Case report
V. German,1 N. Papadopoulos,1 C. Diakalis,1 C. Goritsas1 and A. Ferti1
Introduction
Brucellosis is a zoonotic infection with a worldwide distribution, endemic in the Mediterranean region, and is associated with high morbidity in humans [1,2]. Osteoarticular complications are the most common focal complications of Brucella spp. infection [3]. These complications commonly affect the axial skeleton, with vertebral spondylitis accounting for 35%–50% of all osteoarticular complications [4–6]. Estimates of the incidence of spondylitis range from 9% to 31% [4,5]. While lumbar spine involvement is the most common, cervical involvement is a rare, but more severe, complication, accounting for 8.3% of cases of vertebral osteomyelitis in a recent study [4].
We present a case of brucellar spondylitis with paravertebral mass in the cervical segment that resulted in neurological deficits.
Case report
A 36-year-old female patient, a veterinarian who was working and living in Albania, with a history of nephrolithiasis and an unremarkable family history, presented at our hospital with high fever that had started 20 days previously. Coexisting symptoms were night sweats, headache, neck pain extending down the back, and myalgias, especially in the right arm.
The patient had initially been treated by a general practitioner with ciprofloxacin for 1 week, followed by ampicillin and streptomycin for 4 days with apparently no remission of the symptoms. The Wright test was reported as negative at that time. The patient presented at the Sotiria General Hospital for Chest Diseases in Athens with persistent high fever (up to 39.8 C), neck and back pain, myalgias and restricted movement of the right arm.
Physical examination revealed nothing but cervical spine tenderness at C4–C6, while neurological examination revealed a decrease in strength in the right biceps and triceps, with attenuation of their reflexes.
Laboratory results showed an erythrocyte sedimentation rate of 99 mm/h, a leukocyte count of 9480 /mm3 with 49% neutrophils and 32% lymphocytes, a haemoglobin level of 11.8 g/dL and a platelet count of 348 000 /mm3. Liver function tests were abnormal: alkaline phosphatase 1484 U/L, gamma-glutamyl-transpeptidase 443 U/L, serum glutamic oxaloacetic transaminase 134 U/L, serum glutamic pyruvic transaminase 324 U/L and lactate dehydrogenase 348 U/L. Blood urea, creatinine, total bilirubin and electrolyte levels were normal. Four consecutive blood cultures were negative. There was a diffuse hypergammaglobulinaemia and an increase in C-reactive protein value to 3.41 mg/L (normal value < 0.8 mg/L). Tests for rheumatoid factor and antinuclear antibodies, the tuberculin skin test and Wright agglutination test were all negative.
Brucella infection was confirmed with a positive result for Brucella IgM antibodies (> 100 U/mL) using an enzyme-linked immunsorbent assay (Serion Immundiagnostica GmbH, Germany).
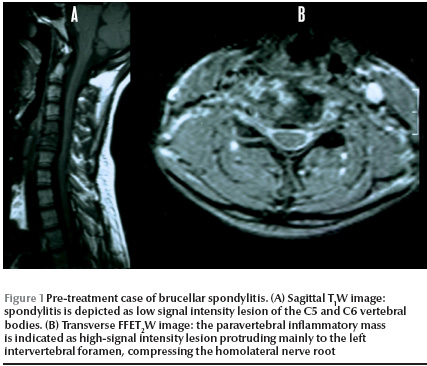
Cervical spine X-ray showed narrowed C5–C6 and C6–C7 intravertebral spaces and a possible paravertebral anterior mass in the C6–C7 area. Thoracic spine X-ray had no abnormal findings. A cervical spine computerized tomography (CT) scan consequently performed revealed spondylodiscitis in the C5–C6 intravertebral space, with destructive changes in the C5 vertebral body and presence of tissue in the right lateral paravertebral space. Cervical magnetic resonance imaging (MRI) confirmed the C5–C6 spondylitis and the existence of a minimal inflammatory paravertebral mass with root compression (Figure 1 ). The patient underwent a CT guided fine-needle aspiration of the abscess. Histological examination revealed a nonspecific inflammatory infiltration with no evidence of malignancy. All culture tests were negative.
The patient was started on oral doxycycline 100 mg 2 × day, oral rifampicin 600 mg daily and intramuscular streptomycin 1 g 4 × day. The doxycycline and rifampicin regimen continued for a period of 3 months and streptomycin was discontinued after 2 weeks. Thirty days after admission, the patient was discharged free of symptoms with amelioration of the neurological signs. The laboratory tests on her discharge were normal, including erythrocyte sedimentation rate and liver function tests.
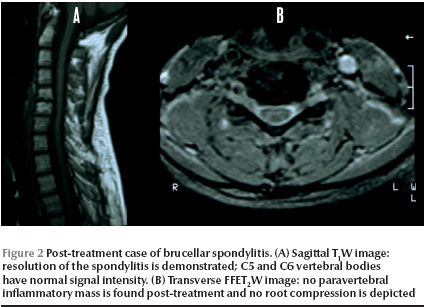
Three months after discharge the patient remained free of symptoms, neurological examination was normal and complete laboratory tests were within normal limits with a decrease in the anti-Brucella IgM antibody titre to 50 IU/mL. A second cervical MRI showed remission of spondylitis with no evidence of the paravertebral mass (Figure 2).
Discussion
Brucellosis remains an important public health problem in the Mediterranean region, where efforts to eradicate Brucella melitensis in animals have failed. In Greece, 284 cases of brucellosis were officially reported during 2006 [7].
The clinical manifestations of brucellosis are varied. The musculoskeletal system is frequently affected and the spine is the most common site of bone brucellosis. The spine is most frequently affected in the lumbosacral region, and patients are usually males over the age of 50 years [1,4,5]. Cervical involvement, however, is accompanied by more severe manifestations, such as paravertebral and epidural masses, neurological and functional disabilities [1,5].
Diagnosis and treatment should be quick and intense, since delay in treatment leads to a high morbidity rate. In a multicentre prospective study of 593 patients with brucellosis. the incidence of spondylitis was 9.7% [5]. The incidence of medulla or root compression, however, depended on the affected segment of the spinal column. In the group of patients with cervical spondylitis, 71% had compression of the medulla or roots, versus 11% and 21% in the dorsal and lumbar group respectively. In addition, patients with cervical and dorsal spondylitis had a significantly higher rate of paravertebral or epidural masses than those in the lumbar group. Moreover, there were a significantly higher number of patients with unsatisfactory progress in the cervical group compared with the dorsal and lumbar groups. Recent studies in Greece found osteoarticular involvement in nearly half the cases of acute brucellosis [2,8].
Occasionally patients with paravertebral abscess fail to respond to conservative treatment and have to undergo surgery [1,9]; however, success has been reported with conservative treatment, and this may be sufficient in selected patients [10]. Generally, little information is available about brucellar spondylitis and treatment regimens vary widely. The Ioannina recommendations, developed by experts in November 2006, advised that the outcome of spondylitis may be improved when a streptomycin regimen is used and that the duration of therapy must be not less than 3 months [11].
In a recent study of 918 patients with brucellosis, the incidence of vertebral osteomyelitis was 10.4%, and cervical involvement was established in 8.3% of them [4]. In that study patients were treated with doxycycline for 3 months plus streptomycin for 2 or 3 weeks (DOX-STR regimen) or doxycycline plus rifampicin (DOX-RIF regimen) both for 3 months. No significant differences were found between the 2 treatment groups in treatment failure, mortality and relapse. In our case, we preferred to use initially streptomycin for 2 weeks plus doxycycline and rifampicin for a total of 3 months. The administration of triple regimens is used for neurobrucellosis [2]. We believe that this treatment strategy combines the superiority of the DOX-STR regimen with the better implementation of the oral DOX-RIF regimen. However, more well-designed, controlled trials are needed to establish the superiority of a certain regimen. Currently therapeutic decisions are guided mainly by expert opinion. In our case there was a rapid response to antimicrobial chemotherapy, as was reported in previous cases of brucellar spondylitis with paravertebral abscess [6,12].
Cervical spondylitis should be considered a severe complication of brucellosis; therefore its treatment and follow-up must be energetic in order to detect and correct as early as possible compressions of the neural axis and its roots. Treatment should be prolonged to prevent both complications and relapses. Further evaluation in controlled studies is needed to assess the efficacy and safety of treatment options in brucellar spondylitis.
References
- Solera J et al. Brucellar spondylitis: review of 35 cases and literature survey. Clinical infectious diseases, 1999, 29:1440–9.
- Pappas G et al. Brucellosis. New England journal of medicine, 2005, 352(22):2325–36.
- Colmenero JD et al. Complications associated with Brucella melitensis infection: a study of 530 cases. Medicine, 1996, 75:195–211.
- Colmenero JD et al. Clinical findings, therapeutic approach, and outcome of brucellar vertebral osteomyelitis. Clinical infectious diseases, 2008, 46:426–33.
- Colmenero JD et al. Clinical course and prognosis of brucella spondylitis. Infection, 1992, 20:38–42.
- Basaranoglu M et al. A case of cervical brucella spondylitis with paravertebral abscess and neurological deficits. Scandinavian journal of infectious diseases, 1999, 31:214–5.
- Epidemiologic data for infectious diseases. Athens, Hellenic Centre for Infectious Diseases Control, Department of Epidemiological Surveillance and Intervention [website] (http://www.keel.org.gr, accessed 12 October 2009).
- Andriopoulos P et al. Acute brucellosis: presentation, diagnosis, and treatment of 144 cases. International journal of infectious diseases, 2007, 11:52–7.
- Tekkok IH et al. Brucellosis of the spine. Neurosurgery, 1993, 33:838–44.
- Guzey FK et al. Cervical spinal brucellosis causing epidural and prevertebral abscesses and spinal cord compression: a case report. Spine journal, 2007, 7:240–4.
- Ariza J et al. Perspectives for the treatment of brucellosis in the 21st century: the Ioannina recommendations. Public Library of Science medicine, 2007, 4(12):1872–8.
- Malavolta N et al. Brucella spondylitis with paravertebral abscess due to Brucella melitensis infection: a case report. Drugs under experimental and clinical research, 2002, 28:95–8.
Eastern Mediterranean Approach to Noncommunicable Diseases
Chronic diseases such as cardiovascular, diabetes, cancer, renal, genetic and respiratory conditions are rising dramatically in the Eastern Mediterranean Region. Currently, 45% of the region’s disease burden is due to noncommunicable diseases. It is expected that this burden will rise to 60% by the year 2020. The impact of these conditions falls heavily on the region’s poor and marginalized populations.
The Eastern Mediterranean Approach to Noncommunicable Diseases has the overall objective to improve the health of populations of the Region by reducing mortality and morbidity from major NCDs through an integrated collaborative intervention programme of prevention and health promotion.
Further information about the work of EMRO in tackling noncommunicable diseases s is available at: http://www.emro.who.int/ncd/ncd_introduction.htm


