Report
S. Shawky 1
الرعاية الصحية الأولية في إقليم شرق المتوسط: من ألما آتا إلى الدوحة
شيرين شوقي
الخلاصـة: في الاحتفال بالذكرى الثلاثين لإعلان ألما آتا في المؤتمر الدولي حول الرعاية الصحية الأولية الذي أقيم في الدوحة، تجدَّد التزام إقليم شرق المتوسط بالرعاية الصحية باعتبارها الوسيلة لتحقيق صحة أفضل. ولاتزال المبادئ التي حظيت بالاتفاق عليها في ألما آتا عام 1978 تَنْطَبق اليوم كما كانت من قبل. وقد قدَّم هذا المؤتمر فرصة لبلدان إقليم شرق المتوسط لتحديد التوجُّهات المستقبلية لتوجيه النظم الصحية نحو إدماج الرعاية الصحية الأولية، واتباع أسلوب العمل المتعدد القطاعات.
ABSTRACT The celebration in Doha of the 30th anniversary of the Alma-Ata Declaration at the International Conference on Primary Health Care renewed the commitment of the Eastern Mediterranean Region to primary health care as the tool for better health. The principles agreed at Alma-Ata in 1978 apply as much now as they did before. The event provided an opportunity for the Eastern Mediterranean countries to define future directions to steer the health systems to integrate primary health care and harness the intersectoral approach.
Les soins de santé primaires dans la Région de la Méditerranée orientale : d’Alma-Ata à Doha
RÉSUMÉ À l’occasion de la célébration à Doha du trentième anniversaire de la Déclaration d’Alma-Ata, lors de la Conférence internationale sur les soins de santé primaires, la Région de la Méditerranée orientale a renouvelé son engagement en faveur des soins de santé primaires en tant qu’outils pour l’amélioration de la santé. Les principes adoptés à Alma-Ata en 1978 restent, aujourd’hui comme hier, d’actualité. L’événement a fourni une occasion pour les pays de la Méditerranée orientale de convenir de nouvelles orientations pour guider les systèmes de santé, intégrer les soins de santé primaires et mettre en oeuvre l’approche intersectorielle.
1Social Research Center, American University in Cairo, Cairo, Egypt (Correspondence to S. Shawky:
Received: 25/03/09; accepted: 03/06/09
EMHJ, 2010, 16(12): 1285-1289
Introduction
On 1–4 November 2008 in Doha, the capital of Qatar, the countries of the Eastern Mediterranean Region (EMR) celebrated the 30th anniversary of the Alma-Ata Declaration with the International Conference on Primary Health Care: The foundation for health and wellbeing [1]. The event was an important occasion, assembling numerous health professionals to share their global and regional experiences and plan future directions. The main goal of the conference was to develop action-oriented recommendations to harness the potential of the primary health care (PHC) approach in safeguarding health and wellbeing. The Doha conference reaffirmed the World Health Organization’s (WHO) definition of health and renewed the health community’s commitment to the Alma-Ata vision [2] which shifted health care away from a focus on hospital care and the biomedical model. The event underlined the importance of looking at regional needs in order to steer health systems towards better performance and greater equity and ensuring the role of PHC as the tool for achieving the goal of “health for all”.
PHC was adopted as an ideal to strive for in most EMR countries soon after the Alma-Ata Declaration, with the aims of limiting health sector expenditure, using resources more efficiently, improving health care and reducing health inequities. The past few decades have seen increasing political attention in the Region on PHC, with an active focus on health sector reforms that integrate PHC within national health systems and a push for broader economic structuring, with countries implementing health sector reforms and looking for mechanisms to increase their health system’s financing and strategies to mobilize financial resources. The evidence, however, paints a different picture of PHC in the Region: as a vision that did not fully achieve its goals. Recent statistics reveal that the EMR countries are still lagging behind other countries in achieving health equity, in facing the new health threats and in reducing expenditure on health through building insurance systems [3,4]. Despite notable improvements in the overall health of people in the Region, the health indicators are skewed towards the most favoured groups in the population. The Region suffers from new health threats, among which HIV infection is one of the most concerning [5]. The cost of health services are mounting, health insurance systems are in their infancy and many people are at risk of catastrophic payments.
The regional and international commitment to revitalize the role of PHC and support health and wellbeing in EMR provide a unique opportunity to review the evolution of health concepts and the Alma-Ata vision [1,6]. These aim to highlight the issues and challenges facing the development of PHC in the EMR in an attempt to map out future directions for supporting population health and well-being in the Region.
Evolution of health concepts
In the past, “health” referred to the absence of disease. Progress in health since the early years of the 20th century alerted the scientific community to the idea that health needs to be thought of as much broader than just absence of disease. WHO called for a shift from this focus on curing disease towards the concept of health balance through preserving health for the healthy and restoring health for the unhealthy. WHO has defined 2 main dimensions to maintaining the health balance: building health potential and health protection.
The new direction liberated the concept of health from the narrow continuum of disease and medicine to the WHO broader definition of health in 1946 as: “a state of complete, physical, social and mental well-being and not merely the absence of disease or infirmity”. The definition was a revolution from earlier concepts that spelt out health in a social context. However, this new vision was challenged by breakthroughs in health technology during the 1950s that produced an array of new antibiotics, vaccines and other medicines, instilling the belief among health professionals and the general public that technology held the answer to all the world’s health problems. This was coupled with a global trend towards the realization that the medical model was not meeting the most urgent needs of the poor and disadvantaged populations. It was clear that the advanced curative technologies were distorting the health systems in many countries, especially those in the developing world.
The new health perspective was revitalized by the landmark WHO and UNICEF international conference in Alma-Ata in 1978. The main goal was to discuss the urgent problem of providing people with the right to life and health. The participants stressed the responsibility that governments have for the health of their people. The conference underlined the importance of social and economic development, as well as the political independence for completely realizing the mission of health development. The triumph of the event was the adoption of the Alma-Ata Declaration: the 20th century’s key health charter [2]. The Alma-Ata Declaration had two major achievements: defining the goal “Health for All by the year 2000” and identifying PHC as its tool.
The Health for All policy ushered in a new era in health and a new vision of the disease panorama. The redefinition of health removed the focus on hospitals and the biomedical model of health care. It called for a broader sociopolitical orientation for health policy, encompassing a broad social and economic development context. It gave prominence to the need for action from many other social and economic sectors in addition to the health sector. The core idea of the Alma-Ata Declaration was to administer the Health for All policy under the concept of PHC. PHC was viewed as a major tool in implementing the WHO strategy and the key for achieving the goal of Health for All, thus, contributing to health development in an integrated comprehensive, intersectoral and participatory approach through efficient and equitable health systems. The Health for All framework set the ground for reform in the national public health policies of WHO member states. The reference to the year 2000 meant that, as of that date, all the countries would have developed the appropriate political strategies and be enacting concrete measures towards achieving the goal of Health for All.
WHO saw clearly the value of PHC and began to promote it around the world. The 1990s saw increasing scientific advances in understanding the social determinants of health. In 2000, the United Nations Millennium Summit set ambitious targets to tackle the root causes of ill health and the Millennium Development Goals were adopted by the 189 member states [7]. In the same context, the Commission on Social Determinants of Health was founded in 2005 as an attempt to revive the foundation for health equity, the efficiency of health systems and intersectoral action for health [8]. All these initiatives agreed on the need for an integrated PHC system within a comprehensive national health system as the best way to tackle health problems in communities and for people to access health care.
Primary health care concepts and mission
The definition of PHC proposed 30 years ago rests on 3 pillars (Figure 1). First, care must be essential, providing comprehensive, continuous and quality care that meets the actual health needs of the community. Secondly, care should be accessible through geographical, social and functional accessibility. Thirdly, care needs to be affordable within the available resources.
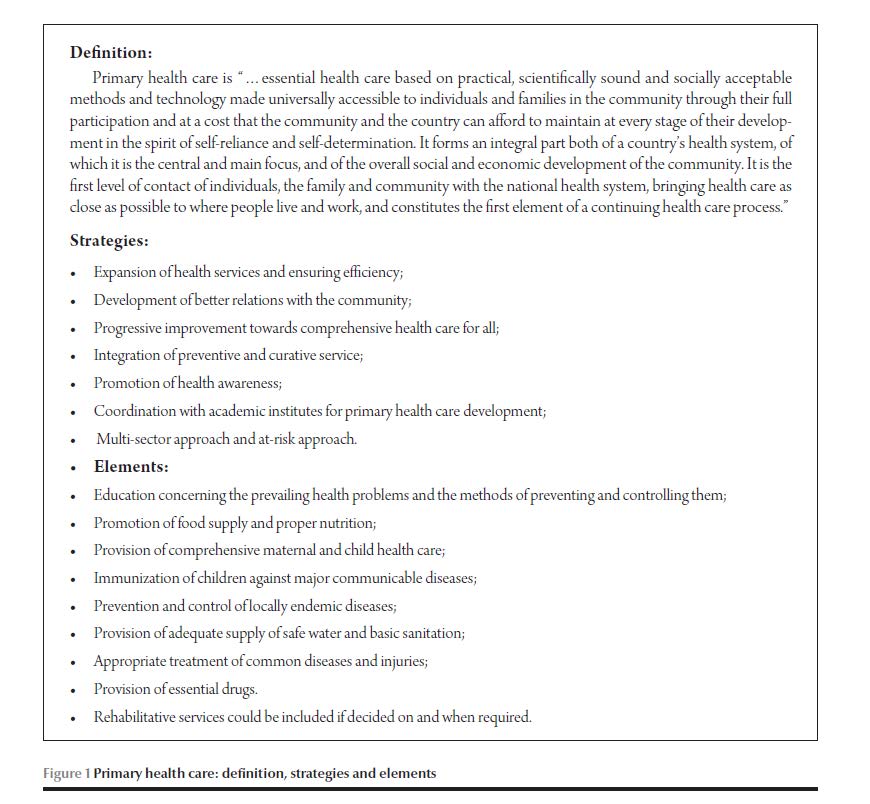
PHC aimed to be context-specific to meet the actual priority community needs, the stage of socioeconomic and health development and the available resources in a community or a country. In this context, 6 strategies and 8 elements were defined to shape the PHC mission (Figure 1). The strategies of PHC and the delivery of its elements are organized on the basis of equity in distribution, appropriate technology, intersectoral approaches and community participation. The mission of PHC is completed by its instruments, including community surveys and diagnosis, family health records, plans of action, the team approach and health information systems.
This emphasis on PHC has reshaped health systems worldwide to cope with their new broader role. Within any health system, the PHC concept has several responsibilities that are linked to the medical and non-medical sectors. Within PHC there is a responsibility to provide individual diagnosis and health care services through primary medical care, focusing on minor illness and prevention of diseases. It has a screening function for the early detection of patients who need a higher level of medical care, thus acting as a referral system. PHC involves a community responsibility to provide a diagnosis of community needs and services through surveillance systems, surveys, outreach programmes, community empowerment programmes and building health databases. PHC also includes a responsibility to mobilize intersectoral actions and oversee the services provided by other non-health sectors for promotion of health and wellbeing.
Primary health care issues in the EMR
It is apparent that there is an active movement towards PHC in the EMR. The Region can point to many success stories. However, an in-depth look at the Region reveals a common issue. While the mission of PHC is to target health and wellbeing, PHC in the Region is still skewed towards the biomedical model. The intersectoral approach is lagging behind, with many PHC instruments blocked and several elements lacking. The PHC package in this case acts only as primary medical care with a patient–doctor approach and disease focus.
This half-finished development of PHC is illustrated by 3 main issues. Firstly, most PHC settings are only applying a family health model. It is true that the family model has a broad health vision that looks at an individual within the family. Integration of a family health model within a PHC setting is an asset that can effectively and efficiently reduce the need for, and relieve the burden on, referral systems. Nevertheless, the family approach does not encompass all components of PHC. For example, the family health approach is not applicable to initiatives such as surveillance systems, community surveys and diagnosis, control of endemic diseases, health information systems and community empowerment, all of which require a community approach with intersectoral action.
Secondly, the role of PHC in monitoring population health and controlling emerging diseases is hampered by the numerous disease-specific programmes running independently outside of PHC settings in the Region.
Thirdly, recent years have seen the setting up of huge number of different initiatives in the Region, for example maternal and child health, reproductive health, community-based, women’s empowerment and poverty alleviation programmes. Although these programmes represent important elements of PHC, each is working on its own, detached from the PHC context. This risks depriving the PHC system of its responsibilities and functions, encouraging weak and fragmented health systems, and delays the initiation of intersectoral actions.
Health care challenges in the EMR
The 3 major challenges concerning PHC in the EMR countries are how to stimulate an intersectoral approach, how to utilize human capacities and how to secure funding.
A common feature in all EMR countries is the lack of an intersectoral approach to PHC. The blame for this can be attributed to both the national and international communities. On a national level, government sectors are accustomed to working independently. The ministries of health are still believed to be uniquely responsible for population health. The other non-health sectors rarely pay attention to the health outcomes of their policies and interventions. NGOs and civil society are struggling for population health; however, they are rarely engaged in intersectoral actions. On the international level, each international organization has links with a specific sector, whether government sector or civil society. The international aid programmes are directed to a single sector and there are no international aid investments or programmes that have an intersectoral model with a mechanism for budget sharing.
The countries of the Region lack the health professionals who can lead a health system integrated with PHC [9–12]. Integrated PHC systems need 3 main types of professional: public health professionals to plan, manage and organize the health system; community health professionals to work on community diagnosis and manage PHC with a community-based approach; and family health professionals to provide primary care. There are several reasons for this. First, education in public health is deficient in most countries of the Region, and in countries where it does exist the number of public health professionals is inadequate for the size and health needs of the population. Second, while community health education is available in most medical schools and schools of health sciences, PHC education is rarely integrated into the community health curriculum. Even though there are many community health professionals, their role is ill-defined or is confused with public health or family health and there is a limited labour market. Third, in several countries of the Region, family health education does not exist. To solve this problem in settings where the family model leads PHC, some countries have trained general practitioners on family health for a few months, although there are many doubts about the success of this experience.
PHC funding is a function of government subsidies and beneficiary’s contributions. Government inputs to PHC in the Region are limited as ministries of health give priority to hospital care and curative technology. The beneficiaries pay their share, either as service fees or through membership of a family fund, or a package of both. The PHC out-of-pocket cost overburdens the people, especially the poor, who are forced to seek health care in public hospitals at lower cost. Although PHC is a global responsibility, international aid investments are mainly allocated to detached, disease-specific vertical programmes or community programmes, thus depriving PHC of a likely funding source.
Future directions in the EMR
Integrated PHC health systems remain a key goal of health policy. It is time that EMR countries steered their health systems towards this goal with well-planned steps that build on positive achievements and mitigate the shortcomings in the implementation of PHC. Three broad future directions are recommended to nurture the role of PHC: defining an operational model for intersectoral action, generating human resources and securing financing for PHC.
First, the EMR countries are invited to initiate a vigorous dialogue among all relevant stakeholders to reach a consensus on strategies to support and organize intersectoral action. Strategies designed with the focus on equity, working within the framework of social determinants of health and a budget-sharing mechanism will provide the best base for defining an operational intersectoral model. The Region can go further and test the model on a country level, identify success stories that can be improved on and used on a wider scale as a model for the Region.
Second, the EMR countries need to strengthen their health education programmes and direct them towards meeting community health needs. The Region needs to set up more schools of public health independent from the medical schools. Schools of public health are distinct from medical schools in offering multidisciplinary education to students from diverse disciplines. Countries need to build capacity in family health through enforcing family health education in schools of medicine and allied health sciences. Countries need to revisit the community health curriculum in schools of medicine and allied health sciences in order to integrate PHC as a key component and define the true role of community health education.
Third, there is a need for stakeholders to take action towards institutionalizing vertical programmes, outreach activities and community-based initiatives within PHC. On the one hand this will support the PHC system to fulfil its responsibilities and on the other it will offer more funding opportunities for PHC. This action is best complemented by developing a workable social health insurance structure that guarantees universal coverage and risk pooling.
References
- The foundation for health and wellbeing. International Conference on Primary Health Care, Doha, Qatar, 1–4 November 2008.
- International Conference on Primary Health Care: Declaration of Alma-Ata. Alma-Ata, USSR, 6–12 September 1978.
- WHO Statistical Information System (WHOSIS). Geneva, World Health Organization [website] (http://www.who.int/whosis/en/index.html, accessed 29 August 2010).
- The state of the world’s children 2008: child survival. Geneva, United Nations Children’s Fund, 2008.
- AIDS epidemic update 2007. Geneva, Joint United Nations Program on HIV/AIDS and the World Health Organization, 2007.
- The world health report 2008. Primary health care: now more than ever. Geneva, World Health Organization, 2008.
- The millennium development goals report, 2007. New York, United Nations, 2007.
- Commission on Social Determinants of Health, 2005–2008. Geneva, World Health Organization [website] http://www.who.int/social_determinants/thecommission/en/
- The world health report 2006. Working together for health. Geneva, World Health Organization, 2006.
- A snapshot of the world’s public health schools. Bulletin of the World Health Organization, 2007, 85:910–911.
- Public health schools: six portraits. Bulletin of the World Health Organization, 2007, 85:907–909.
- Health professions education directory. Cairo, World Health Organization Regional Office for the Eastern Mediterranean [website] (http://www.emro.who.int/hped/, accessed 29 August 2010).


