A. Garjani,1 M. Salimnejad,2 M. Shamsmohamadi,2 V. Baghchevan,2 R.G. Vahidi,3 N. Maleki-Dijazi1 and H. Rezazadeh1
أثر المناقشات الجماعية التفاعلية بين الأطباء في تعزيز الوصف الرشيد للأدوية
علي رضا كرجاني، مينا سليم نزاد، شمس محمدي، ويدا باغجه وان، رضا قلي وحيدي، نسرين مالكي، حسن رضا زاده
الخلاصـة: لايزال الاستخدام الرشيد للأدوية يمثل مشكلة في جمهورية إيران الإسلامية. ويقيِّم الباحثون في هذه الدراسة أثر المناقشات الجماعية التفاعلية كأحد المداخلات التثقيفية على سلوكيَّات وصف الأدوية لدى واحد وخمسين من الأطباء العاملين في شمال غرب تبريز. وقد حلّل الباحثون الوصفات قبل وبعد المداخلة (مجموعات المداخلة ومجموعات الشواهد) مستخدمين استمارة تتضمن ثمانية مؤشرات للوصف الصحيح. وقد وجد الباحثون أن العدد الوسطي للأدوية في كل وصفة قبل المداخلة 3.82. وكانت النسبة المئوية للوصفات التي تتضمَّن المضادات الحيوية (40.8%) والكورتيكوستيروئيدات 25.9% والـحُقَن 58.0%. أما بعد المداخلة فقد حدثت تغيرات طفيفة لا يعتدّ بها إحصائياً في المؤشرات في كل من مجموعات المداخلة ومجموعات الشواهد مقارنة بما كانت عليه النتائج قبل المداخلة.
ABSTRACT: This study assessed the effect of an educational intervention (interactive group discussion) on the prescribing behaviour of 51 general physicians from the north-west of Tabriz. Prescriptions were analysed pre-intervention and post-intervention (control and intervention groups) using a proforma with 8 indicators of correct prescribing. The mean number of drugs per prescription pre-intervention was 3.82. The percentage of prescriptions with antibiotics, corticosteroids and injections were 40.8%, 25.9% and 58.0%, respectively. Following the intervention there were slight but not significant changes in the indicators in both intervention and control groups compared with pre-intervention results.
Efficacité d’une discussion interactive entre médecins aux fins de pratiques de prescription rationnelles
RÉSUMÉ: Cette étude a évalué les effets d’une intervention éducative (discussion de groupe interactive) sur les habitudes en matière de prescription de 51 médecins généralistes du nord-ouest de Tabriz. Les prescriptions (établies par un groupe ayant suivi l’intervention et par un groupe témoin) ont été analysées avant et après l’intervention à l’aide d’un formulaire comportant 8 indicateurs de prescription correcte. Le nombre moyen de médicaments par ordonnance avant l’intervention était de 3,82. Les pourcentages de prescriptions d’antibiotiques, de corticostéroïdes et d’injections étaient respectivement de 40,8 %, 25,9 % et 58,0 %. À la suite de l’intervention, les indicateurs (dans le groupe ayant suivi l’intervention comme dans le groupe témoin) avaient légèrement changé, bien que de façon non significative, par rapport aux résultats avant l’intervention.
1Department of Pharmacology and Toxicology, Faculty of Pharmacy; 2Research and Development Section, Drug and Food Vice-Chancellors Office; 3Health Service Management Research Centre, Faculty of Health and Nutrition, Tabriz University of Medical Sciences, Tabriz, Islamic Republic of Iran (Correspondence to A. Garjani:
Received: 30/04/06; accepted: 27/09/06
EMHJ, 2009, 15(2):408-415
Introduction
Many developing countries have a limited budget allocated to health care, especially for drug procurement. Inappropriate, ineffective and inefficient use of drugs commonly occurs at health facilities in both developing and developed countries [1–4]. Since 1979, the national drugs policy in the Islamic Republic of Iran has been based on using generic medications, local production of generic medicines, price control, self-sufficiency in biological products and active good manufacturing practice inspection. Essential drugs are estimated to be available and affordable for more than 90% of the population [5]. The Iranian Ministry of Health has set up a promotion centre for the rational use of drugs and dedicates considerable financial and human resources to monitoring the rational use of safe drugs [5]. Despite these successes, inappropriate use of drugs due to irrational prescription practices is a common problem in the country, and requires prompt attention [5,6]. Common types of irrational use include: non-adherence to prescribed drugs, self-medication with prescription drugs, overuse and misuse of antibiotics, overuse of injections, overuse of relatively safe drugs, use of unnecessary expensive drugs and poor patient compliance [7–10].
Successful interventions have been carried out worldwide; among these are educational programmes to update physicians about prescribing in a rational way [11–15]. Studies have shown that short, interactive, problem-oriented training courses using appropriate training materials significantly improved drug prescribing practices [16,17]. One of these studies on the impact of a short course in pharmacotherapy for undergraduate medical students in Indonesia found that prescription practices improved substantially [17]. Razon et al. have shown that a targeted educational intervention can improve antibiotic prescription practices for respiratory infections in children and decrease unnecessary antibiotic use [18]. Similar studies revealed that methods such as face-to-face training [19,20], focus group discussions [19] and small group discussions [21] were effective in improving rational prescription practices. Another study in Indonesia showed that the use of interactive group discussions had a significant effect in decreasing the use of injection formulations [22].
In view of the problem of irrational drug prescription in the Islamic Republic of Iran, it is important to find a suitable educational strategy for improving the prescribing behaviour of physicians. Commonly used approaches such as interactive group discussion, which has been proved to be effective in some other countries, have not been tested here, and therefore the present study aimed to assess the efficacy of this approach in the Iranian context. The study measured physician’s drug prescribing in the north-west of Tabriz and investigated the effect of an educational intervention in the form of an interactive group discussion.
Methods
Sample
The study group was all 51 general physician from the public and private sector in north-west Tabriz, Islamic Republic of Iran. For each physician, up to 50 of their prescriptions issued during September 2002 were selected with a simple random sampling method from the files of the Khadamat Darmany insurance organization.
Data collection
A proforma with 8 items was piloted and used to collect data on the prescribing pattern of physicians from their prescriptions. The items included clear, correct and complete writing of the drug name, dosage form, strength, directions for use and number of drugs. For each of the attributes a correct answer was assigned a score of 1 and an incorrect answer 0. For each attribute, scores were averaged (maximum score 1 per attribute). To calculate the overall prescribing pattern, the mean scores of attributes were summed. Score 8 indicated correct prescribing of all items of the prescription.
The information on the prescriptions was analysed using the prescriptions survey software of the Iranian Ministry of Health and Medical Education, and drug prescribing indicators such as the percentage of patients receiving antibiotics, glucocorticoids, injections and other drug groups were determined.
The data collectors were trained and were blind to the study conditions. Data collection was supervised and the accuracy of data was validated by a member of the study team.
One month after the intervention in August 2003, prescribing data were collected using the same proforma for both intervention and control groups.
Intervention
The data collected from prescriptions were presented to a team of health care professionals in a focus group discussion to obtain their perceptions about the training content of rational prescription writing to use at the intervention phase. Members of the focus group discussion included 5 general physicians who were not in our sample, 5 university lecturers and 5 health policy-makers.
After the intervention had been designed, the study group physicians were randomly divided into a control group (25 physicians) and an intervention group (26 physicians). At the intervention phase the test group attended a 1-day interactive group discussion on rational prescription writing.
Data analysis
All results are expressed as means and standard deviation (SD). One-way ANOVA with Student–Newman–Keuls post-test was carried out to test any differences between the mean values of different groups. The chi-squared test with Yates correction was used to compare the data presented as percentages. The differences between groups were considered significant at P < 0.05.
Results
Pre-intervention prescribing patterns
Table 1 shows the mean scores for correct prescription writing obtained by physicians before the interactive group discussion (pre-intervention), after the interactive group discussion in the control group (not attending the course) and in the test group who participated in the interactive group discussion. There were 2297 prescriptions included for analysis, collected from 51 general physicians’ files before the intervention.
Regarding correct prescribing, the physicians received a mean score of 6.00 (SD 1.10) out of 8 before the intervention. The score was lowest for correct and complete writing of drug names: mean 0.45 (SD 0.11) out of 1. Correct and complete writing of directions for use of drugs had mean scores of 0.68 (SD 0.12) and 0.66 (SD 0.11) out of 1 respectively. The mean score for clear writing of prescriptions was 0.85 (SD 0.12).
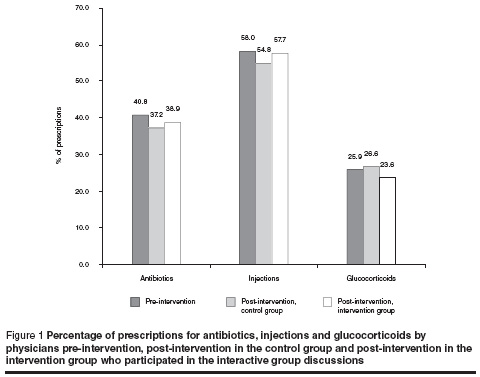
The mean number of drugs per prescription was 3.82 and the proportion with 5 or more drugs was 21.7%. In 93.7% of the prescriptions the drugs were ordered by generic name. Analysis of data from the pre-intervention period showed that 40.8% of prescriptions were for antibiotics, including penicillins, cephalosporins and aminoglycosides. Glucocorticoids, cardiovascular and nonsteroidal anti-inflammatory drugs were prescribed in 25.9%, 67.2% and 24.7% of prescriptions respectively. Injection use was widespread with 58.0% of prescriptions for injections (Figure 1).
Focus group discussion findings
All of the participants in the focus group discussion believed that fundamental reform in the structure of the health care delivery system, especially with regard to drug prescribing, was the most effective way to promote rational prescription writing. In this group discussion some underlying factors mentioned as encouraging the irrational prescription of drugs were:
poor pharmacotherapy teaching for undergraduate medical students;
lack of standard treatment guidelines;
prescribers’ worries about the precise etiology of the disease, leading to prescribing of different drugs;
low income of general physicians, who prescribe to meet patients’ demands and ensure their satisfaction in order to attract more patients;
prescribers’ belief that they ought to prescribe something to lessen the pain or prevent probable infections for patients.
lack of a good referral system;
economical incentives that persuade physicians and pharmacists to promote irrational use of drugs;
lack of effective and programmed continuing medical education and printed material for health professionals;
lack of monitoring of prescribing practices;
lack of patient education and information about drugs and their strong belief in the efficacy of injections and antibiotics.
In focus group discussions the training content to use at the interactive phase was agreed upon as follows: review of example prescriptions, principles of prescription writing, necessity of rational prescribing and use of drugs, impact of irrational use of drugs, common errors in prescribing, and rational use of injections, antibiotics and glucocorticoids (why, where, how and how long).
Post-intervention prescribing patterns
One month after the intervention, 1135 prescriptions from the intervention group and 1084 from the control group were analysed. The mean number of drugs prescribed by physicians from the intervention and control groups and from all physicians before the intervention were 3.76, 3.71, and 3.81 per prescription respectively, but the differences between groups were not significant.
Compared to the baseline data, there was a tendency toward a decreased use of antibiotics after the intervention in both intervention and control groups (Figure 1). In the control group antibiotic prescribing decreased from 40.8% (pre-intervention) to 37.2%, while in those who attended the interactive group discussion it decreased to 38.9%. The changes, however, were not statistically significant (P > 0.05). For glucocorticoids there was a slight reduction in the intervention group (23.6%) and a very slight rise in the control group (26.6%) compared to the pre-intervention period (25.9%) (Figure 1).
Injection use before the intervention accounted for 58.0% of prescriptions. Post-intervention, however, the use of injections was similar in the intervention and control groups. None of these differences were statistically significant (Figure 1).
The physicians in the interactive discussion group (intervention group) obtained a mean score of 6.24 (SD 0.80) out of 8 for correct principles of prescribing, which was slightly, but not significantly, better than the post-intervention control group [mean score 6.00 (SD 1.00)] and the pre-intervention baseline data [mean score 6.00 (SD 1.10)] (Table 1). Correct and complete writing of drug names in the intervention group attained a mean score of 0.52 (SD 0.11) out of 1, 13% better than the post-intervention control group [mean score 0.46 (SD 0.09)] and a 15% improvement on the pre-intervention score [mean score 0.45 (SD 0.11)] (P = 0.14). In spite of a slight increase obtained by the intervention group in the scores of other items, this increase was not statically significant (Table 1).
Discussion
The results of this study in Tabriz show that the problems of prescription writing still remain to be solved. Incorrect and incomplete writing of drug names and direction for use, polypharmacy (mean 3.82 drugs per patient), overuse of antibiotics (40.8% of prescriptions), misuse and overuse of injections (58.0% of prescriptions), and over-prescription of glucocorticoids (25.9% of prescriptions) are common patterns of irrational prescribing of drugs.
The results of Cheraghali et al. in 5 provinces of the Islamic Republic of Iran were very similar to ours: nationally, the mean number of drugs per prescription was 3.4 and antibiotics were prescribed in 58% of prescriptions and injections in 41% [5]. Data from other countries showed that the mean number of drugs per prescription was: Indonesia 3.5, Bangladesh 1.4, and Nigeria 3.8 [23]. The rate of antibiotic use was 43% in Indonesia, 25% in Bangladesh and 63% in Sudan [23]. The rate of injection use was 45%, 11%, and 36% in Indonesia, Zimbabwe and Sudan respectively [23]. Improving rational prescription writing is a complicated issue because many factors influence prescribing behaviour, such as guidelines, physicians’ knowledge, patient’s knowledge and habits, patients’ satisfactions, prescribers’ economic incentives, organizational setting, the supply system (including industry or pharmacy influences), regulations, and drug information systems [12,14,15].
In our study, the intervention, in the form of an interactive group discussion, was somewhat effective in shifting prescribing practices closer to the recommended norms and there was a 15% improvement in correct and complete writing of drug names. However, the intervention did not improve the rational prescribing of antibiotics, glucocorticoids or injections. It is likely that the underlying motivations mentioned before, such as economic incentives, and constraints, such as ineffective supply systems, regulations and information systems, encourage irrational prescribing. Therefore educational approaches may not be enough to improve the prescribing of drugs without solving the underlying problems. Gray has shown that didactic approaches to educating physicians and/or other health professionals do not produce changes in learner behaviour [24]. Similarly, printed materials and practice guidelines have not been shown to change prescribing behaviour [24]. Perhaps other strategies such as managerial and regulatory developments would be useful in promoting more appropriate use of drugs. In the meantime it is necessary to increase patients’ knowledge, conduct public campaigns on rational drug use, and provide face-to-face education to patients through prescribers.
Acknowledgements
This study was supported by the Research and Drug and Food Vice Chancellors of Tabriz University of Medical Sciences. The authors thank all physicians involved in the study, Eastern Azerbaijan Insurance Organizations, faculty members of Tabriz Faculty of Pharmacy, and colleagues at the Directorate General Drug and Food.
References
- Laing RO. Promoting rational drug use. Contact, 1994, October:1–6.
- Quick J, Laing R, Ross-Degnan D. Intervention research to promote clinically effective and economically efficient use of pharmaceuticals: the International Network for Rational Use of Drugs. Journal of clinical epidemiology, 1991, 44(Suppl. 2):57S–65S.
- Stuart B et al. Trends in the prescription of inappropriate drugs for the elderly between 1995 and 1999. American journal of geriatric pharmacotherapy, 2003, 1(2):61–74.
- Taylor LK et al. Inappropriate prescribing practices: the challenge and opportunity for patient safety. Health care quarterly, 2005, 8:81–5.
- Cheraghali AM et al. Evaluation of availability, accessibility and prescribing pattern of medicines in the Islamic Republic of Iran. Eastern Mediterranean health journal, 2004, 10(3):406–15.
- Gholamreza-Sepehri, Meimandi MS. The quality of prescribing in general practice in Kerman, Iran, International journal of health care quality assurance, 2005, 18(5):353–60.
- Lynch T. Medication costs as a primary cause of nonadherence in the elderly. Consultant pharmacist, 2006, 21(2):143–6.
- Ogwal-Okeng JW et al. A comparison of prescribing practices between public and private sector physicians in Uganda. East African medical journal, 2004, 81(Suppl.):S12–6.
- Laing RO. Rational drug use: an unsolved problem. Tropical doctor, 1990, 20:101–3.
- Reeler AV. Injection: a fatal attraction. Social science and medicine, 1990, 31(10):1119–25.
- Jackson SL, Peterson GM, Vial JH. A community-based educational intervention to improve antithrombotic drug use in atrial fibrillation. Annals of pharmacotherapy, 2004, 38(11):1794–9.
- Sachs L, Tomson G. Medicines and culture—a double perspective on drug utilization in a developing country. Social science and medicine, 1992, 34(3):307–15.
- Injection practices in the developing world. Results and recommendations from field studies in Uganda and Indonesia. Geneva, World Health Organization, 1996 (WHO/DAP/96.4),
- Soumerai SB. Factors influencing prescribing. Australian journal of hospital pharmacy, 1988, 18(3):9–16.
- Hogerzeil H. Promoting rational prescribing: an international perspective. British journal of clinical pharmacology, 1995, 39(1):1–6.
- Laing RO, Ruredzo R. The essential drugs program in Zimbabwe: new approaches to training. Health policy and planning, 1989, 4(3):229–34.
- De Vries TP et al. Impact of a short course in pharmacotherapy for undergraduate medical students: an international randomized controlled study. Lancet, 1995, 346:1454–7.
- Razon Y et al. Effect of educational intervention on antibiotic prescription practices for upper respiratory infections in children: a multicentre study. Journal of antimicrobial chemotherapy, 2005, 56(5):937–40.
- Ross-Degnan D et al. A strategy for promoting improved pharmaceutical use: the International Network for Rational Use of Drugs. Social science and medicine, 1992, 35(11):1329–41.
- Managing drug supply: the selection, procurement, distribution, and use of pharmaceuticals, 2nd ed. West Hartford, Connecticut, Kumarian Press, Management Sciences for Health in collaboration with the World Health Organization, 1997:138–479.
- Santoso B et al. Small group intervention vs formal seminar for improving appropriate drug use. Social science and medicine, 1996, 42(8):1163–8.
- Santoso B et al. Interactional group discussion: results of a controlled trial using a behavioral intervention to reduce the use of injections in public health facilities. Social science and medicine, 1996, 42:1185.
- Ross-Degnan D et al. Field tests for rational drug use in twelve developing countries. Lancet, 1993, 342:1408–10.
- Gray J. Changing physician prescribing behaviour. Canadian journal of clinical pharmacology, 2006, 13(1):e81–4.


