. Mr. Mitsugu Saito underscored the seriousness of the damages caused by the floods to the health sector, and reiterated Japan’s support to WHO in providing primary health care services through the mobile clinic, as well as essential vaccines and medicines.
MERS situation update, October 2019
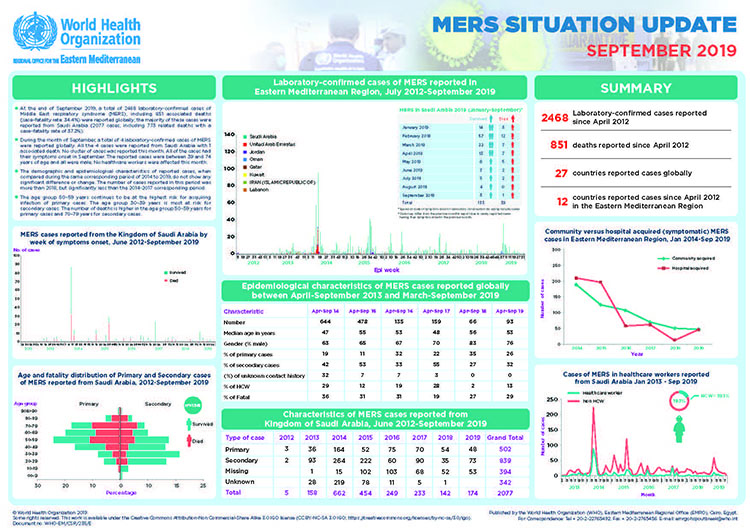 Read the situation update for October 2019At the end of October 2019, a total of 2482 laboratory-confirmed cases of Middle East respiratory syndrome (MERS), including 854 associated deaths (case–fatality rate: 34.4%) were reported globally; the majority of these cases were reported from Saudi Arabia (2090 cases, including 776 related deaths with a case–fatality rate of 37.1%).
Read the situation update for October 2019At the end of October 2019, a total of 2482 laboratory-confirmed cases of Middle East respiratory syndrome (MERS), including 854 associated deaths (case–fatality rate: 34.4%) were reported globally; the majority of these cases were reported from Saudi Arabia (2090 cases, including 776 related deaths with a case–fatality rate of 37.1%).- During the month of October, a total of 14 laboratory-confirmed cases of MERS were reported globally. 13 of the cases were reported from Saudi Arabia with 3 associated deaths and 1 case was reported from United Arab Emirates. One healthcare worker was also infected this month while providing care for a case. No other cluster of cases was reported this month. Two of the cases had their symptom onset in September. The 3 deaths reported were within the 70-79 age group.
- The demographic and epidemiological characteristics of reported cases, when compared during the same corresponding period of 2014 to 2019, do not show any significant difference or change. The number of cases reported in this period was less than all other corresponding periods.
- The age group 50–59 years continues to be at the highest risk for acquiring infection of primary cases. The age group 30–39 years is most at risk for secondary cases. The number of deaths is higher in the age group 50–59 years for primary cases and 70–79 years for secondary cases.
Read the latest MERS update for October 2019
Subscribe to the Infectious Hazard Management monthly e-mail update for the latest data and analysis.


