Research article
H.A. Naqvi,1 S. Sabzwari,2 S. Hussain,1 M. Islam 2 and M. Zaman 3
وعي الممارسين العامّين ومعالجتهم للاضطرابات النفسية الشائعة: مسح مجتمعي في كاراتشي في باكستان
حيدر علي نقوي، سانيه سبزواري، سجاد حسين، محمد إسلام، محمد زمان
الخلاصة: قيَّمَت هذه الدراسة معارف الممارسين العامين ومعالجتهم للاضطرابات النفسية الشائعة في كاراتشي في باكستان. وقد أجرى الباحثون مقابلات منهجية في عام 2009 مع 360 ممارساً عاماً اختاروهم وفق الاعتيان العشوائي للمجموعة. وقدَّر الباحثون أن عدد المرضى المصابين باضطرابات نفسية يصل إلى %10 من العبء اليومي من الحالات، وذلك وفقاً لتقديرات %71.8 من الأطباء. ولم يكن لدى ثلثي الأطباء العامين معرفة بمعايير التشخيص لاضطرابات الاكتئاب والقلق، وفقاً للمراجعة العاشرة للتصنيف الدولي للأمراض ICD-10. وكانت مجموعة الأدوية المعروفة أكثر من غيرها هي البنزوديازيبين والأكثر استعمالاً لجميع حالات الصحة النفسية (%75.3). وكان مجموعة أقل من الممارسين العموم على دراية بالمثبطات الانتقائية لالتقاط السيروتونين (%35.1)، أو مضادات الاكتئاب الثلاثية الحلقات (%20.2). ووجد الباحثون أن عدم وجود الوقت الكافي والقيود المالية لدى المرضى هي من ضمن العقبات التي أبلغ أنها تقف أمام الرعاية. كما وجد الباحثون أن أغلب الممارسين العامين (%69.2) لم يتلقوا أي تعليم طبي حديث حول مشاكل الصحة النفسية، وأن الفجوات في معارف الممارسين العامين حول معالجة الاضطرابات النفسية لها آثارها على الاستخدام الرشيد للأدوية النفسية في الرعاية الأولية.
ABSTRACT This study assessed the knowledge and management of common psychiatric disorders by general practitioners (GPs) in Karachi, Pakistan. Structured interviews were carried out in 2009 with 360 GPs selected by cluster random sampling. Patients with psychiatric disorders were estimated to be up to 10% of the daily caseload according to 71.8% of doctors. Two-thirds of GPs were unaware of the ICD-10 diagnostic criteria for depression and anxiety disorders. Benzodiazepines were the most recognized category of medication (75.3%) and were the most commonly used medication for all mental health conditions. Fewer GPs were familiar with selective serotonin reuptake inhibitors (35.1%) or tricyclic antidepressants (20.2%). Lack of time and patients’ financial constraints were reported to be barriers to care. Most GPs (69.2%) had not received any recent medical education about mental health problems. Gaps in GPs’ knowledge about the management of mental disorders have implications for the rational use of psychotropic medications in primary care.
Sensibilisation des médecins généralistes aux troubles psychiatriques courants et prise en charge de ces troubles : une enquête communautaire à Karachi (Pakistan)
RÉSUMÉ La présente étude a évalué les connaissances des médecins généralistes sur les troubles psychiatriques courants et la prise en charge de ces troubles par ces derniers à Karachi (Pakistan). Des entretiens structurés ont été menés en 2009 auprès de 360 médecins généralistes sélectionnés par échantillonnage aléatoire en grappes. Il a été estimé que les patients souffrant de troubles psychiatriques représentaient 10 % du nombre de cas à traiter par jour selon 71,8 % des médecins. Deux tiers des médecins généralistes ne connaissaient pas les critères diagnostiques de la CIM-10 pour les troubles dépressifs et anxieux. Les benzodiazépines représentaient la catégorie de médicaments la plus connue (75,3 %) et la plus fréquemment utilisée pour tous les troubles mentaux. Les médecins généralistes qui connaissaient bien les inhibiteurs sélectifs de la recapture de la sérotonine (35,1 %) ou les antidépresseurs tricycliques (20,2 %) étaient moins nombreux. Le manque de temps et les contraintes financières des patients étaient des obstacles aux soins. La majorité des médecins généralistes (69,2 %) n'avaient pas suivi de formation médicale récente sur les troubles de santé mentale. Les failles dans les connaissances des médecins généralistes concernant la prise en charge des troubles mentaux ont des conséquences sur l'utilisation rationnelle des médicaments psychotropes en soins de santé primaires.
1Department of Psychiatry, Aga Khan University, Karachi, Pakistan (Correspondence to H.A. Naqvi:
2Department of Family Medicine; 3Section of Epidemiology and Statistics, Community Health Sciences, Aga Khan University Hospital, Karachi, Pakistan.
Received: 10/03/10; accepted: 30/08/10
EMHJ, 2012, 18(5): 446-453
Introduction
The World Health Organization (WHO) has proposed that mental health care should be integrated within general health services in a decentralized manner [1]. Goldberg has argued that closer collaboration between general practitioners (GPs) and psychiatric services can bring advantages to patients, to primary care staff and to mental health staff [2]. Certainly the supply of psychiatrists in developing South East Asian countries is much smaller than that in the developed world (typically below 0.4 per 100 000 versus 9–25 per 100 000), implying that primary care must be one of the main providers of mental health care for all forms of disorders. However, many developing countries are not only short of psychiatrists they are also short of physicians [3,4]. The situation is not so different in Pakistan where the primary health care system is weakly developed and poorly functioning [5].
Studies on the benefits of integration of mental health services into primary care centres in India and Pakistan are inconclusive [6]. Most psychiatric patients in Pakistan bypass primary care services and access services at secondary and tertiary care centres directly, the primary reason being the questionable quality of services offered at these centres [7]. Additionally, in the absence of any kind of health insurance, most patients pay out of their own pocket [8]. In a study carried out at a tertiary care centre in Karachi, 68% of patients presented to psychiatrists for the first time. In the care pathway to mental health specialists, only 18% of patients had past contact with a primary care physician [9]. Although common mental disorders were diagnosed in one-third to a half of primary care attendees in India, primary care staff were reported to recognize only 10% of these cases [10].
The expertise of primary care physicians in the recognition of mental disorders is an important factor in the effective management of patients in primary care [11]. There is ample evidence of the benefits of early recognition and management of mental health problems from industrialized countries, where health systems are better developed. However, this needs to be studied systematically in the context of Pakistan, where the realities of health care delivery are quite different. In Pakistan almost 70% of health care services are provided by the private health care sector, therefore it is important to explore the opinion of these GPs regarding common psychiatric disorders. The objectives of this study therefore were to assess the knowledge and awareness of primary care physicians in Karachi, Pakistan, regarding the recognition and management of common psychiatric disorders and to gather their opinions about the care and services for patients with common mental disorders.
Methods
We conducted this study in 2 stages over a course of 9 months from April to December 2009. In the first stage, we carried out a survey over 6 months, mapping the GPs in Karachi, the largest metropolitan city in Pakistan in order to create a representative sampling frame of GPs. The primary reason for conducting the mapping exercise was that the existing lists of GPs available from various professional bodies in Pakistan were inaccurate. In the second stage, through a systematic sampling strategy, we randomly selected GPs to answer the questionnaire.
Sampling strategy
Assuming 50% prevalence (in the absence of any previous reference on GPs’ opinions in Pakistan), with 95% confidence level and ± 5% error the estimated sample size was 385 doctors. Using a reference database on the estimated population of practising physicians in the country [12] the sample size was adjusted to 352. The final sample size was increased to a round figure of 360 subjects.
The subjects were selected using cluster random sampling. Karachi city is divided into administrative 18 towns. Among these towns there are 178 union councils. The population of each union councils varies from 40 000–75 000 individuals according to the most recent census in 1998. In order to represent each of the 18 towns, 1 union council was selected randomly by ballot from each town. This created a sampling frame of 18 union councils. A list of all GPs practising in each of the councils was prepared, with separate codes assigned to other (alternative) care providers, in order to distinguish them from registered medical practitioners. Preliminary information, such as contact address and telephone numbers, nature and timing of practice were documented for these GPs, enabling us to construct a sampling frame of 1800 GPs. Then 20 GPs were enrolled from each union council, thereby generating a sample of 360 GPs.
Data collection
In the initial stage, we took permission from the city government officials and administrative officers in the charge of towns, after informing them of the study objectives. Two field surveyors carried out the first stage mapping of GPs. In the second stage, 2 research officers were recruited due to their past experience in data collection and each research officer approached the GPs for participation. The research officers were trained by the principal investigator (H.N.) in order to standardize the data collection procedure, enhance compliance and ensure the accuracy of information. A field coordinator supervised the overall project. He was instrumental in monitoring the initial survey of GPs in selected union councils, besides maintaining overall quality control through random checks. He also supervised the second stage data collection in the field. As part of the study protocol, we made 3 visits to the GPs in case of non-response. First and second visits were made by the research officer, while the field coordinator made the third and the last visit, noting down the concerns and reasons for non-participation. Despite these measures we encountered a refusal rate of 5%.
Questionnaire
The study questionnaire was developed by a focus group of psychiatrists and family physicians from the departments of psychiatry and family medicine at Aga Khan University. The study questionnaire was pre-tested and modified using 10% of the study sample size. It was administered to the identified GPs in the second stage of survey.
The questionnaire included information about GPs’ awareness of various psychiatric disorders in their routine practice. It also asked about the International Statistical Classification of Diseases and Related Health Problems (ICD-10) diagnostic criteria [13], treatment and referral difficulties and barriers to care. Individual characteristics of the practice that may have had an influence on the services rendered were collected. Some background information on the GPs was also included in the questionnaire. The section on medications assessed the GP's familiarity with a broad group of psychotropic medications. The choices included selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, serotonin and noradrenaline reuptake inhibitors (SNRIs), benzodiazepines, bupropion (wellbutrin®), buspirone, antipsychotics and mood stabilizers. Physicians were free to choose multiple responses, thereby generating response rates greater than 100%.
The ethics review committee of Aga Khan University Hospital reviewed the study protocol and granted permission to conduct it. The study was conducted in compliance with the ethical principles for medical research involving human subjects of the Helsinki Declaration.
Data analysis
Data was initially entered in the EpiData, version 3.1 then transferred to SPSS, version 15.0 for further analysis. Percentages of responses were calculated for relevant variables pertaining to knowledge and awareness. For categorical variables the chi-squared test of association was calculated, while for continuous variables Student t-test was used. The significance level was P < 0.05.
Results
In this survey we interviewed 360 GPs: 314 males and 43 females. The mean age of physicians was 44 (SD 10.4) years. They had been in practice for an average of 15 (SD 9.5) years. Table 1 shows the general characteristics of the GPs stratified by public or private sector medical college attended.
Type of clinics
A majority of the GPs (342, 95.0%) worked in private clinics where patients paid a fee for their services, while 4.8% of GPs were providing free services at welfare clinics affiliated with a nongovernmental organization or charity (Table 1).
Frequency of psychiatric disorders in general practice
The frequency of patients with mental disorders seen in their daily practice was reported to be up to 10% of their caseload by 71.8% of GPs and 11%–25% of their caseload by 10.3%. Surprisingly 12.9% of GPs denied seeing any psychiatric patients. When we inquired specifically about the frequency of patients with depressive disorders, 72.2% reported that around 1–5 patients daily had a depressive disorder and 13.6% reporting seeing 6–10 patients daily with depression. Only 6.4% of GPs denied seeing any patient with depression in their practice. This trend was somewhat similar for anxiety disorders: 70.6% participants reported seeing 1–5 patients, while 15.8% reported seeing 6–10 patients daily.
Awareness of diagnostic criteria
GPs’ knowledge about the ICD-10 diagnostic criteria for depressive disorder, generalized anxiety disorder, panic disorder, bipolar affective disorder and somatization disorder was assessed. Around two-thirds of GPs reported a lack of awareness with the ICD-10 diagnostic criteria for all these disorders (Table 2). Awareness of the ICD-10 criteria for depression was significantly better for among the 289 GPs graduating before 1999 (28.9%) compared with the 70 graduating in year 2000 or later (11.4%) (χ2 = 7.87, df = 2, P = 0.019).
Psychotropic medications in general practice
When asked about their knowledge of psychotropic medications 75.3% of GPs reported awareness of the benzodiazepine group (Table 3). The next most familiar drug groups were antipsychotics and mood stabilizers, cited by 50.6% and 43.5% of GPs respectively. Only 35.1% of GPs reported familiarity with SSRIs and only 20.2% with tricyclic antidepressants.
Figure 1 illustrates the physicians’ choice of medications for various psychiatric disorders. Benzodiazepines were the first choice of medication for all conditions and 52.3% of GPs reported using them in the treatment of depression. The next most commonly choice for depression were SSRIs, antipsychotics, mood stabilizers and tricyclic antidepressants, cited by 31.6%, 27.1% and 20.9% GPs, respectively. The correctness of responses were compared with American Psychiatric Association guidelines. When we grouped the drugs into potentially correct (SSRIs, SNRIs, tricyclic antidepressants and bupropion) and incorrect (benzodiazepines, mood stabilizers, antipsychotics and buspirone) choices 42.2% of GPs chose a suitable drug. GPs graduating before the year 2000 were significantly more likely to be correct than those graduating after 2000 (45.2% versus 30.0%) (χ2 = 5.321, df = 2, P = 0.021)
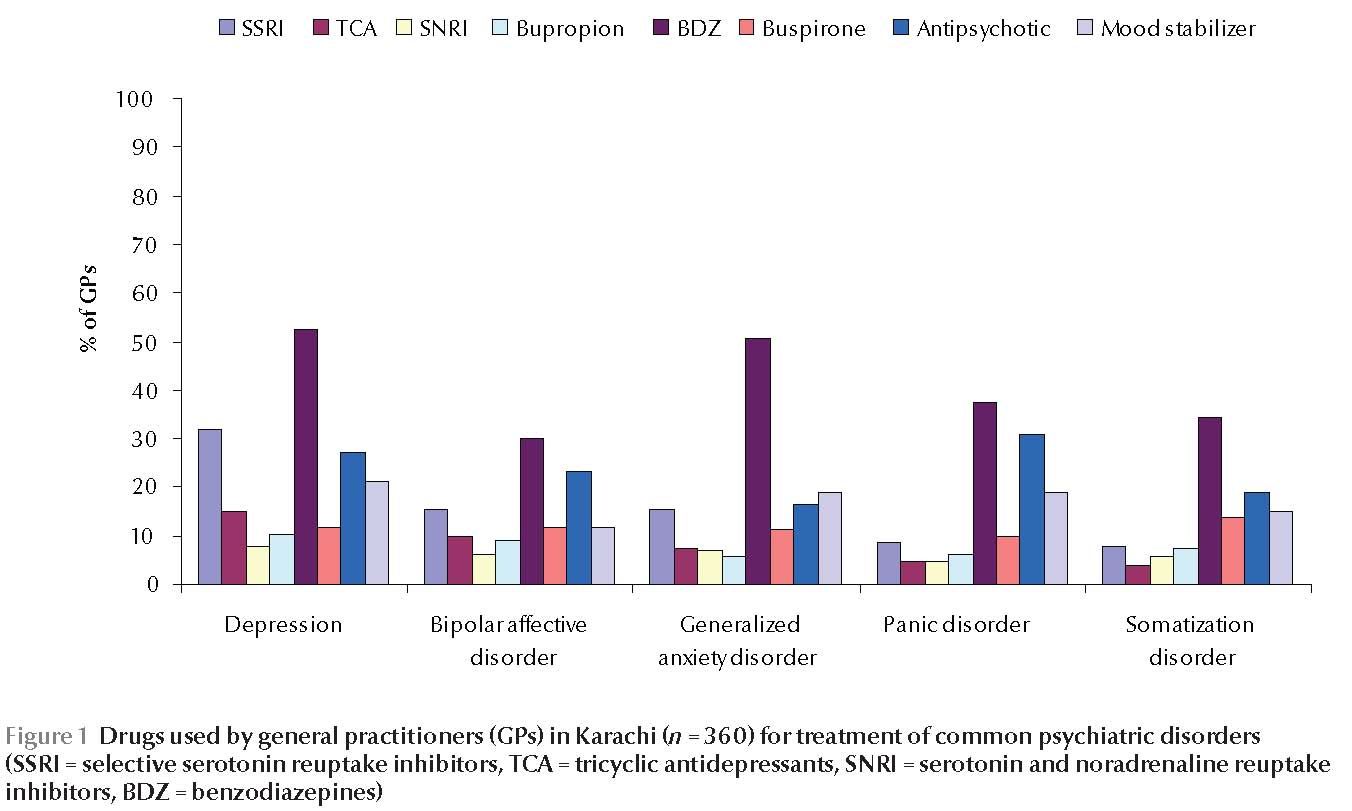
When asked about the choice of medication for bipolar disorder, benzodiazepines were cited by 30.1% physicians and antipsychotics and mood stabilizers by only 23.0% and 11.4% physicians. However, 40% reported that they did not know which medication to prescribe in the treatment of bipolar affective disorder. When we grouped the responses into potentially correct (antipsychotics and mood stabilizers) and incorrect responses (other medications), an overwhelming majority of GPs (71.7%) made a wrong choice of medication.
For the treatment of generalized anxiety disorder benzodiazepines were again the most favoured drugs, chosen by 50.7% of GPs, and SSRIs was chosen by only 15.4% of GPs. However, there were more correct (63.3%) than incorrect (36.7%) choices when drug categories were grouped. This was not a surprise since GPs could select any of the 6 drug groups (SSRIs, tricyclic antidepressants, SNRIs, benzodiazepines, bupropion and buspirone) in order to score a correct answer.
In the medication of choice for panic disorder benzodiazepines were again cited by 37.3% physicians. Antipsychotics and mood stabilizers were cited by 30.8% and 18.8% of GPs, respectively, while only 8.5% cited SSRIs as the treatment of choice and 34.5% did not know which medication to prescribe for panic disorder. Overall, 60.6% gave an incorrect response when the choices were dichotomized into correct and incorrect.
The last question on the choice of medication was about treatment of somatization disorder. Although 47.9% GPs reported that they did not know which medication to prescribe, 34.3% chose benzodiazepines in this category too. Antipsychotics (18.7%), mood stabilizers (15.0%), buspirone (13.6%) and SSRIs (7.6%) were the other choices for treatment of somatization disorder.
Other treatment modalities
When asked if they used any other treatment modality besides medications 74.4% GPs reported that they employed counselling themselves, while 8.6% gave “general advice” regarding health. Two GPs reported that they used “spiritual advice” as a treatment modality. The remaining physicians reported that they preferred to refer patients after the initial treatment. When asked whether they considered their treatment to be effective or not, 71.4% believed that their treatments were effective, while 8.3% reported it was not and 9.7% were not sure.
Treatment difficulties and referrals
When asked if they encountered difficulties in managing patients with mental disorder 86.7% agreed that they had difficulties. The type of difficulties GPs experiences were grouped into physician- and patient-related factors. Lack of time and lack of interest were the main physician-related factors, mentioned by 84.6% and 26.0% physicians respectively (Figure 2).
A minority (16.0%) reported that their own lack of knowledge about management of mental disorders was the main difficulty in providing care. Among patient-related factors, 58.0% of GPs reported that patients’ refusal for the treatment was the main issue.
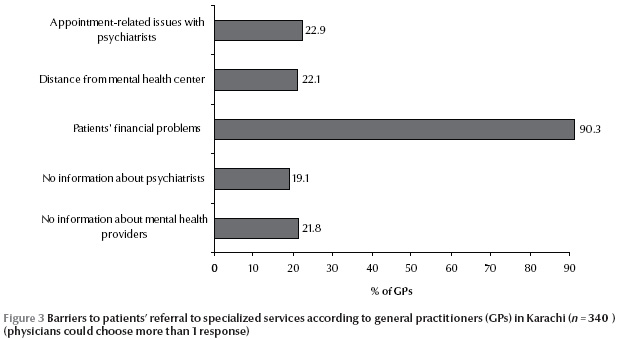
There were some interesting responses when we asked about the type of patients that were generally referred to specialist services. The majority of GPs cited patients displaying violence towards others (83.8%), violence towards self (72.2%) and psychoses (70.4%). Sexual disorders were a low priority for referral, cited by only 23.4% physicians. When asked about the difficulties encountered in referring patients to specialized services, 90.3% of GPs reported patients’ financial constraints as the major impediment (Figure 3).
Continuing medical education
We asked if they felt that their knowledge and expertise was sufficient to treat their patients with mental disorders. A majority of GPs (74.7%) believed that they lacked information in this specialized area, while 10.6% thought that had enough expertise in managing patients with mental disorders and 14.2% were unsure. When asked if they had attended any seminars, workshops or continuous education programmes about mental disorders during the last 3 years 69.2% reported that they had not, while 30.6% had had some form of continuing medical education. Finally, we enquired if they would like to attend a course on management of mental disorders in general practice; 48.9% showed interest in attending such a course, while the rest felt no need for it.
Discussion
It is not realistic to refer all patients with psychiatric problems to specialist services, nor is this desirable. Many patients with depression and anxiety, as well as other disorders, can be managed well by primary care physicians who are motivated to provide care. This is the first study from Pakistan which examined the knowledge and awareness about common psychiatric disorders among GPs in the private health care sector, which provides almost 70% of health care services in the country. The key findings of our study are that GPs lacked knowledge of internationally recognized diagnostic categories for mental disorders and that their choice of drugs for these disorders was not based on standard treatment practice. Although GPs reported that they did not have enough time for the management of mental disorders, they also believed that patients were unable to afford to attend specialist psychiatric services. A great majority of our GPs had not attended any form of continuing medical education about mental disorders in general practice. Furthermore, psychiatry is not taught and examined as an essential undergraduate subject in most medical colleges in Pakistan. These gaps in GPs’ knowledge and education have implications for the rational use of psychotropic medications in primary care and for the quality of care delivered in general.
We identified substantial gaps in physicians’ knowledge and understanding of mental disorders and their management in primary care. The fact that 63.6% of GPs were unaware of the ICD-10 diagnostic criteria for depression and anxiety is concerning. In Pakistan, where prevalence estimates of depression and anxiety are reported to be around 30% to 50%, non-recognition of these problems can have serious consequences [14]. Even in situations when these conditions were recognized, the lack of adequate knowledge regarding management strategies is concerning.
The fact that benzodiazepines were the most familiar drugs to three-quarters of surveyed GPs, and were prescribed for the treatment of depression by 52.3% of them, has serious public health implications. The irrational use of psychotropic medication, however, is not limited to benzodiazepines alone. That 30.8% of GPs in our survey considered using antipsychotics for the treatment of panic attacks is also alarming, so too is the use of antipsychotics for the treatment depression by 27.1% of GPs. Somatization disorder was another category in which various psychotropic medications were prescribed incorrectly. A previous study from our centre showed that patients who were prescribed psychotropic medications knew less about the effects, side-effects and hazards of their use compared with those who were prescribed other medications [15].
Data from the National Ambulatory Medical Care Survey in the United States also supports our observations [16]. In their reports, general and family practitioners wrote psychotropic drug prescriptions in 84 per 1000 patient visits, in contrast to psychiatrists who had a rate of 441 per 1000 visits. The allegations that primary care physicians prescribe psychotropic drugs inappropriately may be correct in part, but it is also likely that these physicians are treating very different patients than those seen by specialists. In a study from the United Kingdom, exploring the reasons behind psychotropic drug prescriptions, Hyde et al. concluded that GPs used symptom severity (as measured on the General Health Questionnaire) for deciding who received treatment for depression and anxiety [17].
This survey has a few limitations which should be kept in mind while interpreting the results of this study. This was an opinion survey, in which GPs were asked to give their views on the frequency of common disorders in their own practice. Like all self-reported surveys, we have no way of knowing if their assessments were correct. The primary reasons for conducting an opinion survey rather than an objective assessment was to build the trust and confidence of the GPs, thereby establishing a link with specialist services. In the initial stages of the survey, GPs expressed apprehension about the research study and the implications of the findings on their daily practice. However, they were reassured that the survey would not have any negative bearing on their practice, only that they would receive regular communications on various continuous medical education programmes for primary care physicians. Finally, one possible reason for the under-recognition of antidepressants could be that we asked about the generic names of drug groups, rather than using the specific brand names.
Further research is needed to explore the prevalence estimates of common psychiatric conditions from a representative sample base of general practice throughout Pakistan. The prescription of psychotropic medications, especially benzodiazepines, also needs to be studied systematically. There is an urgent need to study the cost-effectiveness of managing mental disorders in primary care in countries such as Pakistan, which have a dearth of resources.
Acknowledgements
We like to acknowledge the contribution of Mr Sajid Reza Shah, field coordinator, whose untiring efforts and commitment to the field work, in very testing times, made this survey possible. We would also like to acknowledge the administrative support of Mr Dominic Dsouza, administrative officer, Department of Psychiatry, Aga Khan University.
References
- World health report 2001. Mental health: new understanding, new hope. Geneva, World Health Organization, 2001.
- Golderg D et al. The treatment of common mental disorders by a community team based in primary care: a cost effectiveness study. Psychological Medicine, 1996, 26:487–492.
- Goldberg D. Psychiatry and primary care. World Psychiatry; Official Journal of the World Psychiatric Association, 2003, 2:153–157.
- Patel V et al. Mental health services in primary care in ‘developing’ countries. World Psychiatry; Official Journal of the World Psychiatric Association, 2003, 2:163–164.
- Khattak FH. Health economics and planning in Pakistan. Islamabad, Ad-Rays Publishers, 1996.
- James S et al. Demand for, Access to and use of community mental health care: Lesson from a demonstration project from India and Pakistan. International Journal of Social Psychiatry, 2002, 48:163–176.
- Chisolm D et al. Integration of mental health care in to primary care: demonstration cost-outcome study in India and Pakistan. British Journal of Psychiatry, 2000, 176:581–588.
- Statistical annex. In: World health report 2004. Changing history. Geneva, World Health Organization, 2004.
- Naqvi HA et al. Pathway to psychiatric care in Karachi. Journal of the College of Physicians and Surgeons of Pakistan, 2006, 16:438–439.
- Patel V et al. Somatic and psychological models of common mental disorder in primary care in India. Psychological Medicine, 1998, 28:135–143.
- Jencks SF. Recognition of mental distress and diagnosis of mental disorder in primary care. Journal of the American Medical Association, 1985, 253:1903–1907.
- Karachi city: physicians’ directory, 2005. Medi Publications [website] (http://www.urdf.net/paksehat/index.htm/, accessed 21 March 2012).
- International statistical classification of diseases and related health problems, 10th revision. Geneva, World Health Organization, 1993.
- Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: systematic review. British Medical Journal, 2004, 328:794–797.
- Ganatra HA et al. Educating and informing patients receiving psychopharmacological medications: are family physicians in Pakistan up to the task? PLoS ONE, 2009, 4:e4620.
- Mechanic D. Treating mental illness: generalists versus specialists. Health Affairs, 1990, 2:61–75.
- Hyde J et al. Deciding who gets the treatment for depression and anxiety: a study of consecutive GP attendees. British Journal of General Practice, 2005, 55:846–853.


