A.A. Ishak,1 N.H. Al-Jayefy1 and Y.A. Raja’a2
مرتسم الحالات الطارئة في طب الأطفال في اليمن: الحاجة إلى دلائل إرشادية مسندة بالبينات
اسحق، الجايفي، رجاعة
الخلاصـة: هدفت هذه الدراسة إلى تقديم وصف لأوضاع وأوصاف الأطفال المصطحبين إلى أقسام خدمات الطوارئ في المستشفيات والمراكز الصحية في اليمن من أجل توفير المعلومات الخاصة بإعداد دلائل إرشادية للخدمات الطارئة في طب الأطفال. وقد جمعت المعلومات من 3454 حالة من سبع مستشفيات ومركزين صحيـين في خمس محافظات، وكانت معظم الحالات لأطفال أصغر من عامين من العمر. وكانت غالبية الحالات الطارئة في الأطفال بسبب مشكلات بالجهاز التنفسي (28.6%) ومشكلات مَعِدِية معوية (25.5%)، وقد راجع 36.4% من الأطفال وهم يعانون من هـذه المشكلات مدّةً تجاوزت الأربعـة الأيـام. وقد عولج ثلث عدد الأطفـال (33.2%) باستخدام الجيل الثالث من السيفالوسبورينات cephalosporins وحده أو متـرافقا مع مضادات حيوية أخرى. وبلغت معدلات الوفيات 1.9%، وتمثَّلت أهم أسباب الوفاة في الفشل القلبي والفشل التنفسي.
ABSTRACT: This study describes the status and characteristics of children presenting to emergency services in hospitals and health centres in Yemen in order to inform the development of guidelines for paediatric emergency services. Information was collected from 7 hospitals and 2 health centres in 5 governorates about 3454 cases, mostly aged < 2 years old. The majority of paediatric emergency cases were due to respiratory system problems (28.6%) and gastrointestinal problems (25.5%); 36.4% of children presented with a duration of complaint exceeding 4 days. One-third of cases (33.2%) were treated with 3rd generation cephalosporins alone or in combination with other antibiotics. The mortality rate was 1.9%. The most important causes of death were cardiac and respiratory failure.
Profil des cas d’urgence pédiatrique au Yémen : nécessité de principes directeurs reposant sur des bases factuelles
RÉSUMÉ: Dans le cadre de cette étude, nous avons décrit la situation et les caractéristiques des enfants qui arrivent dans les services d’urgences des hôpitaux et des centres médicaux du Yémen afin de contribuer à l’élaboration de principes directeurs destinés aux services d’urgences pédiatriques. Les informations ont été recueillies auprès de sept hôpitaux et de deux centres médicaux de cinq gouvernorats, à propos de 3454 cas pour la plupart âgés de moins de deux ans. La majorité de ces cas d’urgence pédiatrique étaient dus à des troubles de l’appareil respiratoire (28,6 %) et à des troubles gastro-intestinaux (25,5 %) ; à leur arrivée, 36,4 % des enfants se plaignaient depuis plus de quatre jours. Un tiers des cas (33,2 %) ont été traités avec des céphalosporines de troisième génération, seules ou associées à d’autres antibiotiques. Le taux de mortalité était de 1,9 %. Les causes de décès les plus importantes étaient l’insuffisance cardiaque et l’insuffisance respiratoire.
1Department of Paediatrics; 2Department of Community Medicine, Faculty of Medicine and Health Sciences, Sana’a University, Sana’a, Yemen (Correspondence to Y.A. Raja’a:
Received: 12/09/05; accepted: 05/02/06
EMHJ, 2008, 14(2): 366-375
Introduction
The majority of the population of Yemen are still living in rural areas, but the proportion decreased from around 82% in 1988 to 73% according to the 2003–04 annual statistical report of the Yemeni Ministry of Population and Public Health. Although mortality rates have declined due to better socioeconomic status and better health care coverage, the rates are still relatively high, especially in rural areas [1,2].
The paediatric emergency services play a very important part in the prevention of disease and disability. However, the high cost of these services, which are based on high-cost technology serving a minority of conditions, has to be considered in relation to the needs of the majority of patients and the community. Therefore, there is a need for guidelines that address how to prevent complications arising from emergencies with minimal or no intervention [3,4].
Health services have mostly been developed on vertical selective programmes that address priority diseases. Paediatric emergency services are delivered as part of the overall health delivery system. Duke et al. have shown in a study of 21 hospitals in developing countries that the lack of quality paediatric care may result in unnecessary suffering or avoidable death [5]. In Yemen the quality of paediatric emergency services is affected by the lack of clinical practice protocols adapted to local circumstances, the weakness of the referral system, the underdeveloped administrative and technical setup, and a lack of public awareness and participation. Although there may be some individual efforts and protocols for treatment of certain diseases in the field of emergency medicine, a uniformity of approach and local adaptations are urgently needed. Local adaptation may be difficult due to the fact that practising physicians in Yemen have pursued their training in an array of medical schools in different languages.
Pre-hospital care is another very important aspect of paediatric emergency services capable of greatly contributing to minimizing complications. Yet, knowledge, facilities and experience at the level of health providers and the public at large may be limited or non-existent.
Primary care services in Yemen started to take shape with the development of a locally adapted module of the Integrated Management of Childhood Illnesses (IMCI) strategy, which gives a good background for similar modules at higher levels of service. Quality paediatric emergency services at primary care level essentially depend on the recognition of danger signs and then referral to higher levels of care. However, the IMCI guidelines and the training modules do not include essential pre-hospital care methods that are needed for teaching not only to primary care workers but also to the public [6].
In the field of paediatric emergency services, families lack basic knowledge, experience and support, such as pre-hospital care and social services. A significant proportion of the cost of health care is also borne by families in spite of the fact that government legislation includes the free provision of medical services to the public. The economic burden on the family due to expensive social habits such as chewing khat (a strong habit-forming plant [7]) or smoking cigarettes reduces a family’s capacity to cope with health care costs.
This study aims to describe the status and characteristics of children presenting to emergency services in hospitals and health centres in Yemen in order to add local input to the development of guidelines for paediatric emergency services.
Methods
Setting
This descriptive study was conducted in 7 hospitals located in 5 out of the 15 governorates of Yemen over the period May to December 2004. The sites were selected to represent the various geographical areas of the country, including the highlands, the midlands and the coastal areas. Different categories of hospitals were also represented at a range of levels: 2 teaching and referral hospitals, 2 large and 2 small hospitals and 1 private hospital; 2 health centres were also chosen (1 in a highland and 1 in a coastal area).
Data collection
We studied 3454 paediatric emergency cases: 10.7% from health centres and 89.3% from hospitals. For the purpose of our study we defined a paediatric emergency case as a child aged 0–16 years which needed immediate intervention to save life or prevent complications.
For each case, pre-emergency, emergency and personal characteristics were recorded using a datasheet compiled by physicians at the medical emergency departments at the hospitals and health workers at the health centres. Other data were collected directly from the adult who brought the child, the majority being one or both of the parents. Data collectors were medical care providers at the health care facility in the targeted governorates during the process of medical care. They were trained by the principal investigator during the preparatory stage of the research. The purpose of the study was explained to all of them and each investigator was asked to record the scheme of management of each case. A draft of our future common guidelines was given to each hospital in order be used in the process of care, inviting at the same time comments on the guide, based on local and personal experience of the participants in the study. The activity of the research was planned to be followed by a workshop in order to study the data and the experience during the study period in order to provide practical experience to the guide for doctors in the hospital, especially the role of doctors in the IMCI system of care. The workshop was conducted a few months after the end of the study; follow-up of the development of common local protocol is still in progress by the principal investigator.
The patients were all paediatric emergency cases attending for emergency care at hospitals or during general sessions at primary care centres during the study period. The data collected from parents included: personal information; family and social history; transport conditions; duration of complaint; and cost of treatment. Data recorded by the health care provider providing the immediate care to the patient were: diagnosis; management of the case; and use of drugs.
A separate questionnaire was designed to obtain some baseline data about the rates and types of childhood accidents in the past year, in order to inform campaigns to raise public awareness about childhood accidents. It was a retrospective study conducted at the same time as the main survey from parents who were in the hospital for any purpose of care and a few questionnaires were distributed to other institutions and women’s gatherings. Information was collected by volunteers, who were able to fill in the simple self-administered questionnaire.
Data analysis
Initial evaluation of the data from health centres and hospitals suggested that the findings were homogenous and therefore the data were pooled and analysed collectively. The collected data was entered into a computer and analysed using SPSS, version 11.5, to calculate frequencies.
Results
The total number of paediatric emergency cases recorded was 3454; 59% were males and 41% were females. Data were missing for many variables due to either recall problems or work pressure during the emergency care.
The age range was 0–192 months and the median age was 14 months. A total of 60% were below the age of 2 years (Table 1). Patients attended in similar numbers on all days of the week, mostly between 06.00 and 12.00 hours (48.4%, 1433/2959 visits for which data was available).
Out of 320 cases where the attendant answered the question about transportation time, 47% reported that they took more than 30 minutes to reach the hospital, and no cases were transported by ambulance.
In almost half of the 3209 cases (1459, 48.3%) the child’s attendant had not sought any medical advice before the visit to the emergency department. The remaining cases had been seen in a hospital (670, 20.9%), private practice (454, 14.1%) or health centre/primary care unit (470, 14.6%), more than one place (66, 2.1%); only 0.3% (11) were seen by a non-professional worker.
The cumulative duration of complaints was: 1 day for 17.3% of cases, 2 days 37.7%, 3 days 54.4% and 4 days 63.5%. The duration of complaint was > 4 days in 36.5% (1179/3232) of cases. Of these, 14.1% (166) had respiratory problems and 17.4% (206) had diarrhoea.
Table 2 shows the conditions of the children during transport, as reported by the attendant who brought the child (in most cases the parents). Over half (57.8%) were suffering from respiratory or gastrointestinal infections.
Table 3 shows the distribution of cases by body system affected. Respiratory problems were 28.6%, diarrhoea and dehydration 25.5%, high fever 11.0%, and coma and shock 1.4%. Of the respiratory infections 16% were due to pneumonia (no specific causes recorded) and the rest were due to bronchial asthma.
Table 4 shows the distribution of cases by diagnosis. The majority of specific diagnostic conditions were labelled as gastroenteritis, pneumonia, high fever, febrile conditions, etc. Other reported conditions represented all systems but in relatively few numbers.
Out of 2687 patients investigated, at least 1 laboratory test was done for almost 95%. Some of these tests were: complete blood count and other haematological studies (15.0%), chest X-ray (10.2%) and serum electrolytes (3.6%). Side laboratories operated by physicians (i.e. facilities for rapid diagnosis such as tapes, microscope and slides for blood picture, blood sugar and blood urea, etc.) were not available in any of the research sites. The possibility of accurate diagnosis supported by laboratory evidence was not possible for the majority of diagnostic conditions, such as diarrhoea, respiratory infection and fever. Some cases were already diagnosed, such as sickle-cell anaemia, 2.3% (n = 78) and cardiac conditions, including congenital and rheumatic heart diseases 3.3% (n = 108).
Management
Table 5 shows the use of antibiotics in the paediatric emergency services. The majority of children treated were given a combination of at least 2 antibiotics. Cephalosporins alone or in combination comprised 32% of all cases, of which 1st generation cephalosporins represented 0.4% while the 3rd generation cephalosporins represented 12.6%.
Other drugs were used for 1440 cases (41.7%): cortisone (12.2%), diuretics (12.0%), diazepam (11.2%) and dopamine (9.7%).
A total of 9.9% of children were given cardiopulmonary resuscitation, 8.0% were given a blood transfusion, and 30.0% were put on oxygen therapy. Two thirds of patients (2326/3454, 67.3%) were put on intravenous fluids and analysis of 1763 cases where information was available showed that 3.5% had saline, 14.7% glucose, 44.1% glucose saline and 13.5% Ringer’s solution.
Parent’s characteristics
The majority of mothers were housewives (n = 3207, 92.8%) and were present at the child’s examination in 83.3% of cases (n = 2876). The occupation of fathers was: labourer (36.4%), employee (8.5%), private business (17.8%), student (1.4%), unemployed (8.5%) and other/unknown (4.7%). Fathers were present at 76.1% of examinations (n = 2630). The proportion of mothers who reported chewing khat and smoking tobacco was 8.5% and for fathers the rate was 46.6%.
Results of analysis of 246 questionnaires about childhood accidents showed that 16.2% were falls from a height, 15.5% car accidents and 10.0% burns and scalds; other forms of violence were solid object wound (8.0%), stab wound (5.0%), gunshot wound (2.0%) and drug poisoning (6.0%).
Outcomes
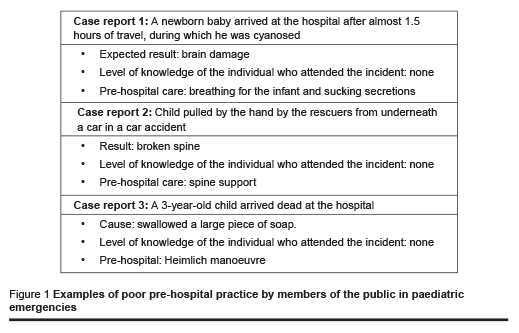
Table 6 reveals that 1.9% of the paediatric emergency cases (n = 65) died. Out of those children, 1 died suffocating from a foreign body and 1 was a victim of a car accident who had a broken spine caused by the rescuers. Causes of death were mostly cardiac (32%) and respiratory (20%). In Figure 1 we summarize 3 cases, examples of poor pre-hospital practice by members of the public in paediatric emergencies, in order to give examples of problems which could have been prevented by correct pre-hospital care.
Cost
The answers to the questions on costs of emergency treatment were very difficult to analyse because of the difficulty in categorizing them, as the majority of parents tended to exaggerate the cost and or confuse the treatment and other costs. Although the treatment of emergency cases is generally free, patients have to pay for medical supplies and in some hospitals there is also a nominal fee. Our estimate of the average cost of medical care, subsidies and transport for a case of febrile convulsions was around US$ 34.
Discussion
Yemen is a country which suffers a heavy burden of infection and malnutrition; this is partially due to people’s lifestyle and the country’s ecology. Moreover, emergency situations are further complicated due to the effects of “haphazard modernization” in terms of misuse of drugs, exposure to chemicals, motor car accidents and even from lack of, or improper, medical services [1–3].
The overall impression from our exploration of paediatric emergency services is that there is no system of practice followed (initial triage, assessment, monitoring, uniform definitions and documentation, follow-up, etc.). This agrees with observations on paediatric emergency services in other underdeveloped countries [4,5].
The age and sex distribution of children showed that the majority were males below the age of 12 years of age. A high proportion of our paediatric emergency cases presented late to the hospital or health centre (over 60% with a duration of complaint of 4 days), which has a negative impact on the outcome. Most of them were cases of diarrhoea and respiratory illnesses, which are the most common presenting diagnoses to both emergency and non-emergency services among Yemeni children. Generally speaking, these conditions are at the top of the list as presenting symptoms according to previous surveys over the past 2 decades [1]. From a study in India it has also been shown that diarrhoea and acute respiratory infections are the most important reasons for utilization of primary and secondary levels of paediatric emergency services [8].
The use of antibiotics shown by our survey reflects more a prescribing habit than a prescribing rationale, and effective drug promotion rather than drug information. Of all drugs used 51% were prescribed for respiratory infections, either 3rd generation cephalosporins alone or a combination of broad-spectrum penicillin and/or aminoglycosides. Compliance with the use of antibiotics is difficult for patients’ families when we take into account the high cost of drugs and the fathers’ occupation (36.4% of all the patients’ attendants were labourers who depend on daily wages). The development of organisms resistant or multiply resistant to antibiotics is disastrous to the health of the community at large. The problem is even more serious in situations of poor quality control, i.e. a lack of proper guidelines on alternatives to technological facilities in the process of clinical decision-making and rational use of antibiotics [9,10].
Cardiopulmonary resuscitation was applied to only few cases, suggesting that very few staff are actually trained and very few sites have the technical facilities for simple life support. Prehospital knowledge and practice is deficient in this area of care. We felt that there is a need to educate the general public, especially parents, about the correct methods of prehospital care for problems such as suffocation, ingestion of foreign bodies, burns, etc. Other research shows that many children in developing countries die before reaching any health facility and many more die because there is no chance to reach a health facility [11].
The use of intravenous fluids in this survey suggests overuse. Of all fluids, 33% were given to cases of diarrhoea and 21% to cases of respiratory infections. Unfortunately, oral rehydration corners were not available in the emergency units, which could have been very useful to decrease the need for intravenous fluids in mild cases [12–14].
Oxygen was given to 30% of cases. Previous studies have shown that oxygen can be used in as low as 16% concentration. In our sites, where oxygen is used without proper laboratory monitoring or other means of control such as transcutaneous monitoring, it may be safer and more economical to use air for resuscitation as an alternative which has been shown to be as effective as oxygen [15].
The socioeconomic parameters of parents, i.e. manual occupations, low level of education and khat-chewing and smoking habits, all constitute additional factors which add to the inability of the family to cope with emergency situations. Poverty, in addition to maldistribution of the family budget, further exacerbates the problem of coping with emergency situations [1].
The outcome of the paediatric emergency services care could not be evaluated properly. The significance of information on the outcome can neither be accurate nor representative of the community being studied, essentially due to a selection bias on the one hand and to inability to carry out proper follow-up. The mortality rate was 1.9%. The most important causes of death reported in this study were cardiac and respiratory failure.
The language of medical records is English for hospitals and Arabic at IMCI centres. At IMCI centres, records are structured and unified, whereas those of the hospital are in the form of a register which is not structured or unified. However, paediatric emergency services cases cannot be traced due to the fact that all emergency cases are referred and no records can be traced for the referral and or the feedback process. The referral system is generally very weak at all levels of the health service. The process of referral is affected by the difference in management between primary care services, practising according to guidelines, and higher levels, operating according to individual opinions [7] [Ishak A. Evaluation of IMCI in Yemen. Unpublished report to UNICEF, March 2005].
Although almost all emergency situations at primary care level are referred to higher levels, there are many situations where referral is impossible. Furthermore, cases such as burns, scalds, bleeding and injuries, which need at least first-aid care, are not included in the IMCI guidelines. Simoes et al. have shown from a study on the management of severely ill children at first-level health facilities in sub-Saharan Africa that there are also situations where referral is difficult or impossible, but the health worker can mange if he/she and the centre are prepared to do so [16].
There is probably a significant shortage of reference sources in the country for paediatric emergency services care, such as poisoning information, patterns of resistance to antibiotics, medicolegal advice, social support, scientific and educational data, etc., all of which add further dimensions to the complex issue of safety and efficiency of paediatric emergency services [17,18].
The lessons learned from this experience with regard to the development of a manual for paediatric emergency services are as follows:
Information systems for paediatric emergency services at primary and secondary levels of service need to be developed so that the clinical guidelines at both levels can be periodically evaluated.
All available information and experiences should be combined to create the proposed unified guidelines.
There is a real need for alternative means of laboratory support, such as a scoring system for evaluation, and for alternative means of therapy based on evidence from the financial, technical and safety points of view, e.g. the use oral rehydration solution instead of intravenous fluids even in moderately severe cases, the use of air instead of oxygen for resuscitation, the use of clinical scores to differentiate bacterial from viral infections, the use of simple side laboratories to be operated by physicians.
Acknowledgements
This study was supported by the High Council for Mothers and Children and supported financially by UNICEF (Sana’a Office). Thanks are due to the directors and colleagues at the research sites and at the Department of Child Health in the Ministry of Health.
References
- Government of Yemen, UNICEF, World Bank, Barnen R. Children and women in Yemen: a situation analysis: health and nutrition. Washington DC, UNICEF, 1999.
- The Yemen family health survey, 2003. Sana’a, Yemen, Ministry of Public Health and Population and Central Statistical Organization, 2003.
- Stidham GL. Emergencies in international child health. Current opinion in pediatrics, 1977, 9(3):254–8.
- Sarnaik AP, Daphtary K, Sarnaik AA. Ethical issues in pediatric intensive care in developing countries: combining western technology and eastern wisdom. Indian journal of pediatrics, 2005, 72:339–42.
- Duke T et al. Improving the quality of paediatric care in peripheral hospitals in developing countries. Archives of disease in childhood, 2003, 88:563–5.
- Integrated management of childhood illness. Geneva, World Health Organization, 2001 (WHO/FCH/CAH/00.40/2001).
- Al-Motarreb A, Baker K, Broadley KJ. Khat: pharmacological and medical aspects and its social use in Yemen. Phytotherapy research, 2002, 16(5):403–13.
- Singhi S, Singhi S, Gupta G. Comparison of pediatric emergency patients in a tertiary care hospital vs a community hospital. Indian pediatrics, 2004, 41:67–72.
- Archibald LK, Reller LB. Clinical microbiology in emerging countries. Emerging infectious diseases, 2001, 7(2):302–5.
- Gaur AH, Hare ME, Shorr RI. Provider and practice characteristics associated with antibiotic use in children with presumed viral respiratory tract infections. Pediatrics, 2005, 115(3):635–41.
- Gove S et al. Development and technical basis of simplified guidelines for emergency triage assessment and treatment in developing countries. WHO Integrated Management of Childhood Illness (IMCI) Referral Care Project. Archives of disease in childhood, 1999, 81:473–7.
- Tamburlini G et al. Evaluation of guidelines for emergency triage assessment and treatment in developing countries. Archives of disease in childhood, 1999, 81(6):478–82.
- Dalby-Payne J, Elliot E. Gastroenteritis in children. Clinical evidence, 2004, Dec(12):443–54.
- Saugstad OD, Rootwelt T, Aalen O. Resuscitation of asphyxiated newborn infants with room air or oxygen: an international controlled trial, the Respair 2 study. Pediatrics, 1998, 102(1):e1–7.
- Razzak JA, Kellermann AL. Emergency medical care in developing countries: is it worthwhile. Bulletin of the World Health Organization, 2002, 80(11):900–5.
- Simoes EAF et al. Management of severely ill children at first level health facilities in the sub-Saharan Africa when referral is difficult. Bulletin of the World Health Organization, 2003, 81(7):522–31.
- Nolan T et al. Quality of hospital care for seriously ill children in less-developed countries. Lancet, 2001, 357:106–10.
- Robertson MA, Molyneux E M. Triage in the developing world—can it be done? Archives of disease in childhood, 2001, 85:208–13.


