N.M. Hanna,1 S.M. Adib2 and Z. Daoud1
1Department of Medical Laboratory Sciences, Faculty of Health Sciences, University of Balamand, Beirut, Lebanon (Correspondence to Z.D. Daoud:
2Department of Public Health, Faculty of Medicine, Saint-Joseph University, Beirut, Lebanon.
Received: 07/04/06; accepted: 13/09/06
EMHJ, 2009, 15(2): 470-474
Introduction
Symptoms of gastroenteritis compatible with a food-borne outbreak started appearing among employees at the central headquarters of a “Bank” located in Beirut, Lebanon, on the evening of Monday 17 May 2004. Earlier on that day, many employees had had lunch at the bank cafeteria. All of those with signs and symptoms had eaten the main dish of chicken noodles au gratin served at the cafeteria on that day. The chicken noodle dish had been brought from the kitchen of a local catering company in 2 large serving containers. This catering company has an excellent reputation in Beirut and had been serving the Bank for more than a year with no previous problems reported.
Public health officers alerted to the outbreak went to the caterer on May 18 in line with legal regulations. Based on the mandate of an obsolete law they were supposed to “destroy” the remains of the “poisoned” food items. This kind of policy usually renders all evidence-based epidemiological investigations impossible. Fortunately, a portion of leftovers of the chicken noodles had been hidden by the caterers from the public health food inspectors, in anticipation of potential court action. Those leftovers were sent on 18 May to the Central Laboratory, the government reference laboratory in Beirut. On 19 May, testing of the remains of the incriminated dish demonstrated the presence of S. enterica Serovar Enteritidis, thus confirming the contamination of the dish.
Case report
Preliminary epidemiological findings
A team of independent Lebanese investigators hired by the Bank conducted investigations in parallel to the public health services. They obtained the chronological order of events. The incriminated dish had been brought from the catering kitchen at 11:30 on May 17, and set up on the heating table of the cafeteria. It started to be served about 1 hour later. The cafeteria personnel reported serving about 40 dishes during the lunch break on that day. Of those eating it, only 32 people could be identified by name. Upon being interviewed, it appeared that 26 had developed signs and symptoms of gastroenteritis, and 14 had been hospitalized. In at least 1 case, the chicken noodle dish had been the only food item consumed at the cafeteria or outside throughout the day prior to the appearance of gastroenteritis symptoms. No cases appeared among those who had not taken the dish or had not eaten at the cafeteria.
For this investigation, a case of food-borne illness was defined as a person who had developed diarrhoea or fever greater than 38 °C between 17 and 19 May. The attack rate was thus very high at 81%, suggesting a very large infective dose ingested via the incriminated dish.
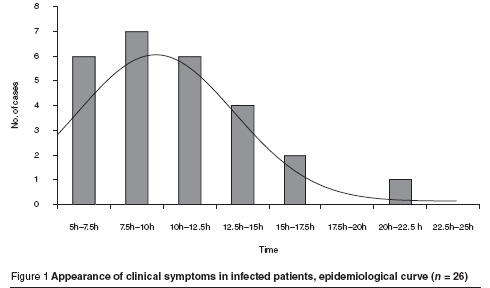
Signs started emerging as early as 5.5 hours after ingestion of the incriminated meal, and up to 22.5 hours later. The mean incubation period was 10.3 (standard deviation 4.1; median 9.1) hours for the whole group. The distribution of the incubation periods is shown in the epidemiological curve (Figure 1).
Most commonly reported signs were diarrhoea (88.5%) and fever (84.6%), with signs of systemic infection in at least 11.5% of the group (Table 1). In one case, severe septicaemia occurred. These findings are compatible with salmonella infection, which may classically begin 6–48 hours after ingestion of contaminated food or water and may last between 2 and 7 days [1]. The most credible differential diagnosis in this case would have been a staphylococcal intoxication. However, signs of intoxication with staphylococcus usually appear a few hours following ingestion, and end within 1-2 days. The clinical presentation did not point to a diagnosis of botulism or any other enteric infection [2].
Salmonellosis was confirmed in stool and blood cultures within 48–72 hours after hospital admission of the first cases. S. enterica Serovar Enteritidis was isolated from 2 patients in 2 different hospitals, and identified using the API 20E test strip (Bio-Mérieux, France). It corresponded to the strain found in the incriminated dish, further supporting the suggestion of a point source food infection in all gastroenteritis cases reported at the Bank.
Upstream findings
After confirming the epidemiological links between the infected chicken noodle dish and the gastroenteritis cases, a visit to the catering company kitchen was conducted. It showed that standard procedures of food handling had been followed. The dish had been served at the Bank in the past with no apparent health problems, suggesting that the usual preparation process in the kitchen may not be immediately incriminated. Preparation normally starts in the evening prior to the day the dish is served. However, in this instance, some of the constituents had been prepared 3 days ahead, because the dish was to be served on a Monday, immediately after the week-end closure.
In the process of preparing the chicken noodle dish, there were at least 3 potential routes of contamination:
chicken: the raw chicken obtained from a local farm could have been contaminated prior to the cooking process;
kitchen water: could have contaminated the noodles at the time of cooling, or milk put in at the time of mixing the sauce: organisms by this route may have had enough time to multiply and become a large infective inoculum;
food-handlers: carriers of infective organisms may have contaminated the ingredients during the preparation process; at various stages, almost all workers in the kitchen were involved in preparing the chicken noodles.
All 3 avenues had to be explored to determine the origin of the contamination.
All 18 kitchen workers provided samples of rectal and nasal mucosa to be cultured at the laboratory of the Saint-Georges Orthodox Hospital in Beirut. Results confirmed the absence of Salmonella carriage in all workers. At the time of the outbreak, drinking water was provided to the catering company from a tanker company, as city water is not sufficient for their needs. Despite the usual chlorination and filtration procedures, water samples repeatedly done on May 18 and 21 yielded high faecal coliform counts but no Salmonella. This evidence that some long-term contamination had been taking place in the water reservoirs involving ubiquitous, though not pathogenic, bacteria did not have direct relevance to the outbreak under investigation.
On May 28, the caterers revealed the existence of a frozen batch of the same raw chicken breast consignment that had been used for the chicken noodles. This batch yielded a significant growth of S. enterica Serovar Enteritidis, thus providing a bacterial link to the infected dish and to the gastroenteritis cases. The batch of chicken came from a large producer of poultry and eggs in Lebanon. Within a few days of finding the contaminated raw chicken, informal information was channeled to the investigators through the catering business grapevine about the existence of other cases of salmonellosis related to chicken from the same origin.
This suggested that the outbreak was multicentred, and serious enough to warrant an intervention at the farm level. The producer was advised of their potential involvement in a major food-borne outbreak. They refused to provide access for further investigation on their property.
Laboratory confirmation of the chain of events
The final proof of the alleged chain of events came after the isolates growing in the raw chicken and in the chicken noodle leftovers, as well as those isolated from 2 hospitalized patients, appeared to be genetically similar. Confirmation tests were conducted at the Institut Pasteur in Paris, as the techniques necessary for this process are not currently available in Lebanon. The confirmation was obtained using random amplified polymorphic DNA-PCR (RAPD-PCR).
In light of these findings, it was suggested that raw chicken contaminated with S. enterica Serovar Enteritidis had been shipped to the catering company. The preparation process not only did not eradicate the contamination, but provided it with substrates and delays sufficient to increase the inoculum to infective doses. The end result was a serious outbreak of salmonellosis among the Bank employees.
Discussion and practical implications
Food-borne salmonella outbreaks can create a severe public health threat [3]. Prevention is therefore an appropriate and necessary policy. In Lebanon, food-borne outbreaks, whenever detected, must be reported by law to the Epidemiological Surveillance Unit at the Ministry of Public Health in Beirut. It is believed that the major part of the case-load goes undiagnosed, and therefore undetected, and that only the very tip of the iceberg is ever reported. Despite this, food-borne diseases are still the most commonly reported infectious diseases, in a country where this category of diseases is generally receding within the context of an epidemiological transition similar to that in more advanced nations [4].
This investigation revealed important gaps in the process of food-borne outbreak control in Lebanon. Its usefulness as a case study results from the conjunction of several factors not usually found in all outbreaks. First, the management of the Bank was sufficiently incensed to decide to litigate, and was aware of the need for solid evidence to win any court action. Having observed the apparently inefficient way that public authorities were conducting the procedure, they took the initiative to call upon an independent investigative team. The caterers, concerned that they would be the only party blamed for the salmonella outbreak, had succeeded in concealing some raw and cooked items from the destructive path of the public health authorities. These items were central to establishing contamination upstream from the caterers’ kitchen.
It is generally admitted that food preparation does not by itself guarantee the eradication of bacteria. Cooking reduces the bacterial load to a minimal level not immediately dangerous to humans in normal health. However, should fully cooked or semi-cooked items be stored in less than adequate conditions, the load will increase to an infective threshold. For the catering company, it has become clear that storage of food items prepared with potentially contaminated raw ingredients at the standard 4 ºC was inadequate when the delay before consumption was several days. Freezing cabinets have now been recommended for items which have to be stored for longer than overnight.
Obsolete laws dating back to the 1930s still govern what should be done following a report of “food poisoning”. Public health officers are mandated to stop the spread by “destroying” allegedly contaminated food items and closing down incriminated facilities. The result of this activity is generally agreeable to the public but has never been proven to be epidemiologically sound.
This investigation was conducted at times almost in contravention to current laws, but in as much conformity to textbook procedures as possible [5]. It may provoke several changes in the way food-borne outbreaks are investigated, controlled and prevented in the future in Lebanon.
Acknowledgements
This study was made possible through funding provided by the Bank to the health investigation team composed of academic experts in the field. Some laboratory tests were conducted free of charge at the Institut Pasteur in Paris, France. We are particularly grateful to Ms D. Populaire who conducted the tests.
References
- Mims C et al. Gastrointestinal tract infections. In: Mims medical microbiology, 3rd ed. Philadelphia, Elsevier Mosby, 2004:282–3.
- Black JG. Oral and gastro-intestinal diseases. In: Microbiology: principles and explorations, 6th ed. New York, John Wiley & Sons, 2004:652–4.
- Centers for Disease Control. Preliminary FoodNet data on incidence of foodborne illnesses—selected sites, United States, 2001. Morbidity and mortality weekly report, 2002, 51(15):325–9.
- Ministry of Public Health. Epidemiological Surveillance Unit. Epi-news (http://cms1.omsar.gov.lb/en/HealthPrevention/EpidemiologicalSurveillanceUnit, accessed 12 April 2009).
- American Medical Association et al. Diagnosis and management of foodborne illnesses: a primer for physicians and other health care professionals. MMWR recommendations and reports, 2004, 53(RR04):1–33 (http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5304a1.htm, accessed 16 May 2008).


