R. Hong1 and M. Ruiz-Beltran2
ABSTRACT We examined the risk of infant mortality among low-birth-weight children (< 2500 g) control- ling for other risk factors of infant mortality. We used survival regression analysis on 11 361 childbirths in the 5 years preceding the 2000 Egypt Demographic and Health Survey. Higher birth order; shorter birth interval; lack of prenatal care, safe sources of drinking-water and hygienic toilet facilities; living in urban residence and Upper Egypt rural region were associated with a higher risk of infant mortality. The multivariate model indicated that low-birth-weight children were about 3 times more likely to die in infancy than other children (hazard ratio = 2.89, 95% CI: 2.33–3.58) independent of other risk factors.
Le faible poids de naissance en tant que facteur de risque de mortalité infantile en Égypte
RÉSUMÉ Nous avons examiné le risque de mortalité infantile chez des enfants ayant un faible poids à la naissance (< 2500 g) après élimination des autres facteurs de risque de mortalité infantile. Nous avons utilisé une analyse de régression pour étudier la survie lors de 11 361 accouchements survenus pendant les cinq années qui ont précédé l’Enquête sur la démographie et la santé en Égypte de 2000. Les facteurs associés à un risque accru de mortalité infantile étaient le rang de naissance élevé, les naissances rapprochées, l’absence de surveillance prénatale, le manque de sources d’eau potable et d’installations sanitaires hygiéniques, la vie en milieu urbain et dans les régions rurales de Haute Égypte. Le modèle multivarié indiquait que les enfants ayant un faible poids à la naissance avaient environ trois fois plus de risque de mourir en bas âge que les autres enfants (rapport des risques instantanés [hazard ratio] = 2,89, IC 95 % : 2,33 - 3,58) indépendamment des autres facteurs de risque.
1Department of Global Health, School of Public Health and Health Services, George Washington University, Washington DC, United States of America (Correspondence to R. Hong:
2Division of Immigration Health, United States Public Health Service, Rockville, Maryland, United States of America.
Received: 26/12/05; accepted: 25/05/06
EMHJ, 2008, 14(5): 992-1002
Introduction
There has been a remarkable improvement in child survival in recent decades. However, the levels of infant and child mortality and morbidity in many developing countries remain unacceptably high [1,2]. The mortality rates are particularly high among high-risk pregnancies and births [3,4], and in countries where adequate primary health care services for maternal and child health, such as prenatal care, delivery and postnatal care, are not universally available to all the population, especially the rural population [5,6].
Low birth weight and premature births are high-risk births. These births are frequently accompanied by a number of associated fetal and neonatal complications that need special and expensive medical care [7]. Low-birth-weight babies are also at higher risk of associated birth defects and/or disabilities and account for a larger percentage of prenatal deaths [8]. Therefore, mortality of among low-birth-weight children contributes to the higher rate of overall childhood mortality especially during the early period of life.
In Egypt, as in many other developing countries, most infant and childhood mortality has been also due to diarrhoea, acute respiratory infections, other infectious diseases such as meningitis, neonatal infections, accidents, and vaccine preventable diseases [9]. These conditions are more critical among low-birth-weight children since they are more at risk of premature birth, fetal defects, neonatal complications, deficient immune system and greater exposure to infections [10,11]. In Egypt, even though public health clinics are generally available throughout the country, there are often shortages of doctors and nurses. In both cities and villages, patients using government facilities can expect a lengthy journey and a long wait to see a physician [12–14].
Previous studies have associated high infant mortality with low birth weight in both developed and developing countries, specifically those with birth defects and premature birth. These studies were mainly conducted at the maternity and neonatal clinics, and did not take into account the socioeconomic and demographic factors and household living conditions of the infants and mothers [15,16]. Other previous studies have linked infant mortality with various factors, such as mother’s education, age at childbirth, delivery status, health status, parity and marital union, father’s education and employment, household income and consumer goods, household safe source of drinking-water and sanitation, and slum and rural residence [17,18]. Demographic characteristics such as child’s sex, ethnicity, preceding and succeeding birth interval, birth weight and birth order are also known to be associated with infant mortality [19]. Using data from the 2000 Egypt Demographic and Health Survey, this study examines the effects of several potential risk factors on infant mortality among lowbirth-weight infants in Egypt [20].
Methods
The analysis uses data from the 2000 Egypt Demographic and Health Survey (EDHS) [20]. It is based on the information of 11 361 children born during the 5 years prior to the survey. The EDHS collected demographic, socioeconomic and health data from a nationally representative sample of 15 573 women aged 15 to 49 years in a sample of 16 957 households. The sampling design allowed for estimates of the major administrative regions. The master sampling frame for EDHS was based on the 1996 National Census. The sampling design was a multistage cluster sample consisting of 500 primary sampling units and included 228 towns and 272 villages. Details of the sampling design are provided in the main EDHS report [20].
Each woman age 15–49 years interviewed in the survey was asked to provide a detailed history of all her live births in chronological order, including sex of the child, date of birth, survival status, age of the child on the date of interview if alive, if not alive, age at death of each live birth. These data from the birth history were used to calculate the infant mortality rate, defined as the probability of dying before completing 12 months of age, using a synthetic cohort life table [21]. The infant mortality rate is expressed as deaths per 1000 live births. Low birth weight was defined as birth weight < 2500 g if the actual birth weight was known. In cases where the birth weight was not available, the mother was asked about the size at birth: very small/ small was categorized as low birth weight (< 2500 g), average/large as normal birth weight (≥ 2500 g).
Because child survival is correlated with prenatal care, delivery assistance, maternal nutrition, household living conditions, and other child, mother and household characteristics and socioeconomic factors that can also affect morbidity and mortality in children, the association of low birth weight and infant mortality were estimated after adjusting for the effects of these other risk factors and potentially confounding factors [22]. These factors include child’s sex (boy, girl), prenatal care by health professional (yes, no), professional assistance at delivery (yes, no), birth order (1, 2, 3, 4+), preceding birth interval (< 23, 24–35, 36–59, 60+ months), mother’s age at childbirth (13–24, 25–34, 35–48 years), mother’s body mass index (BMI) (< 18.5, 18.5–24.9, 25.0+ kg/m2), mother’s education (no education, some primary, secondary or higher), household access to safe drinking water (yes, no), availability of hygienic toilet facilities (yes, no), cooking fuel type (low pollution fuel, high pollution fuel), residence (urban, rural), and geographic division (urban governorate, Lower Egypt–urban, Lower Egypt–rural, Upper Egypt–urban, Upper Egypt–rural, frontier governorates).
The relationship of low-birth-weight status and other factors with infant mortality was estimated using multivariate survival regression procedure with Weibull hazard function in STATA, version 8.0. A number of alternative hazard regression models were estimated to assess the relative significance of different confounding factors included in the analysis. In our analysis, weights were used to restore the sample as some categories of respondents were over-sampled and to adjust for non-response rates that varied from one geographical area to another [20]. Results are presented as hazard ratios (HR) with 95% confidence intervals (95% CI).
Results
Table 1 shows the sample distribution of child birth in the 5 years preceding the EDHS by low-birth-weight status and other selected characteristics. About 16% of children born between 1996 and 2000 were low birth weight. About 51% of all births were boys and 49% were girls. As regards birth order, 27% of children were first order births, and 33% were fourth or higher order births. About 45% of children had a preceding birth interval of less than 24 months. In 53% of the births, mothers received prenatal care from trained health personnel and 60% received professional assistance at delivery. About 11% of births were to mothers aged 13–24 years, and 29% to mothers aged 35–48 years. Less than 1% of the births were to undernourished mothers (BMI < 18.5 kg/m2), 40% of the births were to illiterate mothers and 86% were to non-working mothers. About 87% of children were born in households with safe sources of drinking-water, 25% were in households with hygienic toilet facilities, and 3% were in households using high pollution fuels (firewood or straw) for cooking. Almost 62% of births were in rural areas.
The prevalence of low birth weight was slightly higher among girl babies, first order babies, those with shorter preceding birth interval, those who received prenatal care, those who received delivery assistance and younger mothers. Low birth weight was also associated with a lack of hygienic toilet facilities, using high pollution cooking fuel, rural residence and Upper Egypt rural region.
On average, 42 in every 1000 children born between 1996 and 2000 in Egypt did not survive to her or his first birthday. As expected, the infant mortality rate was higher among low-birth-weight children—87 per 1000 live births compared to only 31 per 1000 live births among the children weighing ≥ 2500 g. Infant morality was highest in children of fourth order birth or higher and preceding birth < 24 months. Children of mothers who did not receive prenatal care or assisted delivery were more likely to die during infancy as were children born to younger mother (13–24 years old) or older mothers (35–48 years old) were at greater risk of infant mortality.
Household lack of a hygienic toilet facilities and access to safe drinking-water was also associated with higher risk of infant mortality. As expected, infant mortality rate is lower in urban areas, particularly so in Upper Egypt.
Association between low birth weight and infant survival
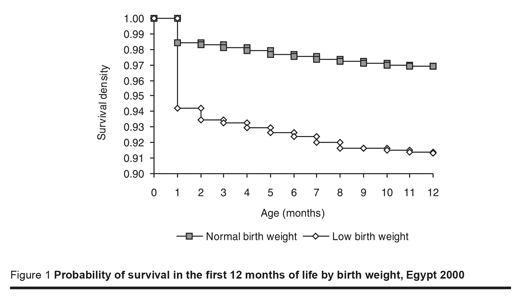
For children born in the 5 years preceding EDHS, Figure 1 shows survival probabilities for children by low-birth-weight status by month of age before 12 months. The 2 survival curves quickly diverge beyond the first month of age, with low-birth-weight children having progressively lower survival probability than children with birth weight ≥ 2500 g with a large majority of low-birth-weight children dying in infancy. The unadjusted HR estimates in Model 1 (Table 2) also indicate that there is a strong relationship between low birth weight and infant mortality. Children with low birth weight are about 3 times more likely to die in infancy than those with birth weight ≥ 2500g (HR = 2.96, 95% CI: 2.41–3.64).
The HR of low birth weight on infant mortality remains large and highly statistically significant when the effects of child’s sex, prenatal care, professional assistance at delivery and birth order are controlled for in Model 2. With these child/birth characteristics controlled for, low-birth-weight children were 2.95 times more likely to die in infancy than those with birth weight ≥ 2500 g.
Additionally, adjusting for mother’s age at childbirth, BMI, education and working status in Model 3 had little influence on the size of the relationship. In the full model (Model 4), when household access to safe drinking-water, availability of a hygienic toilet facilities, type of fuel used for cooking, urban/rural residence, and geographic division were also controlled for, the relationship of low birth weight and infant mortality remained large and significant. With all child, maternal, household, and regional factors controlled for, low-birth-weight children were about 3 times more likely to die in the first year of life than those with birth weight ≥ 2500 g (HR = 2.89, 95% CI: 2.33–3.58).
Effects of other risk factors and confounders on infant survival
In Model 4 (Table 2), with low-birth-weight status and other factors controlled, children born to mothers who did not receive prenatal care were more likely to die before reaching their first birthday than children of mothers who did receive prenatal care (HR = 1.35, 95% CI: 1.08–1.69). Children of fourth order birth or higher and children with preceding birth interval shorter that 24 months were significantly more likely to die before their first birthday than other children. Also children living in households without a safe source of drinking-water and hygienic toilet facilities were about one and a half times more likely to die before 12 months of age than children living in households with a safe source of drinking-water and hygienic toilet facilities. Children living in rural areas had a lower risk of dying before 12 months of age than children in urban areas (HR = 0.30, 95% CI: 0.10–0.90).
However, children living in rural Upper Egypt were at a significantly higher risk of mortality in infancy than children living in other geographical regions (HR = 3.83, 95% CI: 1.20–12.22) (Table 2). None of the other risk factors or confounders had a statistically significant effect on the risk of infant mortality.
Discussion
Low birth weight is associated with higher infant mortality due to premature birth, greater probability of birth defects and complications, higher risk of neonatal infection, and lack of access to adequate health care. The results of our study show that infant mortality is high in Egypt (42 per 1000 live births), and the mortality among low-birth-weight births contributes to a higher rate of overall mortality in infancy. Low-birth-weight infants are 3 times more likely to die during the first year of life than other children, independent of the child’s sex, birth order, pregnancy care, delivery status, maternal education and nutritional status, household access to clean water and sanitation and other factors. These findings are consistent with the results from other studies in developing countries in the region and elsewhere [23–27], and provide further evidence that low birth weight contributes to higher levels of child mortality in developing countries.
Consistent with previous research, our study finds that receiving prenatal care has a strong positive effect on child survival, independent of other factors [28]. Moreover, access to safe drinking-water and hygienic toilet facilities in household has a significant effect on the risk of infant mortality [29]. Also, children living in Upper Egypt rural regions are at higher risk of dying in infancy than children living in other regions. However, contrary to expectations and much of the existing literature, we did not find any significant effects of maternal education, nutritional status, and type of household cooking fuel on the risk of infant mortality. The negative relationship between rural residence and child survival, observed when considered a bivariate analysis, was reversed in the multivariate model. This might be because the urban/rural residence variable is correlated with the geographic region variable and other socioeconomic factors such as water, toilet facilities and cooking fuel.
In previous research, mother’s education has been identified as one of the key factors in promoting child survival [30]. However, in our analysis, maternal education was not found to have any significant effect on infant mortality, and controlling for maternal education had little influence on the effects of low birth weight on infant mortality. Similarly, a lack of a significant relationship of infant mortality with cooking fuel type may partly be because the majority of the children (97%) lived in households using low pollution biomass fuels for cooking.
This study has a number of limitations. The first is its inability to control for morbidity at birth but the EDHS did not collect information on the morbidity of the children at birth. The second potential limitation is that it did not account for access to health care indicators. However, our analysis does include indicators of mothers’ receiving prenatal and delivery care, which can be proxies for mothers’ seeking health care for their young children. The third limitation is that the survey was conducted in 2000. However the level of infant mortality and the prevalence of low birth weight are unlikely to have changed significantly in this short period of time, and the results from this study still contribute useful knowledge in the subject area. Another potential limitation is the cross-sectional nature of our analysis. The study uses a censored, synthetic cohort life table based on the birth history of children and reported characteristics of mothers and households. While some of the covariates used in our analysis, such as child’s sex, prenatal care, delivery care, mother’s age at childbirth, and birth weight, are fixed covariates, others, such as mother’s education, household access to clean water and sanitation, and urban/rural residence are time-varying covariates. In our analysis, all covariates were considered fixed during the study period. However, because these time-varying covariates may not have changed much during the study period and because the main finding in our analysis is the relationship of low-birthweight status and child survival, the crosssectional effects estimated in this study are a good measure of the relationship between low birth weight and infant survival.
Despite these potential limitations, consistency in the direction and strength of the relationship between low birth weight and infant mortality suggests that the following are key to improving child survival in Egypt: improving public health at the community level, specifically screening for high-risk pregnancy and premature birth, and making referral services for these conditions more available and accessible to the rural population; and improving social services, such as provision of safe drinking-water and hygienic waste disposal.
References
- Human Development Report 2004. New York, United Nations Development Programme, 2004.
- World Development Report 2000. Washington DC, World Bank, 2000.
- Macassa G et al. Inequalities in child mortality in Mozambique: differentials by parental socioeconomic position. Social science & medicine, 2003, 57(12):2255– 64.
- Garenne ML, Coninx R, Dupuy C. Effects of the civil war in central Mozambique and evaluation of the intervention of the International Committee of the Red Cross. Journal of tropical pediatrics, 1997, 43(6):318–23.
- Thang NM, Popkin BM. In an era of economic growth, is inequity holding back reduction in child malnutrition in Vietnam? Asian Pacific journal of clinical nutrition, 2003, 12(4):405–10.
- Zere E, McIntyre D. Inequities in underfive child malnutrition in South Africa. International journal of equity health, 2003, 2(1):7.
- Ades A, Johnson BA, Berger S. Management of low birth weight infants with congenital heart disease. Clinical perinatology, 2005, 32(4):999–1015.
- Halbreich U. The association between pregnancy processes, preterm delivery, low birth weight, and postpartum depressions—the need for interdisciplinary integration. American journal of obstetric & gynecology, 2005, 193(4):1312–22.
- Yassin KM. Indices and sociodemographic determinants of childhood mortality in rural Upper Egypt. Social science & medicine, 2000, 51:185–97.
- Velaphi SC et al. Survival of very-lowbirth-weight infants according to birth weight and gestational age in a public hospital. South African medical journal, 2005, 95(7):504–9.
- De Felice C, Del Vecchio A, Latini G. Evaluating illness severity for very low birth weight infants: CRIB or CRIB-II? Journal of maternal–fetal and neonatal medicine, 2005, 17(4):257–60.
- Youssef RM et al. Correlates of unintended pregnancy in Beheira governorate, Egypt. Eastern Mediterranean health journal, 2002, 8(4–5):521–36.
- Cherine M et al. Management of the third stage of labor in an Egyptian teaching hospital. International journal of gynaecology & obstetrics, 2004, 87(1):54–8.
- Gadallah M et al. Patient satisfaction with primary health care services in two districts in Lower and Upper Egypt. Eastern Mediterranean health journal, 2003, 9(3):422–30.
- Hillemeier MM et al. Relative or absolute standards for child poverty: a statelevel analysis of infant and child mortality. American journal of public health, 2003, 93(4):652–7.
- Kiros GE, Hogan DP. War, famine and excess child mortality in Africa: the role of parental education. International journal of epidemiology, 2001, 30(3):447–55; discussion 456.
- Cutts FT et al. Child and maternal mortality during a period of conflict in Beira City, Mozambique. International journal of epidemiology, 1996, 25(2):349–56.
- Choe MK et al. Identifying children with high mortality risk. National family health surveillance bulletin, 1999, (12):1–4.
- Menezes AM et al. Infant mortality in Pelotas, Brazil: a comparison of risk factors in two birth cohorts. Revista panamericana de salud pública, 2005, 18(6):439–46.
- Ministry of Health and Population [Egypt], National Population Council, ORC Macro. Egypt Demographic and Health Survey 2000. Calverton, Maryland, ORC Macro, 2001.
- Rutstein SO, Rojas G. Guide to DHS statistics. Calverton Maryland, ORC Macro, 2003.
- Defo BK. Areal and socioeconomic differentials in infant and child mortality in Cameroon. Social science & medicine, 1996, 42(3):399–420.
- Morales LS et al. Mortality among very low-birthweight infants in hospitals serving minority populations. American journal of public health, 2005, 95(12):2206–12.
- Ezeaka VC et al. Outcome of low birth weight neonates in a tertiary health care centre in Lagos, Nigeria. African journal of medicine & medical science, 2004, 33(4):299–303.
- Cockey CD. More babies born at very low birth weight linked to rise in infant mortality. AWHONN lifelines, 2005, 9(2):113– 21.
- Shawky S. Infant mortality in Arab countries: sociodemographic, perinatal and economic factors. Eastern Mediterranean health journal, 2001, 7(6):956–65.
- Casterline JB, Cooksey EC, Ismail SF. Infant and child mortality in rural Egypt. Journal of biosocial science, 1992, 22(2):254–60.
- Adam T et al. Cost effectiveness analysis of strategies for maternal and neonatal health in developing countries. British medical journal, 2005, 331(7525):1107.
- Shawky S. Infant mortality in Arab countries: sociodemographic, perinatal and economic factors. Eastern Mediterranean health journal, 2001, 7(6):956–65.
- Machado CJ, Hill K. Maternal, neonatal and community factors influencing neonatal mortality in Brazil. Journal of biosocial science, 2005, 37(2):193–208.


