A.A. Ahangar1 and S. Hosseini2
ABSTRACT Headache is a leading cause for consultation in many patients. We compared the agree- ment between non-neurologist physicians and neurologists in diagnosis of the cause of headache among 19 854 patients attending the neurology clinic of Yahyanejad Hospital, Babol, from 1995 to 2004, who were first diagnosed by the non-neurologist physician. The diagnoses of the neurologists were based on International Headache Society criteria. The commonest causes of headache diag- nosed by the neurologist were tension-type and migraine, while sinusitis and ophthalmic disorders were the commonest diagnoses of the non-neurologist physicians. There is a need to inform physicians about the common causes of headache to ensure prompt and correct diagnosis.
Comparaison des causes de céphalées établies par des médecins neurologues et non neurologues à Babol (République islamique d’Iran)
RÉSUMÉ Pour de nombreux sujets, les céphalées sont le principal motif de consultation. Nous avons comparé le diagnostic établi par des médecins non neurologues et neurologues en ce qui concerne la cause des céphalées chez 19 854 patients consultant dans le service de neurologie de l’hôpital Yahyanejad de Babol, entre 1995 et 2004, qui avait dans un premier temps été posé par un médecin non neurologue. Le diagnostic des neurologues se fondaient sur les critères de l’International Headache Society. Les causes les plus courantes de céphalées établies par les neurologues étaient des causes associées à la tension et les migraines, alors que la sinusite et les troubles ophtalmiques étaient les diagnostics les plus courants des médecins non neurologues. Il est nécessaire d’informer les médecins des causes fréquentes de céphalées pour permettre un diagnostic rapide et correct.
1Department of Neurology, Yahyanejad Hospital; 2Department of Social Medicine, Babol University of Medical Sciences, Babol, Islamic Republic of Iran (Correspondence to A.A. Ahangar: alijanahmadiahangar@ yahoo.com).
Received: 15/03/06; accepted: 25/06/06
EMHJ, 2008, 14(5): 1198-1204
Introduction
Headache is one of the most common com- plaints of human kind. In several epide- miological studies 94%–96% of the general population are reported to have episodes of headache throughout their life [1]. Head- aches are important because they are so prevalent and they interfere with the ability of large numbers of individuals to carry out daily activities, and this can have a negative impact on society in terms of productivity [2–4]. In western societies, migraine and tension-type headaches are more prevalent than in eastern societies [5]. Migraines af- fect 28 million people in the United States (US), and most of these individuals experi- ence attack-related morbidity [6]. Rates in China, on the other hand, are especially low, which may be due to cultural differences, as pain tolerance, especially for headache, is affected by cultural, racial and psychologi- cal factors [7–13].
Proper use of the International Headache Society (IHS) classification and diagnostic criteria is important for accurate diagno- sis and treatment of migraine [14,15], as well as for standardization of patients for research protocols [16]. The misdiagnosis of migraine as tension-type headache has potentially significant consequences be- cause it may prevent patients with disabling headaches from receiving appropriate treat- ment [17]. Although people with migraine are aware of their headaches, they are often not aware that they have migraine. This can lead to inappropriate or ineffective use of treatments, delays in seeking appropriate care and miscommunication with physi- cians [18].
Many patients admitted to neurol- ogy clinics, including ours, have previously consulted different physicians and received various investigations to diagnose their headache [19–24] but despite pharmacolog- ical and non-pharmacological treatments, their headache has remained. Because of the importance of prompt and correct diagnosis of headache and because we do not have any data about the accuracy of the first diagnosis of headache cause in our region of northern Islamic Republic of Iran, we compared the diagnosis first made by non-neurologist physicians with that of neurologists to see the degree of correlation.
Methods
This was a descriptive, cross-sectional study using census sampling of 48 750 patients attending our neurology clinic in Babol, northern Islamic Republic of Iran, from 1995 to 2004. Of these, 25 810 had headache as their chief complaint. Inclusion criteria were: patients with headache who had previously consulted a non-neurologist physician and had had no cure for their headache. Exclusion criteria were: i) pa- tients with primary brain lesions including brain tumours and vascular diseases of the brain or epilepsy; ii) patients with known systemic disorders such as malignancies, chronic infections, diabetes, heart failure, renal failure in which headache was a part of their clinical manifestation; iii) patients with a definite diagnosis of their headache cause who had been referred for treatment, introduced for consultation from other col- leagues, or were having their first visit. Af- ter exclusion, 22 670 patients remained.
A file including sex, age, educational and socioeconomic status and previous di- agnosis was opened for each case. Patients also underwent medical history taking and general and neurological examination by a neurologist and, if needed, additional procedures such as neuroimaging (CT scan or MRI), electrophysiological tests (EEG) or laboratory analyses, or consultation with other specialists. Cause of the headache was recorded according to the international clas- sification of headache disorders [14]. After diagnosis, each patient received proper pharmacological and/or non-pharmacologi- cal treatment and a recommendation for a second consultation after 1 month. Of the 22 670 patients, 21 540 returned again after 1 month. They underwent another thorough general and neurological examination and further evaluation if needed. The patients with no relief (due to inappropriate drug administration, drug complications, fear of drug dependency, lack of attention to non-pharmacological instructions, incorrect diagnosis of the neurologist or unidentified cause) were excluded. In the final stage 19 854 patients whose diagnosis was con- firmed at the second evaluation remained in the study. Their first diagnosis (by a non- neurologist physician) was compared with the diagnosis of the neurologist.
Results
In this study, among the 48 750 patients who visited our neurology clinic in the 10 years of the study (1995–2004), headache was the main complaint in 25 810 (53%) cases. After initial exclusions and by the second stage of consultation 19 854 patients remained in the study. Most were aged 30 to 39 years and there were more women (12 145) than men (7709).
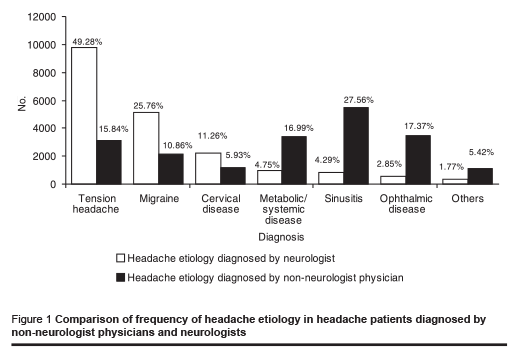
The commonest causes of headache in the patients diagnosed by the neurolo- gists were tension headache (49.28%) and migraine (25.76%), whereas sinusitis (27.56%) and ophthalmic disease (17.37%) were the commonest causes of headache in these patients diagnosed by non-neurologist physicians. Only 15.84% and 10.86% of the patients respectively were diagnosed with tension headache and migraine by non-neurologist physicians. Comparison of the frequency of the different causes of headache as diagnosed by non-neurologist physicians and neurologists is shown in Figure 1.
Discussion
Most of the neurological consultations in this study were because of headache. Head- aches are among the commonest causes of primary care consultation [25]. In this study most patients were aged 30 to 40 years, which is similar to other reports [1]. Headache is commoner in women [26] and 61.2% of our patients were women. Epide- miological studies report primary headache, such as tension-type and migraine [5], is the commonest cause of headaches but in our study, non-neurologist physicians generally diagnosed sinusitis and ophthalmic disor- ders as the cause of headache in patients. These patients even received investigations and treatment such as antibiotics, sinus washing and in some cases sinus surgery or ophthalmic glasses. In one study, 88% of patients with a history of “sinus” headache were determined to have migraine-type headache [27]. In patients with recurrent headaches without fever or purulent dis- charge, the presence of sinus-area symp- toms may be part of the migraine process [27]. In a clinical study, nearly 90% of par- ticipants with self-diagnosed or physician- diagnosed sinus headache met the criteria for IHS migraine-type headache [28]. Thus migraine should be included in the differen- tial diagnosis of such patients.
In our study there was a considerable amount of misdiagnosis when patients first presented with headache. Incorrect first diagnosis has been reported in other re- search; for example in one study 37% of the patients under treatment for tension-type headache, were found to have migraine on further investigations by the neurologist [9]. In another report, 96% of the patients who thought their headaches were due to sinusi- tis actually fulfilled the complete diagnostic criteria for migraine [29]. Sinus headache is a widely accepted clinical diagnosis, al- though many medical specialists consider it an uncommon cause of recurrent headaches. In another study among 3074 individuals who completely fulfilled the migraine cri- teria, only 53% were being treated for this condition [18]. In another report, 52% of patients suffering from headaches that met the migraine criteria, had been treated for a different condition by the first physician they consulted [30] and in another study of migraine patients, 69% of the general practitioners had made a wrong diagnosis [31]. That migraine is significantly under- diagnosed in the US and other countries is well established [32] and migraine is an important target for public health interven- tions because it is highly prevalent and disabling [33].
Generally, the initial diagnosis made by physicians first consulted by the pa- tients – sinusitis, ophthalmic disorders, infectious, systemic or metabolic diseases, hypertension, cervical diseases, migraine, tension headache and headache due to space occupied lesions of the brain – did not cor- respond with the statistics reported in the literature and also they showed no cure with the treatments based on these diagnoses. On the other hand, the diagnoses made by the neurologist, which was confirmed on follow-up, mostly agreed with the statis- tics reported. Thus tension-type headache (49.28%) was the most frequent diagnosis followed by migraine (25.76%) and cervical disease (11.26%). Sinusitis and ophthalmic disorders were only responsible for 4.29% and 2.85% of headaches respectively ac- cording to neurologists.
The socioeconomic impact of migraine and tension-type headache is very important because large numbers of people suffer from them, which results in a loss of pro- ductivity as many sufferers are forced to be absent from the workplace or work with decreased efficiency. The quality of their life is also very adversely affected [34,35]. For example, during 1997 in the United Kingdom the overall loss of productivity due to migraine was estimated at between £611 million and £741 million and US$ 13 billion in the US [36].
The differential diagnosis of headache is often challenging, with significant clinical and socioeconomic consequences of incom- plete or inaccurate diagnosis; overlapping symptoms contribute to the diagnostic chal- lenge. By becoming aware of these diag- nostic pitfalls and being more judicious and careful in diagnosing migraine and other headache types, health-care providers can improve the diagnosis of migraine and help patients to receive appropriate therapy.
The findings of this study show a large disagreement between the initial diagnosis at the first consultation and the correct diagnoses for the patients with headache. They highlight the importance of educating our physicians with regard to the up-to-date statistics reported for headache cause and the international criteria for diagnosis of headache causes. They need to be encour- aged to change their views in evaluation of such patients as well as their diagnosis, prophylaxis and treatment so that patients can be diagnosed promptly and correctly and given the appropriate treatment.
Acknowledgements
The authors thank Miss Soleymanian and Miss Aghajani (Department of Clinical Educational of Yahyanejhad Hospital) for their help in manuscript typing and figure drawing.
References
- Schwartz BS et al. Epidemiology of tension-type headache. Journal of the American Medical Association, 1998, 279:381–3.
- Colás R et al. Chronic daily headache with analgesic overuse: Epidemiology and impact on quality of life. Neurology, 2004, 62:1338–42.
- Stewart WF et al. Lost productive time and cost due to common pain conditions in the US workforce. Journal of the American Medical Association, 2003, 290:2443–54.
- Gesztelyi G, Bereczki D. Primary head- aches in an outpatient neurology head- ache clinic in East Hungary. European journal of neurology, 2004, 11(6):389– 95.
- Lyngberg AC et al. Incidence of primary headache: a Danish epidemiologic follow- up study. American journal of epidemiol- ogy, 2005, 161:1066–73.
- Burk CT et al. The impact of an over- the-counter migraine medication pro- gram on quality of life. Headache, 2003, 43(3):191–201.
- Litcher-Kelly L et al. Associations among pain intensity, sensory characteristics, affective qualities, and activity limitations in patients with chronic pain: a momen- tary, within-person perspective. Journal of pain, 2004, 5:433–9.
- Gupta VK et al. Chronic daily headache with analgesic overuse: Epidemiology and impact on quality of life. Neurology, 2004, 63(7):1341.
- Zwart JA et al. Analgesic overuse among subjects with headache, neck, and low- back pain. Neurology, 2004, 62:1540–4.
- Niere K, Jerak A. Measurement of head- ache frequency, intensity and duration: comparison of patient report by question- naire and headache diary. Physiotherapy research international, 2004, 9(4):149– 56.
- Kaniecki RG. Migraine and tension-type headache. An assessment of challenges in diagnosis. Neurology, 2002, 58(Suppl. 6):S15–20.
- Rasmussen BK. Migraine and tension- type headache are separate disorders. Cephalalgia, 1996, 16:217–20.
- Leston JA. Migraine and tension-type headache are not separate disorders. Cephalalgia, 1996, 16:220–2.
- Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia, 1988, 8(Suppl. 7):1–96.
- Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia, 2004, 24(Suppl. 1):9–160.
- Marks DR, Rapoport AM. Diagnosis of migraine. Seminars in neurology, 1997, 17(4):303–6.
- Kaniecki RG. Migraine and tension-type headache: an assessment of challeng- es in diagnosis. Neurology, 2002, 58(9 Suppl. 6):S15–20.
- Lipton RB, Stewart WF, Liberman JN. Self-awareness of migraine: interpreting the labels that headache sufferers apply to their headaches. Neurology, 2002, 58(9 Suppl. 6):S21–6.
- Pietrini U, De Luca M, De Santis G. Hyper- tension in headache patients? A clinical study hypertension in headache patients? A clinical study. Acta neurologica Scandi- navica, 2005, 112(4):259–64.
- Scher AI, Stewart WF, Lipton BL. Caffeine as a risk factor for chronic daily headache: A population-based study, Neurology, 2004, 63(11):2022–7.
- Gesztelyi G. [Primary headache and depression]. Orvosi hetilap, 2004, 145(48):2419–24 [in Hungarian].
- Stang PE, Carson AP, Rose KM. Head- ache, cerebrovascular symptoms, and stroke: The Atherosclerosis Risk in Communities Study. Neurology, 2005, 64(9):1573–7.
- Diener HC, Kurth T. Is migraine a risk factor for stroke? Neurology, 2005, 64(9):1496–7.
- Pfund Z et al. Headache in intracranial tumors. Cephalalgia, 1999, 19:791–6.
- Jensen R, Olesen J. Tension-type head- ache: an update on mechanisms and treatment. Current opinion in neurology, 2000, 13(3):285–9.
- Jimenez-Caballero PE. Análisis de las cefaleas atendidas en las guardias de Neurología [Analysis of the headaches treated in emergency neurology depart- ments]. Revista de neurologia, 2005, 40(11):648–51.
- Schreiber CP et al. Prevalence of mi- graine in patients with a history of self- reported or physician-diagnosed “sinus” headache. Archives of internal medicine, 2004, 164(16):1769–72.
- Cady RK, Schreiber CP. Sinus headache: a clinical conundrum. Otolaryngology clin- ics of North America, 2004, 37(2):267– 88.
- Cady RK, Schreiber CP. Sinus headache or migraine? Considerations in making a differential diagnosis. Neurology, 2002, 58(9 Suppl. 6):S10–14.
- Evans RW, Wheeler SD. Pseudosinus headaches: misdiagnosis of migraine by migraineurs and physicians. Headache, 2003, 43(9):1010–12.
- Sedighi B, Ghaderi-Sohi S, Emami S. Evaluation of self-medication prevalence, diagnosis and prescription in migraine in Kerman, Iran. Saudi medical journal, 2006, 27(3):377–80.
- Diamond ML. The role of concomitant headache types and non-headache co- morbidities in the underdiagnosis of mi- graine. Neurology, 2002, 58(9 Suppl. 6): S3–9.
- Lipton RB et al. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Head- ache, 2001, 41(7):646–57.
- Schwartz BS, Stewart WF, Lipton RB. Lost workdays and decreased work effective- ness associated with headache in the workplace. Journal of occupational and environmental medicine, 1997, 39:320–7.
- Rasmussen BK. Epidemiology of head- ache. Cephalalgia, 2001, 21(7):774–7.
- Kernick D. An introduction to the basic principles of health economics for those involved in the development and delivery of headache care. Cephalalgia, 2005, 25(9):709–14.


