Research article
K.K. Al-Nasrawi,1 J.K. Al- Diwan,1 T.S. Al-Hadithi 1 and A.M. Saleh 2
فاشية من التهاب الكبد الفيروسي «ئي» في مدينة الصدر، بغداد، العراق
كاظم النصراوي، جواد كاظم الديوان، طارق سلمان الحديثي، أبو بكر مجيد صالح
الخلاصـة: يُعَدُّ الالتهاب الكبدي «ئي» E سبباً رئيسياً من أسباب التهاب الكبد في كثير من البلدان النامية. وتصف هذه الدراسة فاشيةً من فاشيات العدوى بفيروس الالتهاب الكبدي «ئي» في مدينة الصدر، بغداد، حصل الباحثون فيها على عينات من الدم من مرضى مصابين باليرقان، ممَّن تـردَّدوا على 19 مركزاً للرعاية الصحية الأولية في مدينة الصدر خلال الأشهر الستَّة التي سبقت الدراسة في عام 2005، وأجروا عليها اختبارات لكشف أسباب العدوى، فوجدوا أضداد التهاب الكبد الفيروسي «ئي» من النمط IgM لدى نسبة %38.1 من أصل 268 مريضاً. وقد كان التـرابُط بين العدوى بالتهاب الكبد الفيروسي «ئي» وبين التـراكيز غير المقبولة – إن وُجدَتْ – من ثـُمالات الكلور في عيِّنات المياه التي لا تكفل السلامة الجرثومية، تـرابُطاً يُعتَدُّ به إحصائياً. وقد سجَّل الباحثون معدّلات مرتفعة للعدوى بالتهاب الكبد الفيروسي «ئي» مع انخفاض مستويات الكلور والمياه غير المأمونة في شهر حزيران/يونيو. ويغلب أن يكون الاضطراب الكبير في إمدادات المياه والصرف الصحي أهم عامل مساهم في ذلك.
ABSTRACT Hepatitis E virus (HEV) is a major cause of acute hepatitis in many developing countries. This study describes an outbreak of HEV infection in Al-Sadr city, Baghdad. Blood samples obtained from patients with jaundice attending 19 primary health care centres in Al-Sadr city during a 6-month period in 2005 were tested for HEV. HEV (IgM) antibodies were detected in 38.1% of 268 patients. The association of HEV infection with unacceptable residual chlorine concentrations and/or bacteriologically unsafe water samples was significant. High rates of HEV infection, low chlorine concentrations and unsafe water were reported in June. Gross disruption of sanitation and water supplies was the most likely contributing factor.
Flambée d’hépatite virale E à Al-Sadr city, Bagdad, Iraq
RÉSUMÉ Le virus de l’hépatite E (VHE) est une cause majeure d’hépatite aiguë dans de nombreux pays en développement. Cette étude décrit une flambée d’infection à VHE à Al-Sadr city, Bagdad. Des échantillons de sang prélevés sur des patients souffrant de jaunisse et consultant dans 19 centres de soins de santé primaires à Al-Sadr city sur une période de 6 mois en 2005 ont été soumis à un test de dépistage du VHE. Des anticorps anti-VHE (IgM) ont été détectés chez 38,1 % des 268 patients. L’infection par le VHE était fortement associée à des concentrations de chlore résiduel inacceptables et/ou des échantillons d’eau de mauvaise qualité bactériologique. Des taux élevés d’infection à VHE, de faibles concentrations de chlore et une eau de mauvaise qualité ont été signalés en juin. Une interruption massive de l’assainissement et de l’approvisionnement en eau était la cause la plus probable.
1Department of Community Medicine, College of Medicine, University of Baghdad, Baghdad, Iraq (Correspondence to T.S. Al-Hadithi:
2Department of Community Medicine, College of Medicine, Hawler Medical University, Erbil, Iraq.
Received: 13/01/09; accepted: 08/04/09
EMHJ: 2010, 16(11): 1128-1132
Introduction
Hepatitis E virus (HEV) is endemic in the subcontinent of India, South-East Asia, China, parts of the Middle East, Africa and Mexico [1,2] and is a major cause of acute hepatitis in many developing countries [3]. HEV is transmitted principally by the faecal–oral route, and waterborne epidemics are characteristics of outbreaks of HEV infection [1,3]. HEV infection has been reported in haemodialysis patients [4] and a zoonotic route has been suggested [3].
Iraq used to have one of the best health services in the region [5]. However, during the last 3 decades the health system has suffered from a serious deterioration in the provision of health services. This decline has arisen from the massive and swift degradation of the country’s infrastructure as a result of the Iraqi–Iranian war in the 1980s, the Gulf war of 1991 and the prolonged period of economic sanctions [6]. This situation was further aggravated by the 2003 invasion of Allied forces and subsequent civil strife which led to further disruption of the infrastructure necessary for proper sanitation and safe water supply and consequently to a dramatic upsurge of infectious diseases [7–9]. HEV outbreaks are increasingly reported, in Basra (1986), Erbil (1989), Diyala (2001) and Baghdad (2001) [10,11].
These circumstances provided the impetus to carry out an epidemiological study of HEV outbreaks in Al-Sadr city, Baghdad. The objectives of the study were to describe the distribution of cases according to the primary health care (PHC) centre catchment areas where they presented and to find out the risk factors for infection including unsafe water supply and lack of effective chlorination.
Methods
A total of 268 patients with jaundice diagnosed by physicians at 19 PHC centres in Al-Sadr city were included in this study during the period 1 January to 30 June 2005. Jaundice was diagnosed clinically and confirmed by laboratory tests (high serum bilirubin and positive urine bile pigments).
A questionnaire was filled for each patient. The data requested included demographic characteristics and residency (by sector of Al-Sadr city). Blood samples were obtained from each patient and sera were tested for HEV (IgM) antibodies using an enzyme-linked immunosorbent assay (ELISA) at the public health laboratory of the Ministry of Health.
The results of bacteriological examination of drinking water were obtained from the Ministry of Environment’s Baghdad environment laboratory, according to the sector of Al-Sadr city. Water samples were cultured for detection of Escherichia coli, total coliform bacteria and total plate counts. The Baghdad environment administration’s criteria for unsafe water were: zero levels of E. coli, total coliforms < 10/100 mL and total plate counts < 50/1 mL in any water sample. The water samples are judged unsafe for drinking if any one of the tests exceeds the normal limits.
Residual free chlorine of the piped drinking water supply was measured directly at the PHC centres. Residual free chlorine concentration < 0.5 mg per L of drinking water was considered unacceptable. Visits to catchment areas of PHC centres were carried out to observe leaking or flooding in the sewage system.
The chi-squared test was used to assess the association of HEV with the independent variables (demographic characteristics, residual chlorine and unsafe water supply). A P value ≤ 0.05 was considered statistically significant.
Results
Of the 268 patients, 102 (38.1%) were positive for HEV (IgM) antibody. The highest rate of HEV infection was observed in the oldest age group ≥ 40 years (45.5%). The lowest rate (12.9%) of HEV infection was among those< 10 years of age. These variations were statistically significant (χ2 = 11.96,P = 0.017). No significant statistical difference was observed in HEV infection between males and females (39.5% and 35.6% respectively) (Table 1).
High rates of HEV infection were reported from the PHC catchment areas of El-Kemalia (75.0%), Fourteenth Tamouz (71.4%), Eighth (60.0%), Fifth (54.2%) and Eked (50.0%). The catchment areas of PHC centres with high rates of unacceptable residual chlorine concentrations and/or bacteriologically unsafe water samples mostly reported high rates of HEV infection. No HEV cases were reported from the catchment areas of the First, Seventh, El-Umaliah and El-Fdeliah PHC centres, despite high rates of unacceptable residual chlorine concentrations and/or bacteriologically unsafe water supply. These variations in HEV infection with the geographical location of PHC centres were statistically significant (χ2 = 126.7, P = 0.02). The association of HEV infection with unacceptable residual chlorine and/or bacteriologically unsafe water samples was statistically significant(χ2 = 946, P < 0.001) (Table 2).
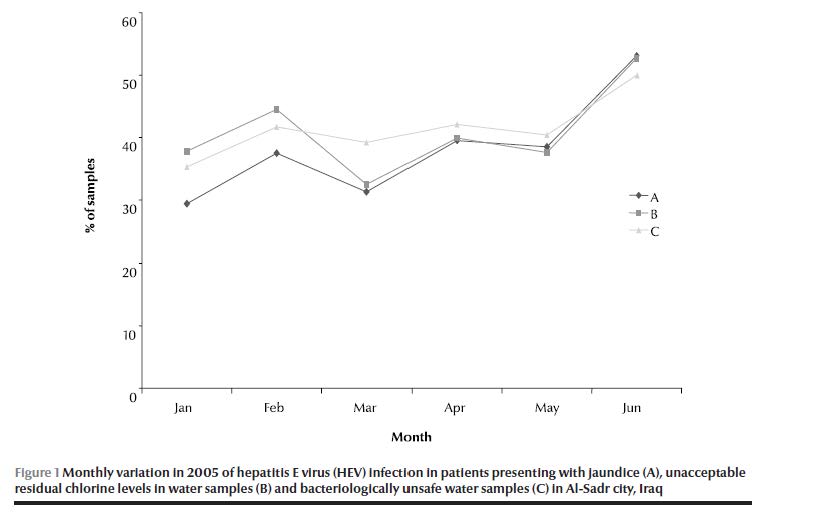
The highest rates of HEV infection, unacceptable residual chlorine and bacteriologically unsafe water samples were reported in the month of June (53.1%, 52.0% and 50.0% respectively). Lower rates were reported in the period January to May. These variations were not statistically significant (Figure 1).
Sewage system leaking or flooding was observed in the catchment areas of Third, Fourth, Fifth and Sixth, Eighth, El-Kemaliah, Eked, Hay El-Nasr, El-Gayareh and El-Fdeiliah PHC centres; between them they reported 91% of HEV infections.
Discussion
The prevalence of HEV infection revealed by this study (38.1%) is higher than that previously reported in 2001 in Al-Sadr city (24.2%) [10]. However, this rate is similar to that reported from Diyala governorate in 2002 (40.9%) [11]. Widely varying rates of HEV infection have been reported worldwide; for example from Morocco (77.3%) [12], India (47.3%–53.0%) [13,14], Somalia (83.7%) [15], Japan (13%) [16] and Egypt (6%) [17]. Variations in the prevalence of HEV infection could be related to the degree of water pollution, variation in the distribution of types of viral hepatitis in the community and the level of immunity in the community.
The significant association of HEV infection with age revealed in this study is consistent with findings reported from India [14], Hong Kong [18] and Indonesia [19]. The finding of no significant sex variation in HEV infection is similar to that previously reported in Iraq [10] and Brazil [20]. However, Corwin et al. in Indonesia reported a significantly higher HEV infection among males than females [19].
In this study, detection of E. coli and total coliforms was used as an indicator for faecal contamination of water samples, as has been used in other studies [21]. Our finding of a significant association between HEV infection and unsafe water supply (unacceptable residual chlorine concentrations and/or bacteriologically unsafe water sample) is suggestive of gross faecal contamination of piped drinking-water supplies in most of the geographical areas of Al-Sadr city, in addition to unacceptably low chlorination levels. The lack of cases reported from catchment areas with a high proportion of unsafe water samples and unacceptable chlorination could be attributed to the continuing displacement of the residents from one sector of the city to another or the improper registration of cases as a result of the civil strife and violence.
Faecal contamination could be attributed to the leaking and flooding of sewage observed at PHC centres in this study. The intermittent shortages and even interruption of drinking-water supplies forces the residents to use electric pumps for the water which further aggravate water contamination through recession of flood water into broken or leaking water pipes. According to surveys conducted in June and September 2003 by the Ministry of Health, low levels of chlorination were demonstrated in 73% of Baghdad districts where piped chlorinated water was available. In other governorates, low chlorination was found in 94% of surveyed districts [5]. The needs assessment report of the United Nations and the World Bank in 2003 indicated that the sewage collection and treatment systems were serving mainly the city of Baghdad and reaching approximately 80% of the population [22]. Contaminated water is closely associated with HEV outbreaks [1–3]. HEV has been detected in sewage and wastewater plants in other studies, in both Egypt and Norway [23,24].
Much of the drinking-water and wastewater systems in Baghdad are currently out of order or working at low capacity. Treatment plants function at a fraction of their former capacities and water distribution suffers from reduced flow and limited chlorination. Sewage collection systems are also only partially operational due to an array of problems caused by the shut-down of lift stations following the Gulf war [25,26] and the Allied invasion. There are a great number of constraints facing the reconstruction and restoration of essential services in Iraq and rehabilitation of the water distribution and sewage collection network and treatment plants remains an enormous health challenge [7–9].
This study described an outbreak of HEV infection in Al-Sadr city as an example of a man-made disaster. Gross disruption of sanitation and water supplies after extensive damage to the infrastructure seems to be the most likely contributing factor.
References
- Krawczynski K, Aggarwal R, Kamili S. Hepatitis E. Infectious Diseases Clinics of North America, 2000, 14(3):669–667.
- Zuckerman JN. Hepatitis E and the traveler. Travel Medicine and Infectious Disease, 2003, 1(2):73–76.
- Okamoto H, Takahashi M, Nishizawa T. Features of hepatitis E virus infection in Japan. Internal Medicine, 2003, 42(11):1065–1071.
- Ayoola EA et al. Hepatitis E virus infection in haemodialysis patients: a case–control study in Saudi Arabia. Journal of Medical Virology, 2002, 66(3):329–334.
- Alwan A. Health in Iraq. The current situation, our vision for the future, and areas of work, 2nd ed. Baghdad, Ministry of Health, 2004.
- Popal GR. Impact of sanctions on the population of Iraq. Eastern Mediterranean Health Journal, 2000, 6(4):791–795.
- Burnham G et al. Mortality after 2003 invasion of Iraq: a cross-sectional cluster sample survey. Lancet, 2006, 368:1421–1428.
- Fearson JD. Iraqi’s civil war. Foreign Affairs, March/April 2007.
- Iraqi Family Service Survey Study Group. Violence related mortality in Iraq from 2002 to 2006. New England Journal of Medicine, 2008, 358:484–493.
- Hasan A, Al-Dulaimy A, Jabar F. Clinical patterns and serological markers of acute viral hepatitis in Diyala. Iraqi Journal of Community Medicine, 2005, 18:355–360.
- Hasan A, Omer A, Al-Dulaimy A. Outbreak of hepatitis E infection in Baquba city. The 8th Scientific Conference of Technical Education Foundation. Baghdad, Iraq, 2002:124–127.
- Benjelloun S et al. Seroepidemiological study of an acute hepatitis E outbreak in Morocco. Research in Virology, 1997, 148:279–287.
- Aggarwal R et al. Role of travel as a risk factor for hepatitis E virus in a disease endemic area. Indian Journal of Gastroenterology, 2002, 21:14–18.
- Mathur P et al. Sero-epidemiology of hepatitis E virus (HEV) in urban and rural children of North India. Indian Paediatrics, 2001, 38:461–475.
- Mushahwar K et al. Serological studies of an enterically transmitted non-A non-B hepatitis in Somalia. Journal of Medical Virology, 1993, 40:218–221.
- Mizuo H et al. Polyphyletic strains of hepatitis E virus are responsible for sporadic cases of acute hepatitis in Japan. Journal of Clinical Microbiology, 2002, 40:3209–3218.
- Aboulata AA et al. Prevalence of hepatitis E virus in Egyptian children presented with minor hepatic disorders. Egyptian Journal of Immunology, 2005, 12:71–76.
- Wong KH et al. Epidemiology of hepatitis A and hepatitis E infection and their determinants in adult Chinese community in Hong Kong. Journal of Medical Virology, 2004, 72(4):538–544.
- Corwin A et al. Epidemic and sporadic E virus transmission in West Kalimantan (Borneo), Indonesia. American Journal of Tropical Medicine and Hygiene, 1997, 57(1):62–65.
- Bortoliero AL et al. Seroprevalence for hepatitis E virus (HEV) infection among volunteer blood donors of the regional blood bank of Londrina, State of Paraná, Brazil. Revista do Instituto de Medicina Tropical de Sao Paulo, 2006, 48:87–92.
- Gordon DM. Geographical structure and host specificity in bacteria and the implication for tracing the source of coliform contamination. Microbiology, 2001, 147:1079–1085.
- United Nations/World Bank, joint Iraq needs assessment. New York, United Nations, 2003.
- El-Esnawy NA. Examination for hepatitis E virus in wastewater plants and workers by nested RT-PCR and ELISA. Journal of the Egyptian Public Health Association, 2000, 75:219–231.
- Myrmel M et al. Enteric viruses in inlet and outlet samples from sewage treatment plants. Journal of Water Health, 2006, 4(2):197–209.
- Abdl-Wahab M et al. Water and waste water systems survey. In: International Study Team on the Gulf Crisis, eds. Health and welfare in Iraq after the Gulf crisis: an in depth assessment. New York, Center for Economic and Social Rights, 1991 (http://www.cesr.org/downloads/Health%20and%20Welfare%20in%20Iraq%20after%20the%20Gulf%20Crisis%201991.pdf, accessed 3 July 2010).
- The situation of children in Iraq. An assessment based on the United Nations Convention on the Rights of the Child. Geneva, United Nation’s Children Fund, 2002.


