A. Rikabi,1 A. Bener,2,4 A. Al-Marri3 and S. Al-Thani1
العدوى بفيروسَيْ بي وسي لالتهاب الكبد في المرض الكبدي المزمن: دراسة سكانية المرتكز في قَطَر
عمار ركابي، عبد الباري بينر، عجايب المرى، شيخة آل ثاني
الخلاصـة: درس الباحثون معدَّل انتشار العدوى بفيروسَيْ التهاب الكبد بي وسي بين مرضى الكبد في قَطَر في الفتـرة 2000 – 2005. وقد حصل الباحثون على درجات ومراحل حالات التهاب الكبد بي وسي من تقارير باثولوجية من المختبر المرجعي الرئيسي في قَطَر. ومن بين 915 مريضاً بالكبد خضعوا للدراسة، كان لدى %29.4 منهم التهاب الكبد سي ولدى %2.5 منهم التهاب الكبد بي. وقد كان معدَّل انتشار التهاب الكبد بي وسي أعلى بين غير القَطَريـين منه لدى المواطنين القَطَريـين، وهو أعلى لدى الذكور عنه في الإناث؛ ولاسيَّما التهاب الكبد سي. ولم تتـرافق معظم الحالات بمضاعفات (%89) ولا بالتهاب (%76.4)، وقد ازداد معدَّل انتشار التهاب الكبد سي بين مرضى الكبد خلال السنوات الأخيرة حتى وصل إلى 481 لكل ألف مريض بالكبد عام 2005.
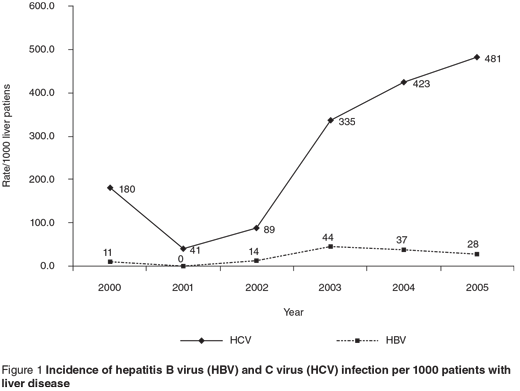
ABSTRACT We investigated the incidence of hepatitis B (HBV) and C (HCV) virus infection among patients with liver disease in Qatar from 2000 to 2005. The grading and staging of HBV and HCV cases were obtained from pathology reports at the principal reference laboratory for Qatar. Of the 915 liver patients studied, 29.4% had HCV and 2.5% had HBV. The incidence of HBV and HCV infection was greater in non-Qataris than Qatari nationals and in males than females, especially for HCV. Most cases were uncomplicated (89.0%) and had no inflammation (76.4%). The incidence of HCV has been increasing in liver patients in recent years up to a rate of 481 per 1000 patients with liver disease in 2005.
Infections par le virus de l’hépatite B et C dans la maladie hépatique chronique : étude en population au Qatar
RÉSUMÉ Nous avons étudié l’incidence de l’infection par le virus de l’hépatite B (VHB) et C (VHC) chez des sujets souffrant d’une maladie du foie au Qatar entre 2000 et 2005. Le grade et le stade des cas de VHB et de VHC ont été tirés des rapports de pathologie du principal laboratoire de référence du Qatar. Sur les 915 sujets hépatiques étudiés, 29,4 % étaient contaminés par le VHC et 2,5 % par le VHB. L’incidence de l’infection par le VHB et le VHC était plus élevée chez les non-Qataris que chez les Qataris et chez les hommes que chez les femmes, notamment en ce qui concerne le VHC. La plupart des patients ne présentaient pas de complications (89,0 %) ni d’inflammation (76,4 %). Ces dernières années, l’incidence du VHC a augmenté chez les patients hépatiques jusqu’à atteindre un taux de 481 pour 1 000 patients en 2005.
1Department of Laboratory Medicine and Pathology; 2Department of Medical Statistics and Epidemiology; 3Department of Immunology, Hamad General Hospital, Hamad Medical Corporation, Doha, Qatar (Correspondence to A. Bener:
4Evidence for Population Health Unit, School of Epidemiology and Health Sciences, University of Manchester, Manchester, United Kingdom.
Received: 27/12/06; accepted: 08/01/07
EMHJ, 2009, 15(4): 778-784
Introduction
Hepatitis is an infection of the liver caused by several viruses, the most common of which are hepatitis A, B and C. Both hepatitis B virus (HBV) and C virus (HCV) are spread mainly through contaminated blood and blood products, sexual contact and contaminated needles. Although there has been a decrease in the incidence of viral hepatitis over the last decade, it is still the most common cause of chronic liver disease worldwide [1–5].
Globally, the number of individuals infected with HBV has been estimated to be 350 million, 40% of whom may progress to cirrhosis, liver failure and hepatocellular carcinoma [3]. Approximately 170 million people worldwide are affected with HCV. It is the most common chronic infection in the United States of America (USA) and is responsible for 40% of chronic liver disease [4]. HCV infections are the principal cause of chronic liver disease, cirrhosis, carcinoma and liver transplantation. Over 17 000 people with chronic liver disease were listed for liver transplantation in 2003, with > 10% expected to die before the operation [6].
Although viral hepatitis is a global health problem, there is a considerable variability in HBV and HCV rates between and within countries and between ethnic groups [2]. The aim of this study was to assess the incidence and impact of HBV and HCV infection in patients with liver disease in Qatar.
Methods
This was a cohort hospital-based study in Qatar during the period 2000–05.
Information was gathered from the hepatitis disease registry of the Department of Preventive Medicine in the National Health Authority. Details of any patient who visits a primary health centre or private clinic in Qatar with symptoms and signs of hepatitis are notified to the Communicable Diseases Control Section and a blood specimen is sent to the central laboratory of the Hamad Medical Corporation for diagnostic tests. All reports of positive cases from the laboratory are forwarded to the Communicable Diseases Control Section database, thus ensuring that any hepatitis patient in Qatar is accurately documented.
All infectious diseases reported to the Department of Preventive Medicine are coded according to the International statistical classification of diseases and related health problems (ICD-10). Viral hepatitis is classified into acute hepatitis A (B15), acute hepatitis B (B16), other acute viral hepatitis (B17), chronic viral hepatitis (B-18) and unspecified viral hepatitis (B-19) [7]. In the Qatar central laboratory, all cases of acute and chronic viral hepatitis B are classified under B-16 and acute and chronic viral hepatitis C are classified under B-18.
From a total of 915 patients in Qatar with hepatitis documented over the study period, we studied all patients with HBV and HCV infection. Liver biopsy of the studied patients helped to establish the correct diagnosis, assess the histological activity (grading) and assess structural changes, including fibrosis and cirrhosis (staging).
Histological study of liver biopsies was performed in the histopathology laboratory at Hamad General Hospital. Differentiation between chronic HBV and HCV infection was based on the presence of classical ground-glass hepatocytes and positive staining for hepatitis B surface antigen in cases of HBV infection. Cases of chronic hepatitis C showed some or all of the histological features usually present in this infection, including lymphoid follicles in portal tracts, damaged interlobular bile ducts, steatosis and granulomas.
The histological changes of chronic hepatitis were classified according to the method of Scheuer [8]. The grading score (0–4) represents necroinflammatory activity, from absent or minimal (0) to severe and widespread interface hepatitis (4). The staging score (0–4) is based on the degree and extent of fibrosis, from no fibrosis (0) to probable or definite cirrhosis (4).
The chi-squared test for trend was used to compare the trend statistical significance differences between years. P < 0.05 was taken as the cut-off value for significance.
Results
Of the 915 patients with liver disease who were screened during the period 2000–05, 269 (29.4%) had HCV and 23 (2.5%) had HBV infection.
Figure 1 shows the incidence of HBV and HCV infection per 1000 population with liver disease over each year of the study. In every year, HCV was more common than HBV. However, there was a notable increase in the incidence of HCV in patients with liver disease during recent years, reaching 481 per 1000 patients in 2005. Incidence of HBV it was 28 per 1000 in the same year.
The rate of HCV was higher in those of non-Qatari nationality than in Qatari nationals (82.9% for all the years combined versus 17.1%) (Table 1). There was a sharp increase in the number of cases of HCV in liver patients in 2005 compared with 2000 (9-fold higher in Qataris and 6-fold higher in non-Qataris).
Over the years, the rate of HBV and HCV infection was higher in male than female patients (73.9% versus 26.1% for HBV and 80.7% versus 19.3% for HCV) (Table 2).
Table 3 shows the stage and grade of HBV and HCV in the patients by nationality. Most of the cases were uncomplicated (260, 89.0%) and had no inflammation (233, 76.4%). Of the complicated cases (32 patients), stage 2 was frequent (10 cases), especially in those of non-Qatari nationality (7 patients). Also, among patients with inflammation, grade 2 was the most frequent (38 cases), of whom 32 were non-Qataris.
Comparing the proportion of HBV and HCV among patients with liver disease in studies from different countries (Table 4), the proportion of HCV in Qatar (29.4%) and Pakistan (29.0%) were similar and very close to the proportion of India (31.5%). HBV, on the other hand, is relatively rare in Qatar (2.5%) and incidence was relatively lower than in the USA and the Far East.
Discussion
Viral hepatitis is the most common cause of chronic liver disease throughout the world [9,10]. Chronic HBV accounts for 5%–10% of cases of chronic liver disease and cirrhosis in the USA [9]. In our study, 31.9% of patients with liver disease had HCV or HBV. A study in Singapore showed that chronic HCV- and HBV-related liver disease constituted 57% of all indications for adult liver transplants [11]. A study in Romania on chronic HCV and HBV infections showed that an association with chronic liver disease was seen in half the patients [12].
In Singapore the prevalence of HBV-related liver diseases was high (Table 4), which was not surprising as HBV is endemic with a 4.1% carrier rate and complication developing in 10%–40% of patients with chronic HBV [11]. In Qatar, HBV was relatively rare, 2.5%, HCV was more common in patients with liver disease (29.4%) and the incidence increased throughout the study period. In contrast, HCV is relatively rare in Singapore and in parts of Asia [13]. In addition, studies from India have shown a prevalence of HCV of 3%–31.5% in patients with cirrhosis and chronic liver disease (Table 4) [14]. However, clinical studies from southern Europe and the USA have shown a high percentage of HCV infection in patients with cirrhosis [15], which is consistent with our findings.
There is considerable variability in the prevalence of HBV and HCV between different countries and ethnic groups. For instance, the prevalence of HCV in people with chronic liver disease has been estimated at 62%–74% in Italy [16], 74% in Egypt [17] and only 29% in Pakistan [18]. This is similar to our finding that non-Qatari liver patients had a higher rate of HBV and HCV infection than Qatari liver patients. People of non-
Qatari nationality in Qatar come mostly from hepatitis-endemic areas, which explains the higher incidence among them.
It is evident from the study findings that HCV is a major cause of chronic liver disease in Qatar. Poynard, Bedossa and Opolon reported that approximately 300 million people infected worldwide with HCV will progress to cirrhosis or liver failure, and would need a transplant in the future [19].
Conclusion
The present study findings revealed that over 30% of patients in Qatar with liver disease had viral HBV or HCV, with HCV playing the greater role,. HBV and HCV infection are both preventable. In order to limit the spread of hepatitis, efforts must be directed at minimizing exposure to sources of infection. Further studies are necessary to evaluate the sociodemographic and other associated risk factors involved with HBV and HCV infection in patients with liver disease.
Acknowledgements
The authors would like to thank Mrs S. Samson and Mr Antony George for their assistance in preparing and typing the manuscript.
References
- Schiff ER, Sorrell MF, Maddrey NC, eds. Diseases of the liver, 9th ed. Philadelphia, Lippincott Williams and Wilkins, 2003:741–4.
- Purcell RH. Hepatitis viruses: changing patterns of human disease. Proceedings of the National Academy of Sciences of the United States of America, 1994, 91:2401–6.
- Lok S. Chronic hepatitis B. New England journal of medicine, 2002, 346:1682–3.
- NIH Consensus Development Program. Management of hepatitis C: 2002. National Institutes of Health Consensus Conference Statement, June 10–12, 2002. Bethesda, Maryland, National Institutes of Health, 2002 (http://consensus.nih.gov/2002/2002HepatitisC2002116html.htm).
- Recommendations and reports. Appendix. Hepatitis A and B vaccines. Morbidity and mortality weekly report, 2003, 52(RR-1):34–6.
- Reiss G, Keeffe E.B. Hepatitis vaccination in patients with chronic liver disease. Alimentary pharmacology and therapeutics, 2004, 19(7):715–27.
- International statistical classification of diseases and related health problems, 10th revision. Geneva, World Health Organization, 1992.
- Scheuer PJ. Classification of chronic viral hepatitis: a need for reassessment. Journal of hepatology, 1991, 13:372–4.
- Types of liver diseases. Liverindia.com [website] (http://www.liverindia.com/chronic.htm, accessed 1 September 2008).
- Hepnet.com [website] (http://www.hepnet.com/hepc/aasld00/terrault.html, accessed 1 September 2008).
- James L et al. Hepatitis B seroprevalence study 1999. Singapore medical journal, 2001, 42:420–4.
- Tănăsescu C et al. The significance of chronic hepatitis B and C virus infections in some connective tissue diseases: the association with chronic liver disease. Romanian journal of internal medicine, 1999, 37(1):53–64.
- Leung NW. Management of chronic hepatitis C. Journal of gastroenterology and hepatology, 2002, 17(Suppl.):S146–54.
- Aggarwal N et al. HCV as a cause of liver cirrhosis: frequency and genotype distribution. Indian journal of gastroenterology, 2001, 20(Suppl. 2):A83.
- Fattovich G et al. Hepatitis C virus infection in chronic hepatitis B virus carriers. Journal of infectious diseases, 1991, 163:400–1.
- Simonetti RG et al. Hepatitis C virus infection as a risk factor for hepatocellular carcinoma in patients with cirrhosis. A case–control study. Annals of internal medicine, 1992, 116:97–102.
- Waked IA et al. High prevalence of hepatitis C in Egyptian patients with chronic liver disease. Gut, 1995, 37:105–7.
- Tong C et al. The occurrence of hepatitis B and C viruses in Pakistani patients with chronic liver disease and hepatocellular carcinoma. Epidemiology and infection, 1996, 117:327–32.
- Poynard T, Bedossa P, Opolon P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet, 1997, 349:825–32.


