M.A. Tazi,1 S. Abir-Khalil,2 F. Lahmouz,1 M.L. Arrach 1 and N. Chaouki 1
عوامل اختطار فرط ضغط الدم بين البالغين في المملكة المغربية
محمد عدنان التازي، السعدية عبير خليل، فاطمة لهموز، محمد العربي عرش، نور الدين شوقي
الخلاصـة: استمد الباحثون في هذه الدراسة المعطيات من المسح الوطني المغربي لعام 2000 للتعرُّف على عوامل الاختطار الرئيسية لفرط ضغط الدم في عينة ممثَّلة من السكان الذين يزيد عمرهم عن 20 عاماً. وقد وجد الباحثون أن اختطار فرط الضغط يزداد بمعدَّل ثابت مع تقدم العمر ليصبح على أعلى مستوى له بين القرويين (نسبة الأرجحية 1.42) والسكريين (نسبة الأرجحية 1.72). ويزداد الاختطار مع ازدياد منسب كتلة الجسم وقياس محيط الخصر وفرط كولستـرول الدم. كما ينقص اختطار فرط ضغط الدم بمقدار %36 لدى من يمشي لمدة 30 – 60 دقيقة يومياً وبمقدار %46 لدى من يمشي لمدة تزيد عن 60 دقيقة يومياً. كما ترافَق استهلاك السمك والفواكة الطازجة أكثر من مرة أسبوعياً باختطار أقل. ومن بين المصابين بفرط ضغط الدم لم يشخَّص إلا %21.9 منهم، ولم يحظ بالمعالجة الدوائية إلا %8.8 منهم.
ABSTRACT This study used data from the Moroccan national survey in 2000 to identify the principle risk factors for hypertension in a representative sample of the population age 20+ years. The risk of hypertension increased steadily with age and was higher among rural residents (OR = 1.42) and those with diabetes (OR = 1.72). The risk increased with increased body mass index, waist size and hypercholesterolaemia. The risk of hypertension decreased by 36% and 46% respectively for those who walked 30–60 min and > 60 min daily. Consumption of fish and fresh fruits 1+ times per week was associated with a lower risk. Among those with hypertension, only 21.9% were previously diagnosed and 8.8% were under medical treatment.
Facteurs de risque d’hypertension dans la population adulte marocaine
RÉSUMÉ Cette étude a exploité les données de l’enquête nationale marocaine de 2000 afin de recenser les principaux facteurs de risque d’hypertension dans un échantillon représentatif de la population âgé de 20 ans et plus. Le risque d’hypertension augmentait régulièrement avec l’âge et il était plus élevé chez les personnes vivant en milieu rural (OR = 1,42) et les diabétiques (OR = 1,72). Il augmentait également si l’indice de masse corporelle, le tour de taille et l’hypercholestérolémie étaient élevés. Le risque d’hypertension diminuait de 36 % chez les personnes qui marchaient entre 30 et 60 minutes par jour et de 46 % chez celles qui marchaient plus de 60 minutes par jour. La consommation de poisson et de fruits frais au moins une fois par semaine était associée à un risque plus faible. Parmi les sujets hypertendus, seuls 21,9 % avaient été diagnostiqués auparavant et 8,8 % étaient sous traitement médical.
1Directorate of Epidemiology and Control of Diseases, Health Ministry, Rabat, Morocco (Correspondence to M.A. Tazi:
2Moroccan League for the Control of Cardiovascular Diseases, Cardiology Department A, University Hospital Ibn Sina, Rabat, Morocco.
Received: 14/11/06; accepted: 28/03/07
EMHJ, 2009, 15(4): 827-841
Introduction
It is well established that hypertension is prevalent not only among developed nations but also in developing countries [1–3]. The available data for several countries in the Eastern Mediterranean Region indicates that hypertension and its associated complications constitute an important cause of morbidity and mortality [4,5]. It has also been reported that well-established risk factors for cardiovascular diseases such as obesity, high serum cholesterol, diabetes and smoking pose a greater risk in those with hypertension than in those with normal blood pressure (BP) levels [6].
In Morocco, the high prevalence of hypertension is a serious public health problem. The results of the 2000 national survey on cardiovascular disease risk factors showed that 33% of individuals aged 20 years and over had hypertension [3]. With knowledge of the principle risk factors of hypertension, the segments of the population most exposed, as well as the rate of its increase in Morocco, an effective strategy to combat hypertension and its associated complications can be initiated.
The objective of this study was to identify the principal risk factors for hypertension and to determine the rate of detection, treatment and control of hypertension in a representative sample of the Moroccan population.
Methods
Population and sample
The survey conducted in 2000 used a representative sample of the Moroccan population aged 20+ years. The sample selection was conducted through a multi-stage clustering technique. A total of 2000 people were selected from 100 communes, in clusters of 20 persons per commune. Morocco is divided into 68 administrative provinces and prefectures, each of which is composed of several communes. The number of clusters selected at random in a province or prefecture was proportional to the number of its inhabitants. Likewise, the number of clusters selected at random in urban and rural areas was proportional to the distribution of the Moroccan population in urban and rural areas, i.e. 53% and 47% respectively. Twenty (20) households were selected at random from each commune included in the survey, and 1 person aged 20+ years from each household was selected at random to take part in the survey. Pregnant women and bed-ridden terminally-ill people were excluded.
Data collection
Data collection took place at the participants’ place of residence. On the first day of the survey the investigator filled in the questionnaire and took the BP and anthropometric measurements of the respondent. A blood sample was taken the next day in order to determine serum glucose, total cholesterol and high-density lipoprotein (HDL) cholesterol levels. The blood sample was centrifuged within the following hour and sent to the laboratory at the Moroccan League for the Prevention of Cardiovascular Disease at the Ibn Sina Hospital in Rabat. The methodology of this survey was reported in detail in a previous article [3].
The survey questionnaire included questions on demographic data (age, sex, place of residence, level of education), socioeconomic status (monthly income, occupation), personal and family history of hypertension, diabetes and hypercholesterolaemia, as well as questions regarding smoking habits, alcohol consumption, physical exercise and dietary habits.
Socioeconomic status was classified based on type of residence and monthly income as: satisfactory (residence in a villa and/or monthly income > US$ 500), low (residence an apartment/traditional house and/or monthly income US$ 300–500) or very low (residence in a shantytown/rural house and/or monthly income < US$ 300).
Smoking and alcohol use were defined as: non-smoker (never smoked cigarettes), smoker (current smoker) or ex-smoker (quit smoking) and non-drinker (never drank alcohol), drinker (current drinker of alcohol) or ex-drinker (quit drinking).
Body mass index (BMI) was defined as: normal (< 25 kg/m2), overweight (≥ 25 to < 30 kg/m2) or obese (≥ 30 kg/m2). Waist size and hip size were measured at the beginning of the great trochanter and the beginning of the umbilicus respectively. Waist size was defined as: normal (men < 88 cm; women < 80 cm), high (men ≥ 88 to < 102 cm; women ≥ 80 to < 88 cm) or very high (men ≥ 102 cm; women ≥ 88 cm). The waist–hip ratio (WHR) as a measure of abdominal obesity was defined as: normal (men < 1; women < 0.85) or high (men ≥ 1; women ≥ 0.85).
Physical activity was defined as: vigorous (accelerated breathing), moderate (rhythmic breathing) or walking. Only physical activity that lasted > 10 minutes was considered. Each activity was measured in terms of average time spent/day (minutes).
Data about diet was based on the frequency of consumption of the main foods habitually consumed by the Moroccan population: frequently (1+ times per week), moderately (< 1 time per week) or rarely (< 1 time per month).
If one of the parents of the participant was known to have hypertension, the person was considered to have a family history of hypertension. A person was considered diabetic if his/her fasting blood sugar was ≥ 1.26 g/L and/or s/he took medication for diabetes. Hypercholesterolaemia was defined as cholesterol level ≥ 2.00 g/L and low HDL cholesterol as ≤ 0.29 g/L for men and ≤ 0.35 g/L for women.
Measurement of hypertension
Hypertension was measured using a Vaquez-type sphygmomanometer. BP measurements were taken from both arms with the subject in a sitting position after a 10 min rest, after which a 3rd BP measurement was taken from the arm with the highest BP. The systolic BP and the diastolic BP values were averaged and done on the same side. A large armband was used when the width of the arm was > 33 cm. A person was considered hypertensive with systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg and/or under treatment with antihypertensive medication. In our survey, 63 people were taking medication for hypertension.
Statistical analysis
The chi-squared test was used for the comparison of the given categories and the t-test for the comparison of the given means and standard deviation (SD) within groups. A non-conditional logistic regression model was utilized to analyse the association between the risk of hypertension (dependent variable) and the different risk factors of interest (independent variables). During the first analysis, a univariate analysis was conducted in order to select the covariates significantly associated with the risk of hypertension, with an alpha error less than 10%. During the second analysis, a multivariate logistic regression (stepwise logistic model) was utilized in order to study the association between hypertension and the significant risk factors identified in the univariate analysis. Only those variables with a P-value < 0.05 were retained in the final model.
We also examined the interactions between the different risk factors retained in the final model. The estimated odds ratios (OR) are presented along with the 95% confidence intervals (CI). The analysis was conducted using SPSS, version 10.
Results
In total, 1802 people (90.1%) participated in the questionnaire survey and blood pressure/anthropometric measures (755 men and 1047 women); 1662 of these (92.2%) gave blood samples the next day for serum glucose, total cholesterol and HDL cholesterol levels. The blood sample was insufficient to test HDL cholesterol in 21 people.
Prevalence of hypertension
The prevalence of hypertension was 39.6% and 33.6% after standardizing for the Moroccan population by age and by sex (men 30.2%; women 37.0%) [3]. The prevalence of hypertension increased significantly with age in both sexes (Figure 1) from 17.5% among those aged 20–29 years (men 17.5%; women 17.4%) up to 73.9% among those 70+ years (men 71.4%; women 77.2%).
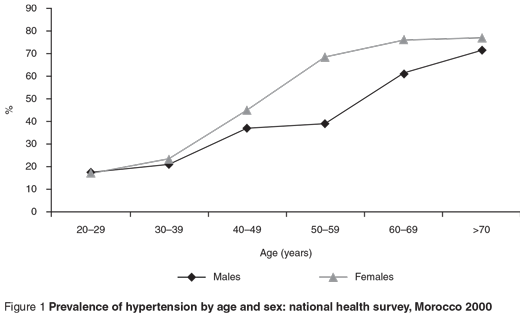
Women had significantly higher mean systolic and diastolic BP levels than men (systolic 134.0 versus 131.3 mmHg, P = 0.017; diastolic 78.7 versus 76.0 mmHg, P = 0.0002). Systolic and diastolic BP increased with age in both sexes. For men, mean BP was 123.2/72.2 mmHg in those aged 20–29 years and 148.3/81.6 mmHg in those 70+ years, reflecting an increase in systolic BP of 20% and an increase in diastolic BP of 13%. Among women, the mean values were 120.6/72.0 mmHg and 157.0/87.3 mmHg respectively in those 20–29 years and 70+ years, reflecting a 30% increase in systolic BP and 21% increase in diastolic BP.
The distribution of hypertensives and non-hypertensives in the population according to the measured variables is presented in Tables 1 and 2. Mean age was 50.6 years and 38.7 years respectively among those with and without hypertension (P < 0.001). The mean systolic and diastolic BP levels were 154.9 (SD 43.1)/90.1 (SD 27 6) mmHg and 118.5 (SD 21.2)/69.4 (SD 17.4) mmHg respectively among those with and without hypertension.
Risk factors for hypertension
The univariate analysis indicated an increased risk of hypertension among rural residents, widowers and individuals with low levels of education. The risk of hypertension was positively associated with age, BMI, waist size and WHR. Hypertension was also positively associated with diabetes, high cholesterol and lowered levels of HDL cholesterol. Those without hypertension more frequently consumed fish, lamb, chicken, eggs, beans and dried fruits. The risk of hypertension was lower among those who smoked cigarettes, drank alcohol and participated in more physical activity or walking, and was not based on socioeconomic status or family history of hypertension.
The multivariate analysis indicated that age, place of residence, BMI, waist size, diabetes, high cholesterol, walking, the consumption of fish and fresh fruits were all independent risk factors associated with hypertension (Table 3). The risk of hypertension increased with age. Hypertension was 8 times more likely among those age 65+ years compared with those 20–34 years old (P < 0.001). The risk of hypertension increased among rural residents (OR = 1.42). The risk of hypertension increased by 36% among overweight individuals and 79% among obese individuals, compared with those of a normal weight. Similarly, the risk of hypertension increased by 77% and 130% respectively when waist size was high and very high. The risk of hypertension was 1.7 times higher among diabetics and 1.4 times and 1.9 times higher respectively when cholesterol levels were 2.0–2.2 g/L or > 2.2 g/L.
Individuals who consumed fish and fresh fruits at least once per week were at low risk for hypertension (43% and 31%, respectively) than those who consumed these items less than once per month (the reference category).
Walking was also associated with a low risk of hypertension. The decrease in risk was 36% for those who walked 30–60 min/day and 46% for those who walked more than 60 min daily.
Sex, level of education, marital status, drinking alcohol, smoking and moderate or intense physical activity were not significantly associated with the risk of hypertension.
Treatment of hypertension
In our survey, 156 (21.9%) of those with hypertension had been diagnosed beforehand (men 13.5%; women 27.3%) and 63 of those (40.4%) were taking antihypertension medication (men 26.3%; women 44.9%). Only 8/63 (12.7%) cases with hypertension and under antihypertension treatment were controlled (i.e. BP < 140/90 mmHg) (men 20.0%; women 11.3%). Thus of those with hypertension, only 8.8% were under medical treatment (men 3.6%; women 12.3%) and only 1.1% were controlled (men 0.7%; women 1.4%).
Discussion
Our study has the advantage of using a representative sample of the Moroccan population and including a number of potential important risk factors of hypertension.
Similar to other studies, the risk of hypertension increased with age [7–12]. This progressive increase is linked with rising systolic BP, increasing with age to an average value close to 140 mmHg in the 7th decade [13].
The rural population was more at risk of hypertension. In the first report we suggested a possible link between stress and rural residence, the majority of such residents work in agriculture, due to the drought in Morocco over the past 2 decades [3]. Stress is known to be a risk factor of hypertension, but other studies are necessary to confirm or refute this [14].
The prevalence of hypertension in our survey was slightly higher among women [3]. However, multivariate analysis indicated that women did not have a higher risk of hypertension than men. Similarly, marital status, level of education and socioeconomic status, as defined in our study, were not significant risk factors for hypertension in the multivariate analysis. But in other studies a high risk of hypertension has been associated with low education level [10] and with a higher socioeconomic status [15].
Many studies have examined the effect of smoking on the prevalence of hypertension. In our study, smoking was not a significant risk factor for hypertension. A similar result was found in the study of Mohsen Ibrahim in Egypt [16]. Certain studies indicate that smokers and ex-smokers are more at risk [17–19]. It has also been suggested that BP among ex-smokers is higher than that of smokers as well as those who have never smoked [20]. The increased risk of hypertension among ex-smokers has been attributed to the number of cigarettes smoked daily prior to cessation of smoking and not to the duration of smoking [21]. Recently, it was suggested that smoking was associated with an increase in systolic BP among older men and not among women [22] and an increase in the incidence of hypertension [23]. Other studies have indicated an inverse relationship between smoking and BP and the risk of hypertension [7,14,20]. These contradictory results indicate that the relationship between smoking and hypertension is complicated. This is further complicated by the finding that those who smoke may consume a different diet from those who do not smoke [24]. However, it is important to note that the relationship between other factors may contribute to the risk of hypertension, such as the age at which one starts smoking and the time elapsed since smoking cessation.
The positive association between obesity and hypertension observed in our study has been reported in numerous studies [8,10–12,14,16,19,25,26]. The Framingham study indicated that 70% of new-onset hypertension may be attributed to obesity or weight gain [25]. The mechanism through which obesity and BP are related has yet to be fully elucidated. Resistance to insulin and peripheral hyperinsulinaemia due to overweight and obesity play a role in the development of hypertension [27].
Waist size reflects abdominal obesity and is considered a good indicator of obesity. The positive association observed in our study between waist size and hypertension has been reported in other studies [12,15,16,28]. Some of those studies indicated that abdominal obesity was a risk factor for hypertension independently of BMI [12,15,28]. Ledoux reported that obesity (BMI) and the abdominal distribution of fat (waist size or WHR) are equally associated with the presence of hypertension [29]. Similar to the study by Perez [14], physical activity was not associated with the risk of hypertension in our study. However, walking did seem to have a protective role against hypertension. In the study of Singh et al. in India, lower physical activity was weakly but significantly associated with hypertension [15].
The results of our study confirm those of similar studies which indicate that there is an increased risk of hypertension among diabetics [14,16,26] and those with hypercholesterolaemia [16]. The association between hypercholesterolaemia and the risk of hypertension may explain some of the mechanisms: first, hypertension and hypercholesterolaemia are linked to atherosclerosis which is associated with reduced vascular compliance [30]; secondly, high cholesterol is associated with vascular diseases, which are linked to changes in the endothelium [31,32]; thirdly, food rich in fat and cholesterol may cause a disturbance in the metabolism of prostaglandins [33]; and fourthly, hypertension and hypercholesterolemia are present in familial dyslipidaemia and hypertension [34].
In our study, drinking alcohol was not significantly associated with hypertension, similar to the results of Perez et al. [14], although other studies have found an association [7,25,35]. A Japanese study found not only a dose–effect relationship between the quantity of alcohol consumed and the level of BP but also a higher prevalence of hypertension among heavy drinkers of alcohol [35]. Another study showed that BMI and the consumption of alcohol are strong predictors of hypertension [25].
The frequent consumption of fresh fruit and fish seems to have a protective role against hypertension. Sacks et al. suggested that consumption of fresh fruits and vegetables are associated with a low risk of hypertension [36]. A number of studies indicate that fish has a protective effect against coronary artery disease [37–39] but there are few available data concerning the relationship between the consumption of fish and BP. Similar to the study conducted by Perez et al [14], the consumption of animal products high in fat were not found to be associated with an increased risk of hypertension. Concerning the relationship between the risk of hypertension and the other foods, few data are available in the international literature.
In this study, family history of hypertension was not found to be associated with hypertension. This contrasts with a number of other studies indicating a positive association suggesting a hereditary component to hypertension [14,19,26].
The detection rate for hypertension (1 in 5 patients) and the proportion under treatment for hypertension (26% for men and 45% for women) remains very low in Morocco. This situation is of further concern because only 1 in 8 patients under medical treatment had a normal level of BP. According to our study, of 100 people with hypertension only 1 had their BP controlled. The reduction in the prevalence of hypertension and its associated complications requires the reduction of the known risk factors and early and adequate assistance for hypertensive patients. It is important to educate the population, in particular those at high risk (obese, diabetic, sedentary lifestyle, etc), who must be identified and assisted.
Our study had certain limitations. The measures of BP were only taken during 1 visit, thus it was not possible to confirm with complete certainty the presence of hypertension among those with elevated BP [18]. The number of cigarettes smoked per day, the quantity of alcohol consumed and the duration of smoking and drinking alcohol were not measured. The food consumption evaluation, which measured the frequency of consumption of certain foods, was an imprecise measure and may have introduced bias, as people in the survey may not have remembered or may not have wanted to declare what they ate and because the quantity of the different foods consumed and nutrient content (carbohydrates, fats, etc.) were not taken into account.
Conclusions
The study results suggest that to reduce the prevalence of hypertension among the Moroccan population necessitates a reduction of certain risk factors, notably obesity and high serum cholesterol, but also the promotion of a healthy lifestyle with regular walking and a balanced diet rich in fresh fruits and fish.
The percentage of individuals with hypertension who are diagnosed and treated is low in Morocco and greater efforts are needed to improve the situation in order to reduce the complications associated with hypertension, most notably stroke.
References
- Gharbi M et al. Niveau des facteurs de risque cardiovasculaire dans la population urbaine et rurale du Cap-Bon: Tunisie [Cardiovascular risk factors in the urban and rural populations of the Cap-Bon : Tunisie]. Revue d’épidémiologie et de santé publique, 1996, 44:125–32.
- Berrios X et al. Distribution and prevalence of major risk factors of noncommunicable diseases in selected countries: the WHO Inter-Health Programme. Bulletin of the World Health Organization, 1997, 75:99–108.
- Tazi MA et al. Prevalence of the main cardiovascular risk factors in Morocco: results of a national survey, 2000. Journal of hypertension, 2003, 21:897–903.
- Alwan A. Prevention and management of hypertension. Alexandria, WHO Regional Office for the Eastern Mediterranean, 1996 (EMRO Technical Publication Series, No. 23).
- Alwan A. Prevention and control of cardiovascular diseases. Alexandria, WHO Regional Office for the Eastern Mediterranean, 1995 (EMRO Technical Publication Series, No. 22).
- Laurenzi M et al. On behalf of the Gubbio study group. Multiple risk factors in hypertension: results from the Gubbio study. Journal of hypertension, 1990, 8:7–12.
- Hu FB et al. Body mass index and cardiovascular risk factors in a rural Chinese. American journal of epidemiology, 2000, 151:88–97.
- Kawada T. Body mass index is a good predictor of hypertension and hyperlipidemia in a rural Japanese population. International journal of obesity, 2002, 26:725–9.
- Brown CD et al. Body mass index and the prevalence of hypertension and dyslepidemia. Obesity research, 2000, 8:605–19.
- Gus I et al. Prevalence, awareness, and control of systemic arterial hypertension in the state of Rio Grande do Sul. Arquivos brasileiros de cardiologia, 2004, 83:429–33.
- Shah SM et al. Hypertension and its determinants among adults in high mountain villages of the Northern Areas of Pakistan. Journal of human hypertension, 2001, 15:107–12.
- Jo I et al. Prevalence, awareness, treatment, control and risk factors of hypertension in Korea: the Ansan study. Journal of hypertension, 2001, 19:1523–32.
- Whelton PK. Epidemiology of hypertension. Lancet, 1994, 344:101–6.
- Perez LH et al. Relation between overweight, diabetes, stress and hypertension: A case–control study in Yarumal-Antioquia, Colombia. European journal of epidemiology, 2001, 17:275–80.
- Singh RB et al. Epidemiological study of hypertension and its determinants in an urban population of North India. Journal of human hypertension, 1997, 11:679–85.
- Ibrahim MM et al. Cardiovascular risk factors in normotensive and hypertensive Egyptians. Journal of hypertension, 2001, 19:1933–40.
- Aday LA et al. Estimating the risk and prevalence of hypertension in a suburban area of Beijing. Journal of community health, 1994, 19:331–41.
- Halimi JM et al. The risk of hypertension in men: direct and indirect effects of chronic smoking. Journal of hypertension, 2002, 20:187–93.
- Shey Wiysonge CU, Ngu Blackett K, Mbuagbaw JN. Risk factors and complications of hypertension in Yaounde, Cameroon. Cardiovascular journal of South Africa, 2004, 15:215–9.
- Seltzer CC. Effect of smoking on blood pressure. American heart journal, 1974, 87:558–64.
- Gueyffier FJ et al. Identification of risk factors in hypertensive patients. Contribution of randomized controlled trials through an individual patient database. Circulation, 1999, 100:e88–94.
- Primatesta P et al. Association between smoking and blood pressure: evidence from the health survey for England. Hypertension, 2001, 37:187–93.
- Lee DH et al. Effects of smoking cessation on changes in blood pressure and incidence of hypertension: a 4-year follow-up-study. Hypertension, 2001, 37:194–8.
- Margetts BM, Jackson AA. Interaction between people’s diet and their smoking habits. British medical journal, 1993, 307:1381–4.
- Kannel WB et al. The relation of adiposity to blood pressure and development of hypertension: the Framingham Study. Annals of internal medicine, 1967, 67:48–59.
- Tozawa M et al. Multiple risk factor clustering of hypertension in a screened cohort. Journal of hypertension, 2000, 18:1379–85.
- Plaisted CS, Istfan NW. Metabolic abnormalities of obesity. In: Blackburn GL, Kanders BS, eds. Obesity pathophysiology, psychology, and treatment. New York, Chapman and Hall, 1994:80–97.
- Thomas GN et al. Impact of sex-specific body composition on cardiovascular risk factors: the Hong Kong Cardiovascular Risk Factor Study. Metabolism, 2006, 55:563–9.
- Ledoux M et al. Correlation between cardiovascular disease risk factors and simple anthropometric measures. Canadian Heart Survey Research Group. Canadian Medical Association journal, 1997, 157(Suppl. 1):S46–53.
- Bulpitt CJ, Hodes C, Everitt MG. The relationship between blood pressure and biochemical risk factors in a general population. British journal of preventive and social medicine, 1976, 30:158–62.
- Henry PD. Hyperlipidimic arterial dysfunction. Circulation, 1990, 7:697–9.
- Vita JA et al. Coronary vasomotor response to acetylcholine relates to risk factors for coronary artery disease. Circulation, 1990, 81:491–7.
- Galli C. Dietary influence on prostaglandin synthesis. Advances in nutritional research, 1980, 3:95–126.
- Williams RR et al. Familial dyslipidemic hypertension. Evidence from 58 Utah families for a syndrome present in approximately 12% of patients with essential hypertension. Journal of the American Medical Association, 1988, 259:3579–86.
- Tsuruta M et al. Association between alcohol intake and development of hypertension in Japanese normotensive men: 12-year follow-up study. American journal of hypertension, 2000, 13:482–7.
- Sacks FM et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. New England journal of medicine, 2001, 344:3–10.
- Kromann N, Green A. Epidemiological studies in the Upernavik district, Greenland. Acta medica scandinavica, 1980, 208:401–6.
- Kromhout D, Bosschierter EB, Coulander CL. The inverse relationship between fish consumption and 20-year mortality rate from coronary heart disease. New England journal of medicine, 1985, 312:1205–9.
- Norell SE et al. Fish consumption and mortality from coronary heart disease. British medical journal, 1986, 293:426.


