M.R. Masjedi,1 R.T. Asl1 and L. Fadaizadeh1
ABSTRACT To study the participation of the private sector in detection and diagnosis of tuberculosis, all suspected cases referring to 4 private laboratories in Tehran for acid-fast bacillus examination during 2002–03 were documented. Of 9037 cases enrolled in the study, 637 had positive examination results (7.1%). Of these 531 (5.9%) cases were direct smear-positive and 489 (5.4%) were culture-positive. Data from the Iranian Ministry of Health showed 9479 cases referred to government laboratories in Tehran urban area during the study period, 208 (2.2%) of which were positive. This larger than expected proportion of TB patients who are detected and managed by the private sector indicates that much closer cooperation is needed between the public and private sectors.
Rôle des laboratoires privés dans le dépistage de la tuberculose à Téhéran (République islamique d’Iran)
RÉSUMÉ Afin d’étudier la participation du secteur privé au dépistage et au diagnostic de la tuberculose, nous avons recueilli des données sur tous les cas suspects adressés à quatre laboratoires privés de Téhéran en vue d’une recherche de bacilles acido-résistants en 2002-2003. Sur les 9037 cas inclus dans l’étude, 637 avaient des résultats d’examen positifs (7,1 %). Sur ces cas, 531 (5,9 %) étaient positifs à l’examen direct et 489 (5,4 %) positifs à la culture. Selon les données du ministère iranien de la Santé, 9479 cas ont été adressés à des laboratoires publics de l’agglomération de Téhéran pendant la période de l’étude, et 208 (2,2 %) d’entre eux étaient positifs. Cette proportion plus importante que prévue de patients tuberculeux dépistés et pris en charge par le secteur privé indique qu’une coopération beaucoup plus étroite doit s’instaurer entre les secteurs public et privé.
1National Research Institute of Tuberculosis and Lung Disease, Tehran, Islamic Republic of Iran (Correspondence to L. Fadaizadeh:
Received: 19/02/06; accepted: 08/06/06
EMHJ, 2008, 14(5): 1110-1118
Introduction
Tuberculosis (TB) is considered to be the greatest cause of mortality and morbidity due to any single infectious disease worldwide. According to the World Health Organization (WHO) [1], there were an estimated 19 740 positive TB cases in the Islamic Republic of Iran out of a population of 68 070 000, with a total of 5335 new smear-positive cases notified during the year 2002. In many high-prevalence countries a large proportion of case detection and treatment is performed by the private sector [2]. This sector includes physicians, pharmacists, nurses and especially laboratories, which have an essential role in the cycle of detection and treatment [3]. Usually cases detected by the private sector are treated in the same cycle and therefore may not be registered or handled by the national tuberculosis programme (NTP).
It is often stated that the differences between estimated and registered cases fall into 2 categories; first, cases that have not been diagnosed and, second, cases that have been diagnosed but have not been reported. The NTP has no scheduled and effective programme for observing the activities of the private sector regarding TB detection and treatment. We decided to study the private laboratories as a proxy for evaluating the participation of the private sector in NTP. The present study, which is believed to be the first to undertake TB detection in the private sector, was conducted in Tehran during the years 2002–03, to determine the extent of case notification performed by the private sector.
Methods
This cross-sectional study was performed during the years 2002–03 in the 4 main laboratories that specialize in detection of acid-fast bacilli in the urban area of Tehran municipality. These 4 laboratories have the most experienced technicians in the field of Mycobacterium spp. detection. Most general private laboratories in the area refer their specimens to these 4 laboratories because, although all private laboratories are potentially able to perform acid-fast bacillus examination, due to safety problems they prefer to use the specialized laboratories. This was confirmed by the registration offices of the laboratories which showed that in addition to specimens directly received by the laboratories, specimens referred from other private laboratories were also registered and the results reported back to the referring laboratories.
All suspected cases referred to these laboratories for acid-fast bacilli detection during the study period were enrolled into the study. The inclusion criteria of our cases were all specimens referred for direct Ziehl–Nielsen staining and culture in Löwenstein–Jensen medium, including sputum, bronchoalveolar lavage, gastric lavage and tissue samples.
Each laboratory was initially evaluated using previously established quality control criteria or by observing their methods of examination along with other laboratory evaluation guidelines. These guidelines were established by the reference laboratory of the Islamic Republic of Iran for TB laboratory quality control, and were in accordance with those proposed by the International Union against TB and Lung Disease and the World Health Organization. After evaluating the laboratories and confirming their quality, each laboratory was visited on a regular weekly basis.
The participating laboratory staff were instructed about the information required for the study, the method of data collection and the inclusion criteria of our study. They were given the questionnaire and were trained to gather information from the patients or the referring laboratories. From the records of patients at each laboratory information was collected about: age, sex, nationality, reason for referral, present illness, type of specimen, name of physician, address and phone number of both patient and physician, direct smear examination results and culture results. Each laboratory was contacted weekly to register the data obtained.
Data entry and analysis were performed by SPSS, version 11.0, and STATA, version 4.0. Initially crude frequencies and percentages of each variable were extracted and calculated. To detect the individual effect of each factor, chi-squared test (or Fisher exact test if needed) was used.
Results
A total of 9037 cases suspected of active TB and referred to the 4 main private laboratories in Tehran were enrolled into the study, 4036 (44.9%) in females and 4959 (55.1%) in males (sex unknown for 42) (Table 1), with ages ranging from 1 to 99 years (Table 2). The distribution of suspected cases by age is shown in Table 2. The proportion of suspected cases increased in older age groups and the highest percent-age of cases (27.3%) was the age group ≥ 65 years. Analysis of variance by age groups and reference laboratories showed no association between age of suspected cases and laboratory (P = 0.959) (Table 3).
Regarding nationality, 8885 (98.6%) suspected cases were Iranian and 123 (1.4%) were Afghan (missing data for 29 cases).
The frequencies of the types of specimens referred were: 6671 sputum (73.8%), 888 bronchoalveolar lavage (9.8%), 395 urine (4.4%), 301 pleural fluid (3.3%) and 222 gastric washing (2.5%) (other specimens: 560).
The examination results revealed that out of 8995 cases where data were available, a total of 635 (7.1%) were positive by direct smear and/or culture. There were 311 cases (49%) in females and 324 (51%) in males. Of these, 598 (97.4%) cases were Iranian and 16 (2.6%) Afghan (missing data: 21).
Age groups 15–24 years, 55–64 years and ≥ 65 years had the highest number of positive results compared with other groups and the ≥ 65 years group was the most dominant (Table 4). While the positivity ratio of the total results (smear and/or culture) was 7.1% for all examinations, the positivity ratio of specimens from females was significantly higher than for males (7.7% versus 6.5%) (P < 0.03). Regarding the nationality of cases, the total positivity ratio of specimens was significantly higher from Afghans compared to Iranians (13.0% versus 6.7%) (P = 0.006).
Of the total number of suspected cases, 531 (5.9%) were positive by direct smear, 260 (49%) in females and 269 (51%) in males (missing data: 2), with a statistically significant difference between the sexes (χ2 = 4.16, f = 1, P < 0.041). It should be noted that 1 laboratory did not consent to giving culture results but the remaining 3 had a total culture-positive rate of 489 cases (5.4%).
The frequency of direct smear positivity by sex is shown in Table 5 and positivity by laboratory is demonstrated in Table 6. Table 6 actually shows the rate of case referral to each laboratory and indicates that the Pasteur laboratory was the most active in case detection among the private laboratories.
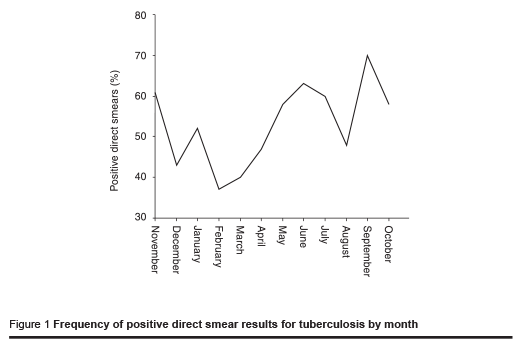
When examining the seasonal pattern of smear-positive patients referred throughout the 1-year period, it was revealed that September and June were the 2 months with the most case referrals (Figure 1).
According to data from the Iranian Ministry of Health (MOH), the total number of cases referred to government laboratories in the Tehran urban area during the period of the study was 9479, including 7850 (82.8%) Iranians and 1629 (17.2%) Afghans. Of these 208 (2.2%) were reported positive, including 78.8% Iranians and 21.2% Afghans (Table 7).
Discussion
Our study showed that the 4 private laboratories that are active in performing acidfast bacillus examinations in Tehran play a valuable role in TB diagnosis in the area. According to the gathered data, 9037 specimens were referred to the private sector. By comparing this result with the number of new smear-positive cases reported to the MOH, 9479 cases for year 2002, it is concluded that the private sector is more active than expected in TB diagnosis.
Considering the sex of the total suspected cases referred, significantly fewer were from females (44.9%) than males (55.1%), suggesting that males are more likely to refer to private laboratories and females to the public sector. Furthermore, 49.0% of the smear-positive cases were in females and 51.0% in males, which differs from the 2004 WHO report of 48.1% males and 51.9% females. This confirms the greater tendency for male patients to refer to the private sector. On the other hand, the positivity ratio of the female cases was higher (7.7% versus 6.5%) which means that although females may refer less often to private clinics, when they do, they are significantly more likely to be as true cases.
There also seemed to be an age bias towards use of the private sector by TB cases. Our results showed that the patients aged ≥ 65 years and 15–24 years old had the highest rate of visits to the private laboratories. This is in accordance with annual data presented by WHO [1], which showed that elderly patients had the highest number of visits. The fact that the geriatric group referred more to the private sector may be due to the fact that the number of older people in the Islamic Republic of Iran has risen dramatically during the past decades and some of them may have had TB during their youth and were experiencing a flare-up of a past problem. Therefore, since they may be a source of infection for family members and the community, special attention must be paid to this vulnerable group and programmes should be arranged for their health care and disease detection.
Considering the examination results, data showed that the overall positivity ratio of direct-smear and/or culture examination was 7.1% in the private laboratories. Also the positivity ratio for the direct-smear examination of sputum was at least 4.9% compared with 2.2% reported by the government laboratories, which shows that a considerable number of patients referring to private laboratories were true cases. This is comparable to data from Nepal that reported a 7.7% positivity ratio of directsmear examination in private laboratories [3]. But according to the same report, the private laboratories did not conform to the quality control standards of TB laboratories proposed by the Nepalese MOH. According to our reference laboratories, the quality of the 4 private laboratories was in accordance with the standards proposed by the Iranian MOH and the results are therefore highly reliable. But considering their higher positivity ratio it seems that a greater number of truly infected patients are referring to the private sector. The reason for this may be the fact that despite the large number of public laboratories, their wide distribution and low costs, the MOH sector has not been successful in detecting patients and therefore there have been more referrals of true patients to the private sector. There are 2 explanations for this finding; first, the public sector is not performing well and, second, patients do not confine themselves to the public sector, a reason which may be also related to the first.
According to data given by the Iranian MOH a total of 82.8% of the suspected cases attending government facilities were in Iranians and 17.2% in Afghans, with 78.8% of the smear-positive cases Iranian and 21.2% Afghan. This showed that there is a significantly higher tendency for Afghans to refer to the MOH compared with Iranians and also a considerably higher positivity ratio for Afghans. The reason for this may be that Afghan families are mostly refugees of low economic status and they prefer to refer to the lowest cost health care centres, i.e. the public centres.
Considering the seasonal pattern of case detection, September and June were the 2 months with the most case referrals, which is in accordance with the pattern reported by the MOH. It is important to study the pattern for several consecutive years to confirm if a pattern exists throughout the year, and pay special attention to case detection during the high seasons for new cases. Also after taking into account of the latency period of TB, a retrospective study can reveal much about the reason for the new infection and ways to control the disease in the future.
This study, which was the first to be performed on the role of the private sector in detection of TB in Islamic Republic of Iran, elucidates one of the major pitfalls of the NTP programme of our country—the involvement of the private sector. Regarding the follow-up of patients it should be noted that since the aim of this study was to assess only the role of private laboratories in TB detection, patients need to be followed in further studies. Similar surveys conducted in other countries, especially India, have also emphasized the important role of the private sector in case detection and treatment [4–17].
As stated earlier, the annual number of cases detected by the private sector was quite similar to that of the MOH, which indicates the importance of the private sector in TB diagnosis. The question remains, however: are these cases registered, followed up and treated effectively? As shown in other settings, the private sector still does not conform to the standards of TB management [10]. Therefore, as Mills et al. [11] and Lönnroth et al. [13] have proposed, the quality of the care given by this sector and the treatment outcome must be evaluated, and effective steps must be taken to resolve the discrepancies regarding TB management.
The aim of this study was to demonstrate the extent of work done by the private laboratory sector in Tehran and to elucidate the target group of TB patients referring to this sector. We emphasize the importance of this active, but neglected, sector and the need for closer relations between the public and private sectors. This relation should be based on both knowledge exchange and executive action. A public–private mix strategy may be a plausible way forward.
Conclusion
The results of this study reveal the important role of the private sector in detecting TB in Tehran and the large burden of TB management carried out by this sector, which has been greatly neglected to date. It is concluded that in order to overcome the existing problems of diagnosis, follow-up and management of TB patients, more attention must be paid to the private laboratories and a closer cooperation must exist between the government and private sectors involved in TB control.
Acknowledgements
This work was funded by the joint EMRO/ TDR/CTD small grants scheme for operational research in tropical and communicable diseases (grant number: SGS02/85). We thank them for funding this project and also for their rewarding comments during implementation of the project.
We also gratefully acknowledge the cooperation of the heads of the private laboratories—Dr Zia Zarifee, Dr Danesh, Dr Ghazisaeed and Dr Bahremand—and their staff for data collection and coordination of the project. We thank Mr Sabetzadeh, Dr Ashayeree and Dr Mohammad Sadeghi who meticulously performed this task.
We also thank the staff of the TB department at the MOH and especially Dr M Nasehi, head of department, for the valuable information she gave regarding the MOH laboratories.
References
- WHO report 2003: global tuberculosis control surveillance, planning, financing. Geneva, World Health Organization, 2004:158 (WHO/CDS/TB/2003.316).
- Uplekar M et al. Tuberculosis patients and practitioners in private clinics in India. International journal of tuberculosis and lung disease, 1998, 2(4):324–9.
- Hurtig AK et al. Sputum examination for acid-fast bacilli in private laboratories, Kathmandu valley, Nepal. International journal of tuberculosis and lung disease, 1999, 3(11):1009–14.
- Hong YP et al. Treatment of bacillary pulmonary tuberculosis at the chest clinics in the private sector in Korea. International journal of tuberculosis and lung disease, 1993, 3(8):695–702.
- Rangan SG et al. Tuberculosis control in rural India: lessons from public– private collaboration. International journal of tuberculosis and lung disease, 2004, 8(5):552–9.
- Arora VK, Lonnroth K, Sarin R. Improved case detection of tuberculosis through a public–private partnership. Indian journal of chest diseases and allied sciences, 2004, 46(2):133–6.
- Newell JN et al. Control of tuberculosis in an urban setting in Nepal: public–private partnership. Bulletin of the World Health Organization, 2004, 82(2):92–8.
- Arora VK Sarin R, Lönnroth K. Feasibility and effectiveness of a public–private project for improved TB control in Delhi, India. International journal of tuberculosis and lung disease, 2003, 7(12):1131–8.
- Rangans S. The public–private mix in India’s Revised National Tuberculosis Control Programme—an update. Journal of the Indian Medical Association, 2003, 101(31):161–3.
- Vyas RM, Small PM, De Riemer K. The private–public divide: impact of conflicting perception between the private and public health case sectors in India. International journal of tuberculosis and lung disease, 2003, 7(6):543–9.
- Mills A et al. What can be done about the private health sector in low-income countries? World hospitals and health services, 2002, 38(3):24–30,41–4.
- Khan JA, Hussain SF. Anti-tuberculous drug prescribing: doctors’ compliance at a private teaching hospital in Pakistan. Tropical doctor, 2003, 33(2):94–6.
- Lönnroth K et al. Private tuberculosis care provision associated with poor treatment outcome: comparative study of a semiprivate lung clinic and the NTP in two urban districts in Ho Chi Minh City, Vietnam. International journal of tuberculosis and lung disease, 2003, 7(2):165–71.
- Hurtig AK et al. Linking private and public sector in tuberculosis treatment in Kathmandu Valley, Nepal. Health policy and planning, 2002, 17(1):78–89.
- Nshuts L et al. Public and private providers’ quality of care for tuberculosis patients in Kampala, Uganda. International journal of tuberculosis and lung disease, 2001, 4(11):1006–12.
- Murthy KJ et al. Public–private partnership in tuberculosis control: experience in Hyderabad India. International journal of tuberculosis and lung disease, 2001, 5(4):354–9.
- Brugha R, Zwi A. Improving the quality of private sector delivery of public health services: challenges and strategies. Health policy and planning, 13(2):107– 20.


