M. Al-Ramahi,1 A. Mahafzah,2 S. Saleh1 and K. Fram1
ABSTRACT In a prospective controlled study, we aimed to determine the prevalence of Chlamydia trachomatis infection in Jordanian women attending an infertility clinic and whether screening is useful as part of routine investigations for infertility. Two groups of patients (152 infertile patients and 146 control patients) had endocervical swab testing by polymerase chain reaction for the presence of C. trachomatis infection. A total of 6/152 patients in the infertility group tested positive for C. trachomatis (3.9%), compared with 1/146 patients in the control group (0.7%), a difference that was not statistically significant. In view of the tendency toward increased prevalence of C. trachomatis infection, screening women for chlamydial infection as part of routine investigations for infertility is recommended.
Prévalence de l’infection à Chlamydia trachomatis chez des femmes stériles dans un hôpital universitaire de Jordanie
RÉSUMÉ Dans une étude prospective contrôlée, nous avions pour objectif de déterminer la prévalence de l’infection à Chlamydia trachomatis chez des femmes jordaniennes consultant dans un service spécialisé dans les problèmes de stérilité, et l’utilité d’intégrer le dépistage de cette infection aux examens courants pour explorer la stérilité. Deux groupes de patientes (152 femmes stériles et 146 femmes témoins) ont fait l’objet d’une recherche d’infection à C. trachomatis par PCR (réaction de polymérisation en chaîne) sur prélèvement endocervical. Au total, 6 patientes sur les 152 du groupe de femmes stériles étaient positives à C. trachomatis (3,9 %) contre une sur les 146 du groupe témoin (0,7 %), une différence jugée non statistiquement significative. Au regard de la tendance à la hausse de la prévalence de l’infection à C. trachomatis, le dépistage des chlamydioses dans le cadre des examens courants est recommandé.
1Department of Obstetrics and Gynaecology; 2Department of Pathology, Microbiology and Forensic Medicine, Jordan University Hospital, Amman, Jordan (Correspondence to M. Al-Ramahi:
Received: 30/04/06; accepted: 12/07/06
EMHJ, 2008, 14(5): 1148-1154
Introduction
Chlamydia trachomatis is the most common sexually transmitted infection [1]. It can lead to pelvic inflammatory disease (PID), tubal factor infertility or ectopic pregnancy. Most of the infected patients are asymptomatic [2] and are usually recognized when they are routinely screened as part of infertility investigations [3] or before performing a gynaecology procedure [4]. Although infection with C. trachomatis has been suggested to be a cause of infertility due to the sequelae on the genital tract, many gynaecology clinics do not perform routine screening for C. trachomatis. This makes the magnitude of the problem unclear. Many patients are diagnosed to have unexplained infertility without screening for possible genital tract infection, which leads to inaccurate diagnosis. Furthermore, many infertility patients undergo gynaecologic procedures including hysterosalpingography and diagnostic laparoscopy without screening for pelvic infection. This may disseminate a pre-existing infection to the whole genital tract, leading to PID, hydrosalpinx or even pyosalpinx.
This study in one clinic was conducted to determine the prevalence of C. trachomatis infection in Jordanian women attending with primary or secondary infertility and to determine if screening for C. trachomatis is necessary as part of routine investigations of infertility.
Methods
Patients
During the period March 2004 to February 2005, all women who attended the gynaecology clinic at Jordan University Hospital, a general tertiary care hospital that serves patients referred from all over the country, and fulfilled the inclusion criteria were enrolled in the study. The infertility group included women who attended the clinic for primary or secondary infertility. Primary infertility was defined as the inability to conceive after 1 or more years of regular coital activity without contraception, and secondary infertility was defined as the inability to conceive after 6 or more months of regular coital activity without contraception with a history of previous pregnancy. The control group included women who were attending the clinic for other gynaecologic purposes (abnormal uterine bleeding, ovarian cyst, intrauterine device insertion, etc). All the control group women had no complaint of infertility and were in the childbearing ages (18–40 years old) during the study period. Women who were single or who were over 40 years old were excluded from the study.
Specimen collection
Endocervical swabs were collected from 152 infertile women and 146 control women. Each swab was kept in 1.5 mL of a sterile medium containing 6.7 mg/mL KH PO 3.36 mg/mL KH PO , 227 mg/mL sucrose, 50 mg/L gentamicin, 100 mg/L vancomycin and 50 mg/L amphotericin B. Specimens were stored at –70 ºC until used for DNA extraction.
DNA extraction
Swabs were vortexed and rotated at 360 ° against the inner wall of the collection tube to remove as much fluid as possible, transferred to a 1.5 mL Eppendorf tube and centrifuged at 16 000 g for 15 min. The pellet was used for DNA extraction using the salting out procedure as described by Miller, Dykes and Polesky [5]. Briefly the pellet was treated with 900 μL whole cell lysis buffer (0.32 M sucrose, 10 mM tris–HCl pH 7.6, 5 mM MgCl2, 1% Triton X-100) for 2 minutes, centrifuged at 16 000 g for 20 s. The pellet was then resuspended in 500 μL of nuclei lysis buffer (25 mM EDTA pH 8.0, 75 mM NaCl, 50 μL of 10% sodium dodecyl sulfate, and 15 μL proteinase-k (10 mg/mL), and samples were then incubated at 37 ºC overnight. The following day when the samples were completely lysed, 140 μL saturated NaCl solution (approximately 6 M) was added, vortexed and centrifuged, then the DNA was precipitated with 2 volumes of 100% ethanol. The pellet was then washed with 300 μL of 70% ethanol, allowed to air dry, then dissolved with 50 μL water and used for polymerase chain reaction (PCR) analysis directly.
Polymerase chain reaction
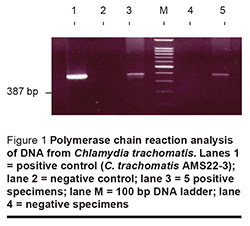
PCR was done using a commercially available kit for the detection of C. trachomatis by amplification of the 60 KD CrP gene (AMS 22-2/F system, Clonit, Milan, Italy), based on a ready-to-use solution that includes well-preserved primers. The amplification product is a 387 bp fragment, which is specific for the C. trachomatis 60 KD CrP gene. For each test 95 μL of amplification solution was mixed with 5 μL of extracted DNA and 2 units of Taq polymerase. PCR amplification protocol was performed in a thermocycler (PTC-100, MJ Research Inc., Watertown, Massachusetts) as follows: 1st cycle denaturation at 94 ºC for 4 min, annealing at 55 ºC for 1 min, extension at 72 ºC for 1 min, followed by 30 cycles of denaturation at 94 ºC for 1 min, annealing at 55 ºC for 1 min, extension at 72 ºC for 1 min and finally cooling at 4 ºC. Negative control samples containing water were always used in parallel to the specimens to detect PCR contamination. Then 10 μL of amplified products were examined at 100 V using 2% agarose containing 0.5 μg/mL of ethidium bromide in 1× tris–boric acid–EDTA buffer. The 387 bp DNA band was visualized under an ultraviolet illuminator and photographed using the GelDoc 1000 documentation system (Figure 1). All procedures were carried out under strict conditions that minimize the risk of DNA carryover.
Ethics
This research project was approved by the research ethics board at Jordan University Medical School. Statistical analyses were preformed using Student t-test, chi-squared test and Fisher exact test where appropriate.
Results
There were 152 women in the infertility group and 146 women in the control group who fulfilled the inclusion criteria in this study. The mean (standard deviation) age of the infertility group was 31.2 (SD 6.1) years compared with 34.2 (SD 8.2) years for the control group (P < 0.001).
Table 1 shows the cause of presentation and the number of positive tests for C. trachomatis for women in the control group. There was no significant difference regarding the cause of presentation to the clinic and the number of positive tests obtained. The cause of infertility and number of positive cases for the infertility group is shown in Table 2. There was no significant difference concerning the cause of infertility and the number of positive tests obtained. There were 6/152 women positive in the infertility group (3.9%) compared with 1/146 women positive in the control group (0.7%). Despite this tendency towards a higher rate of positive tests in the infertility group, the difference was not statistically significant.
The proportion of women testing positive for C. trachomatis in the primary infertility group (2/81, 2.5%) was lower than the proportion testing positive in the secondary infertility group (4/71, 5.6%), but the difference was not statistically significant (Table 3).
Discussion
C. trachomatis is an obligate intracellular pathogen that may cause different clinical diseases including trachoma, genital infections and lymphogranuloma venereum. The mechanism of tissue damage caused by Chlamydia spp. is unclear, but it seems to be related to an immune-mediated inflammatory response [6]. The possible sequelae of chlamydial infection include pelvic damage and transmission of the pathogen to the neonate at birth, causing pneumonia and conjunctivitis [7].
The prevalence of genital chlamydial infection in the United States of America (USA) is estimated to range from 5% to 15% [8], whereas in the United Kingdom (UK) the prevalence of chlamydial infection is about 16% [9]. The reported prevalence of genital chlamydial infection is low in several Eastern Mediterranean countries, probably due to the conservative beliefs in those societies that discourage free sexual relations. In the United Arab Emirates the rate has been reported to be 2.6% [10]. However, the authors noted that they excluded a large population of women aged less than 19 years of age due to cultural and social constraints. Thus no direct comparisons could be made with studies from Europe and USA, which included younger women at high risk of chlamydial infection. A hospital-based study from Jordan reported that the prevalence of chlamydial infection among symptomatic patients was 4.6%, whereas there was no chlamydial infection among asymptomatic patients [11]. In our study the rate of chlamydial infection was 3.9% among women attending for investigation of infertility and 0.7% among a control group of women attending for other reasons.
The prevalence of C. trachomatis infection varies with age, and young adult patients are considered a high-risk group [12]. In our study the mean age of infertile patients was 31 years and for the control patients 34 years. Furthermore, the low prevalence of chlamydial infection may be attributed to the fact that Jordanian society is socially and culturally conservative concerning free sexual relations, and among young adult women sexual activity usually starts with legal marriage.
Several screening tests have been suggested for detecting C. trachomatis infection, including DNA-based tests such as ligase chain reaction (LCR) [13], PCR [14], gene probe [15] and enzyme immunoassay (EIA) [16] using urine or cervical swab samples. A recent meta-analysis demonstrated that DNA amplification techniques, including PCR, performed best for urine and cervical swabs in low prevalence populations [17]. In this study we elected to screen our patients taking endocervical swabs and performing DNA amplification technique using PCR because of the high sensitivity this method provides in detecting chlamydial infection [18].
The aim of detecting infection with C. trachomatis in the lower genital tract is to prevent spreading of infection to the upper genital tract and to prevent further complications in patients who already have upper genital tract infection. Moreover, infection can be disseminated when this group of patients undergoes uterine instrumentation for further evaluation and treatment of their fertility problem. PID following hysterosalpingography has been reported in up to 4% of cases and in 10% of patients having tubal disease [19]. The Royal College of Obstetricians and Gynaecologists recommended that all patients undergoing uterine instrumentation should be screened for Chlamydia spp. or should receive prophylactic antibiotics [20]. In our study, 1 case in the control group and 6 cases in the infertility group were positive for Chlamydia spp., but none of them had documented tubal factor infertility, since occult damage of the tubal cilia or mucosa could not be ruled out. Furthermore, infection could have been limited to the lower genital tract only.
In conclusion, although it was not statistically significant, there was a tendency towards increased prevalence of C. trachomatis infection in infertile patients compared to a control group of women. Therefore, screening of women for C. trachomatis infection is recommended as part of investigations for infertility since infertile patients may undergo further invasive diagnostic and therapeutic procedures that may disseminate a pre-existing asymptomatic infection.
Acknowledgements
This research project was supported by a grant from the deanship of academic research at Jordan University
References
- Paavonen J, Eggert-Kruse W. Chlamydia trachomatis: impact on human reproduction. Human reproduction update, 1999, 5(5):433–47.
- Svensson LO et al. Screening for Chlamydia trachomatis infection in women and aspects of laboratory diagnostics. Acta obstetricia et gynecologica scandinavica, 1991, 70:587–90.
- Thomas K et al. The value of Chlamydia trachomatis antibody testing as part of routine infertility investigations. Human reproduction, 2000, 5(5):1079–82.
- Thomas K, Simms I. Chlamydia trachomatis in subfertile women undergoing uterine instrumentation. Human reproduction, 2002, 17(6):1431–2.
- Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extraction DNA from human nucleated cells. Nucleic acids research, 1988, 16(3):1215.
- Brunham RC, Peeling RW. Chlamydia trachomatis antigens: role in immunity and pathogenesis. Infectious agents and diseases, 1994, 3:218–33.
- Stray-Pedersen B. Is screening for genital infections in pregnancy necessary? Actaobstetricia et gynecologica scandinavica, 1997, 765(Suppl. 164):116–20.
- Mertz JK et al. Trends in the prevalence of Chlamydia infections: impact of community-wide testing. Sexually transmitted diseases, 1997, 24:169–75.
- Pimenta J et al. Screening for genital chlamydial infection. British medical journal, 2000, 321:629–31.
- Ghazal-Aswad S et al. Prevalence of Chlamydia trachomatis infection among women in a Middle Eastern community. BMC women’s health, 2004, 4:3.
- Awwad Z, Amrat A, Shehabi A. Prevalence of genital chlamydial infection in symptomatic and asymptomatic Jordanian patients. International journal of infectious diseases, 2003, 7:206–9.
- Bavastrelli M et al. Sexually active adolescents and young adults: a high risk group for Chlamydia trachomatis infection. Journal of travel medicine, 1998, 5:57–60.
- Gaydos CA et al. Use of ligase chain reaction with urine versus cervical culture for detection of Chlamydia trachomatis in an asymptomatic military population of pregnancy and non pregnant females attending Papanicolaou smear clinics. Journal of clinical microbiology, 1998, 36:1300–4.
- Toye B et al. Diagnosis of Chlamydia trachomatis infections in a symptomatic men and women by PCR assay. Journal of clinical microbiology, 1996, 34:1396– 1400.
- Ferrero DV et al. Performance of the GenProbe AMPLIFIED Chlamydia trachomatis assay in detecting Chlamydia trachomatis in endocervical and urine specimens from women and urethral and urine specimens from men attending sexually transmitted disease and family planning clinics. Journal of clinical microbiology, 1998, 36:3230–3.
- Chernesky MA et al. Diagnosis of Chlamydia trachomatis infections in men and women by testing first-void urine by ligase chain reaction. Journal of clinical microbiology, 1994, 32:2682–5.
- Watson EJ et al. The accuracy and efficacy of screening tests for Chlamydia trachomatis: a systematic review. Journal of medical microbiology, 2002, 51:1021–31.
- Catry MA et al. Comparison of the Amplicor Chlamydia trachomatis test and cell culture for the detection of urogenital chlamydial infection. Genitourinary medicine, 1995, 71:247–50.
- Forsey JP et al. Chlamydia trachomatis, tubal disease and the incidence of symptomatic and asymptomatic infection following hysterosalpingography. Human reproduction, 1990, 5:444–7.
- Initial investigation and management of the infertile couple. London, Royal College of Obstetricians and Gynaecologists, 1996:12.


