G.H. Yaghoubi1 and B. Heidari1
1Ophthalmology Department, Valiasr Hospital, Birjand Medical University, Birjand, Khorasan, Islamic Republic of Iran (Correspondence to Yaghoubi Gholam Hossin:
Received: 15/12/05; accepted: 20/06/06
EMHJ, 2008, 14(5): 1225-1227
Introduction
Central retinal artery occlusion is a rare event and the site of obstruction is not usually visible on clinical examination; therefore, the precise cause is often speculative. It is currently believed that the majority of central retinal artery obstruction is caused by thrombus formation. Atherosclerosis is implicated as the contributory event in most cases, although congenital anomaly of the central retinal artery, systemic coagulopathies, inflammation, or low flow states from more proximal arterial disease may also be present and make certain individuals more susceptible. Further indirect evidence against emboli as a frequent cause of central retinal artery obstruction is the 40% or less probability of finding a definitive embolic source on systemic evaluation and the small incidence of confirmed associated ipsilateral cerebral emboli in affected patients [1,2]. There are many reports that find an association between smoking and cardiovascular disease and the incidence of retinal emboli [3,4].
In this report we describe a case of a man with central retinal artery occlusion that occurred 2 weeks after stopping cigarette smoking.
Case report
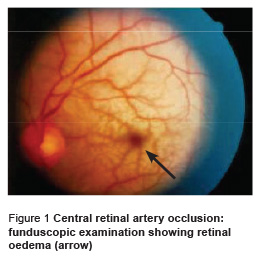
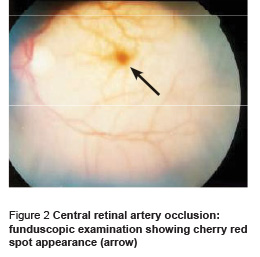
In December 2004, a 28-year-old farmer presented at the eye clinic of Valiasr Hospital complaining of acute loss of vision in the left eye 10 days after he had stopped cigarette smoking. The patient’s vision had been good and he had never had any complaints about his vision before this event. He had a 10-year history of smoking (at least 20 cigarettes a day) but no history of diabetes mellitus, hypertension, cardiac or hepatic disease. Visual examination of the left eye showed poor light perception, 3.5+ relative afferent pupillary defect and eyeball pressure was 13 mmHg. Funduscopic examination showed mild optic papilla redness, retinal paleness and oedema (enlarged, sausage-like vein) (Figure 1) and macular oedema (cherry-red spot) (Figure 2). The right eye visual acuity was 10/10 and ophthalmic examination was normal. The patient was diagnosed with central retinal artery occlusion in the left eye occurring 2 weeks after stopping cigarette smoking.
The patient refused to be hospitalized and was treated with compression, oral prednisolone 75 mg/day, analgesics, timolol drops and acetazolamide 250 mg every 6 hours. However, this treatment did not give a beneficial result and on the 3rd day there was no improvement of vision. The patient was told to come back for further eye and paraclinical evaluation. On the 7th day of occlusion, there was still no improvement in the left eye and routine laboratory examination (complete blood count, lipid profile, renal and hepatic function test and cardiovascular and carotid vessel) were within the normal range.
In a final follow-up after 1 year, there was no improvement in visual acuity but also no complications such as neovascularization, neovascular glaucoma or phthisis bulbi.
Discussion
In this case, the patient diagnosed with central retinal artery occlusion was a young man with no history of any systemic disease. He had a 10-year history of cigarette smoking, but when the occlusion happened he had not been smoking for 10 days. In our patient, laboratory tests, including complete blood count, and liver and renal function tests, were within normal range. We could not find any abnormality on Doppler evaluation of the carotid artery or echography of the heart, which can rule out those sites as the source of embolism. Indeed the absence of an embolus in the retinal artery means the occlusion was not caused by this.
The pathological physiology of central retinal artery occlusion in this case may be due to the following possible alternatives: acute homodynamic change that may appear after smoking cessation; coincidental occurrence; or smoking may be a risk factor for central retinal artery occlusion in this age as discussed by Von Mach and colleagues [5]. However, in this case, the cause of the occlusion was not determined.
Treatment of central retinal artery occlusion can be categorized as conservative (ocular massage, pharmacological treatment, anterior chamber paracentesis) or invasive (catheterization of the proximal ophthalmic artery through the femoral artery with the infusion of thrombolytic agents). However, to date, no satisfactory therapy is available for patients with this disorder [6,7] and in most cases therapy is not successful. In our patient, after 5 days of appropriate treatment and medication, no improvement in visual acuity was observed.
There is lack of a full understanding of the basic scientific facts of acute retinal vascular occlusive disorders, which has led to numerous misconceptions and hence controversy about their pathogenesis, clinical features and treatment [8]. In spite of many searches in the literature we could not find another report of a case such as ours, so this paper may provide further information about this condition.
References
- Yanoff M, Duker JS. Ophthalmology, 2nd ed. New York, Mosby, 2004:854–8.
- Weger M et al. Role of the interleukin-6 -174 G>C gene polymorphism in retinal artery occlusion. Stroke, 2005, 36(2):249–52.
- Wong TY, Klein R. Retinal arteriolar emboli: epidemiology and risk of stroke. Current opinions in ophthalmology, 2002, 13(3):142–6.
- Klein R et al. Retinal emboli and cardiovascular disease: the Beaver Dam Eye Study. Archives of ophthalmology, 2003, 121(10):1446–51.
- Von Mach MA et al. Systemische fibrinolytische Therapie mit Urokinase bei Zentralarterienverschluss der Netzhaut. Eine Fallstudie [Systemic fibrinolytic therapy using urokinase in central retinal artery occlusion. A case study]. Deutsche medizinische Wochenschrift, 2005, 130(16):1002–6.
- Rumelt S, Brown GC. Update on treatment of retinal arterial occlusions. Current opinions in ophthalmology, 2003, 14(3):139–41.
- Werner D. Accelerated reperfusion of poorly perfused retinal areas in central retinal artery occlusion and branch retinal artery occlusion after a short treatment with enhanced external counterpulsation. Retina, 2004, 24(4):541–7.
- Hare SS. Prevalent misconceptions about acute retinal vascular occlusive disorders. Progress in retinal and eye research, 2005, 24(4):493–519.


