S.M. Elkhalifa,1 I.O. Mustafan,1 M. Wais2 and E.M. Malik3
مكافحة الملاريا في منطقة حضرية: قصة نجاح من الخرطوم، 1995 - 2004
صلاح الدين مبارك الخليفة، إبراهيم عثمان مصطفى، محمود وايس، الفاتح محمد مالك
الخلاصـة: الخرطوم منطقة حضرية ينخفض فيها انتقال الملاريا. وقد نجحت جهود المكافحة المبكرة في خفض معدلات الاختطار، إلا أن الملاريا أخذت تعاود الظهور في السنوات الأخيرة. وفي عام 2002، شرعت الحكومة السودانية، بدعم من منظمة الصحة العالمية، في تنفيذ مبادرة تهدف إلى جعل الخرطوم خالية من الملاريا. وركَّزت استـراتيجية الوقاية في هذه المبادرة على التدخلات المرتبطة بمكافحة اليرقات. وتدلُّ النتائج على حدوث انخفاض كبير في معدلات انتشار الملاريا، وفي الحالات المؤكَّدة والمشخصة سريرياً بين المرضى الخارجيـين المراجعين، وكذلك في أعداد الوفيات المرتبطة بالملاريا. ويقتـرح الباحثون جمع معلومات حول معدلات التساوي، وأن يتم إخضاع عينة جزئية من الناموس البالغ الذي يتم جمعه، لإجراء مقايسة الممتـز المناعي المرتبط بالإنـزيم (إليزا) أو إجراء التفاعل السلسلي للبوليميراز PCR لكشف عدوى الناموس بطفيلي الملاريا في المناطق التي تظهر فيها بؤر نشطة.
ABSTRACT: Khartoum is an urban area with low malaria transmission. Early control efforts were successful in reducing the risk but malaria has resurged in recent years. In 2002, the Government of Sudan, with support of the World Health Organization, embarked on an initiative aimed at freeing Khartoum of malaria. The initiative’s prevention strategy has focused on larval control interventions. The results indicate a significant reduction in malaria prevalence, confirmed and clinically diagnosed malaria cases among outpatient attendance and the number of malaria-associated deaths. It is proposed information be collected on parity rates and that a sub-sample of the adult mosquito collections be subjected to ELISA or PCR for identification of malaria parasite infections in mosquitoes in areas showing active foci.
La lutte antipaludique en milieu urbain : histoire d'un succès à Khartoum, 1995-2004
RÉSUMÉ: Khartoum est une zone urbaine à faible transmission palustre. Les actions entreprises dans le cadre de la lutte antipaludique sont parvenues dans un premier temps à réduire le risque, mais on assiste ces dernières années à la résurgence du paludisme. En 2002, le gouvernement soudanais, avec l’appui de l’Organisation mondiale de la Santé, s’est lancé dans une initiative visant à débarrasser Khartoum du paludisme. Celle‑ci reposait sur une stratégie préventive axée sur des opérations larvicides. Les résultats font apparaître une diminution significative de la prévalence du paludisme, des cas cliniquement diagnostiqués et confirmés parmi les patients vus en consultation externe et de la mortalité palustre. Les auteurs proposent de collecter des données sur le taux de parturité des femelles et de soumettre un sous‑échantillon des collections d’anophèles adultes à un test ELISA ou à la PCR pour identification des infections des anophèles par les différentes espèces plasmodiales dans les zones abritant des foyers actifs..
1State Malaria Control Programme, Khartoum State, Khartoum, Sudan.
2Roll Back Malaria, World Health Organization, Khartoum, Sudan.
3Directorate of Malaria and Leishmaniasis Control, Khartoum, Sudan (Correspondence to E.M. Malik:
Received: 24/08/05; accepted: 08/12/05
EMHJ, 2008, 14(1): 206-215
Background
Malaria in Sudan continues to be a major public health problem. There are an estimated 7.5 million cases and 35 000 deaths every year [1]. In the countries of the Eastern Mediterranean Region of the World Health Organization (WHO/EMR), these figures represent 70% and 50% of the Region’s cases and deaths respectively [2]. Sudan has been stratified into 5 operational strata: riverine, seasonal, urban, irrigated and high perennial transmission areas [3]. Plasmodium falciparum is the predominant species, accounting for more than 95% of all malaria cases, with Anopheles arabiensis, An. gambiae and An. funestus as the main disease vectors.
Khartoum State lies between latitude 15° 10′–16° 30′ N and 31° 40′–34° 20′ E in the central part of Sudan. The total area of the state is 28 000 km2. The state has a dry winter from November to March, a dry hot summer from April to July and patchy rains from August to October. The Blue and White Nile rivers separate the state into 3 major areas: Khartoum, Bahry and Omdurman. There is a dam 40 km south of Khartoum city on the White Nile and there are small irrigation schemes and farms concentrated mainly in Bahry area. The total population of the state is approximately 5 548 418 [4]. Due to a daily influx from other states, however, the population of the state shows a steady increase, with about 1000 individuals added to the state population every day. The majority of the population are a mixture of tribes from various malaria-endemic areas in Sudan. The main occupation is government or private employment. According to the above-mentioned operational and epidemiological stratification, Khartoum is considered as urban with low malaria transmission [1]. Recent studies in Khartoum State [5] have confirmed the leading role of P. falciparum. The increasing importance of P. ovale and P. vivax has also been demonstrated. An. arabiensis is the only vector in this area (personal communication: Elfadul Obied, PhD student).
This paper aims to shed some light on the ongoing work in malaria control in Khartoum State, the achievements and recommendations for the future. This involved the systematic review of published and unpublished data. Annual statistical reports and the state malaria control reports, in addition to entomological and parasitological survey reports during 1995–2004, were reviewed intensively.
Programme rationale
Attempts to control malaria in Khartoum started early in the last century. The first organized control programme was initiated in 1904. With the use of retained oil and other simple vector control interventions, the programme succeeded in eradicating malaria from the area [6]. The disease incidence was kept at a very low level up to the 1970s but malaria resurged again from the 1970s to the 1980s due to the deterioration of the control programme and the influx of internally displaced people from high- as well as low-endemic areas. During late 1980s and early 1990s, malaria in Khartoum was the leading cause of outpatient attendances, hospital admissions and deaths in all health facilities. In addition to malaria, nuisance-biting from nonmalaria mosquitoes was a problem. This led in 2002 to the launch of the Khartoum malaria-free initiative. The main goal of the initiative was to ensure that malaria will no longer be a major public health problem in the programme operation areas.
Main programme activities
Multiple interventions targeting mainly the larval stages of An. arabiensis have been in place since 1995. Importance was also placed on case management.
Vector control
In an urban setting such as Khartoum, where mosquito-breeding sites can be identified, prevention strategies based on vector control, with the emphasis on environmental management, can be a central feature of the malaria control programme [7]. The activities adopted by the initiative included the mapping and identification of all breeding sites, treatment of breeding sites, intermittent irrigation, rehabilitation and immediate repair of leaking water pipes and land modification where applicable. The core intervention for the Khartoum malaria control programme was larval control through weekly application of temephos and environmental management. The programme divides Khartoum into working areas following the administrative structure. Geographical reconnaissance for each division was updated every year in order to facilitate the programme implementation. In 2002 WHO supported the programme by assigning experts from the Oman malaria control/eradication programme to develop well-constructed maps allowing for the different interventions. Each public health officer was supported by sanitary overseers and support workers (“mosquito men”) equipped with necessary supplies and equipment.
Malaria case management
Case management, a known effective strategy for malaria control, was given particular attention by the programme [8,9]. Many activities to improve malaria microscopy were carried out; these included supervision and training of staff, provision of consumables and replacement or repair of microscopes where this was necessary. Low sensitivity and specificity is still a feature of microscopy testing as reported in a previous study [10]. Medical staff turnover, the wide relatively uncontrolled private medical sector, medical doctors’ under-reliance on laboratory results and the extent of work needed all contribute to the problems associated with diagnosis of cases. Antimalarial drugs are provided through the revolving drugs fund (developed with assistance from Save the Children, United Kingdom) with a price below 40% of the market price.
Monitoring and evaluation
The programme plan was based on routine surveillance data supported by surveys. This provided data on a weekly, monthly and annual basis that was used to direct the programme activities.
Vector surveillance
A weekly system of vector surveillance was established in the early stages of the programme. Mosquito larvae and adults were collected weekly from 8 stations. The number of sentinel sites increased to a total of 24 stations in 2002 and, following administrative changes in the state, the collection frequency was changed to once every 2 weeks. A trained team composed of a public health officer, 5 technicians and 5 support workers collected the data. The teams were trained in methods of collection and identification of larvae and adults. A senior entomologist compiled the data and reported to the state malaria control programme which supervised the team.
Larval surveys
All known permanent breeding sites including temporal ones were sampled from each station parallel to those earmarked for adult mosquito collections. The team started with inspection of the breeding sites using a dipper (0.5 L); 3–10 dips were taken from each site to estimate the mosquito larvae densities, i.e. the average number of mosquito larvae per dip. The team then classified the larvae according to stage and to species identification and provided a full report using the form recommended by the national malaria control programme.
Adult mosquito surveys
Using the pyrethrum sheet collection method, the team collected indoor resting mosquitoes from 7 rooms in each sentinel site on each and every survey. Collections were usually carried out between 06:00–08:00 hours. Collected mosquitoes were then classified as fed/unfed and parous/nulliparous, based on the physiological and gono-trophic status and identified by species based on morphological features. The average number of Anopheles per room per station was the main entomological indicator for adult mosquitoes.
Parasite surveys
With the assistance of an epidemiologist, a system for an annual cross-sectional parasitological survey during the malaria season (September) has been established since 1995. The sample size was calculated based on an expected prevalence of 10% in 1995. This was changed and the last (2004 survey) was calculated based on the 2003 prevalence (0.5%). The calculated sample size was then taken from all the administrative units. The number taken was proportional to the target population. Villages/blocks were selected randomly from a list for inclusion in the survey. In each selected village/block, all households were surveyed and from each household 5 persons (including at least 1 child under the age of 5 years) were selected randomly. A team of 20 trained laboratory personnel divided into 4 groups collected the blood samples from the field. Another 8 experienced laboratory technicians stained and read the slides collected. The thick and thin blood film slides collected were stained with 5% Giemsa stain for 30 minutes and 100 fields were examined at 10 × 100 magnification by experienced microscopists for the presence of identified trophozoites and gametocytes. Estimation of the parasite density was done by counting the number of asexual stages associated with 200 white blood cells. A team of 4 senior technicians rechecked 10% of the slides collected.
Reported incidence
Reports showing malaria incidence, admissions and deaths (in addition to the slide positivity rates) received regularly on a weekly basis at sentinel stations and on a monthly basis at all health facilities were used to measure the impact of the interventions. The number of sentinel stations increased from 36 in 1995 to 75 in 2000 and to 150 sites by the beginning of 2003. The monthly reporting rate from all health facilities increased from less than 50% to over 90% because of the work done to improve the routine health information system.
Partners involved
Late in the 1980s, with assistance from the Japanese, an intensified programme was established in Khartoum State. The ongoing programme, however, started with local resources in 1995. Efforts to involve more partners were initiated and in May 2002, the State and Federal Ministry of Health, in collaboration with WHO, initiated the Khartoum and Gezira malaria-free initiatives. Different collaborators (such as WHO and the water corporation) were part of this work from the planning stage. With time, the programme assigned more and more activities to other sectors, namely the agriculture and water authorities.
In Khartoum, irrigated urban agriculture influences the transmission of malaria considerably, as seen in other parts of Africa (Table 1) [11]. The activities aiming to reduce the breeding sites in agricultural schemes and small farms were carried out in close collaboration with the Ministry of Agriculture in the state. This collaboration led to more than 80% compliance with the weekly intermittent irrigation activities.
Broken drinking-water pipes were also identified as the important breeding sites and were tackled by joint teams comprising the malaria and the water authority staff that was established in 2001 in all districts with activities including quick repair and treatment of the remaining water. By this system, more than 9000 broken pipes were repaired in the first year before they were able to create breeding sites (personal communication). Senior staff from the national malaria control programme and the district level conducted supervision on a regular basis to ensure the required quality.
The contribution of the Ministry of Education was also important. The malaria control programme arranged with the Ministry of Education a competition between schools that acted as an advocacy tool for the initiative. The press and other media also participated through a council initiated for this purpose.
Programme achievements
Breeding sites, larval and adult densities
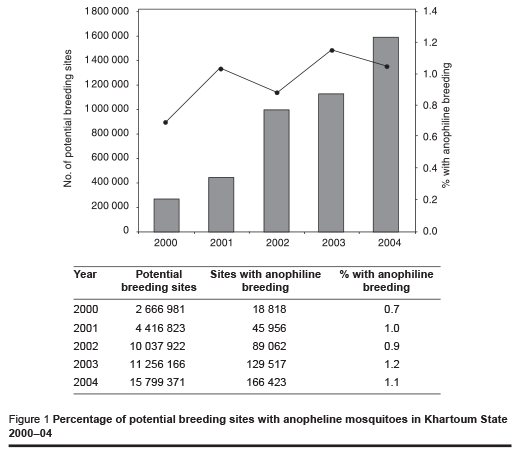
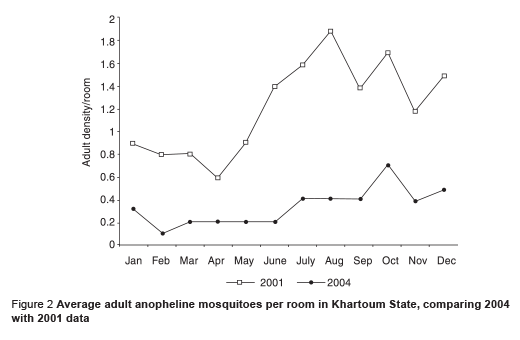
The percentage of sites with anopheline larvae detected did not change greatly between 2001 and 2004 (Figure 1), although the number of breeding sites detected greatly increased. The main sources of anopheline breeding in the state were irrigation sites and small farms, broken waterpipes, indoor sites, new construction basins and institutions (e.g. schools, mosques, public gardens). As shown in Table 1, the number of potential breeding sites inspected increased over the same period. With the exception of irrigated areas, the contribution of different sites for anopheline breeding declined significantly. Data colleted from sentinel sites for vector surveillance revealed a lower density of adult anopheline mosquitoes per room in all months of the year in 2004 compared with 2001 (Figure 2) but the larval density (a range of 6–8 per dip) did not show any difference.
Prevalence
A series of parasite surveys were carried out during the malaria season in September every year during the period between 1995 and 2004. The sample size varied from year to year. The highest slide positive rate was reported in 1998 (5.12%) and the lowest in 2004 (0.05%) (Table 2). P. falciparum was the predominant species, constituting about 99% of the malaria parasites. Positive slides were reported in the age group 5 years and above during 2000 and 2001 (P 0.05). The male:female ratio was 1:1 during the period. Comparison of the survey results of 2003 and 2004 yielded a significant reduction (P < 0.005) of the slide positivity rate (data not shown).
Reported incidence
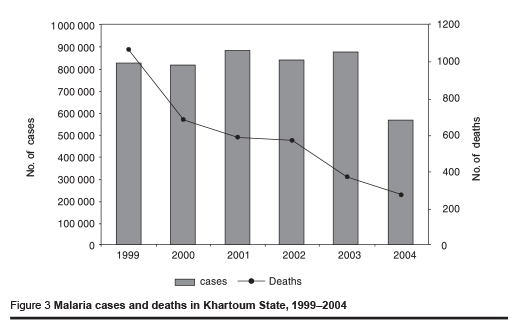
The data collected from the different sentinel sites showed a decline in the number of malaria cases and deaths (Figure 3). Malaria cases, as a proportion of total outpatient attendances, also declined from 40% in the 1990s to less than 20% in 2004. Malaria deaths were markedly reduced from 1070 in 1999 to 274 in 2004, representing an almost 75% reduction.
Overall picture
As reported in the current study, the proportion of malaria cases out of the total outpatient attendances was greatly reduced. Malaria prevalence among the Khartoum State population was also reduced from over 5% in the early 1990s to < 1% by 2004. With this level of malaria prevalence, the interventions were able to reduce the malaria endemicity from meso- to hypoendemic [1]. This reduction was accomplished due to the fact that health care providers managed malaria based on diagnosis and not only on clinical presentation.
Challenges, lessons learned and future perspectives
The current malaria control programme, which has been appreciated by the community, is based on sound interventions, partnerships, community involvement, commitment from staff and political leaders, and sustainability. These well-recognized and recommended tools for malaria control were interrelated, i.e. they had an enhancing effect on each other [8,9]. Sustainability, for instance, was maintained through obtaining the necessary supplies and equipment, staff satisfaction, regular supportive supervision, involvement of the community and productive partnerships. As stated by others [12], the programme built on existing health systems as a result of intersectoral coordination among urban planning, agriculture and other government sectors. This provided the programme with the opportunity to involve the community and the private sector.
In terms of monitoring and evaluation of the impact of the interventions, however, there is room for improvement, especially in monitoring of the entomological indicators. Currently the Khartoum control programme relies on collecting monthly data on mosquito density indicators, i.e. average numbers of mosquito larvae/dip and numbers of adult mosquitoes per room. As none of these indicators are useful in measuring transmission, it is recommended that in addition to the 2 mosquito density indicators, the programme should also concentrate on collecting information on parity rates (an indication of the age structure of the mosquito population) through dissection. Where the parity rate is high, it is an indication that transmission is ongoing and vice versa. Moreover, a sub-sample of the adult mosquito collection, particularly from active foci of infection, should be subject to enzyme-linked immunosorbent assay or polymerase chain reaction testing for identification of the malaria parasite infections in mosquitoes. These results and the information on the adult densities could provide the entomological inoculation rates which the programme can use to measure the impact of the interventions reliably [13,14].
The experience of Khartoum State, like other experiences worldwide [7,15,16], has shown how effective an integrated approach to malaria control can be, where social stability, widespread health education and strong programme administration exist. The programme also succeeded in mobilizing local resources and related sectors for malaria control and this must be encouraged and reinforced through training of local staff, continuous evaluation of local models by national health authorities, and the designation of local leaders based on ability rather than personal or political relations [15,17]. Long-term solutions to ensure sustaina-bility of these control measures and to work towards the slogan raised in 2002 “Towards Khartoum malaria-free zone”, may necessitate proper urban planning, reinforcing the drainage and sanitary facilities and improving the performance of the health services, including malaria microscopy [18].
Acknowledgements
We would like to acknowledge the staff working for Khartoum Malaria Free Initiative who are doing their best to sustain the ongoing malaria control measures. We appreciate the technical and financial support from WHO.
References
- Malik EM et al. Stratification of Khartoum urban area by the risk of malaria transmission. Eastern Mediterranean health journal, 2003, 9(4):559–69.
- Roll Back Malaria in the WHO Eastern Mediterranean Region. Cairo, World Health Organization Regional Office for the Eastern Mediterranean, 2002 (WHOEM/ MAL/273/E/G/12.01/3000).
- Malik EM, Khalafalla OM. Malaria in Sudan: past, present and the future. Gazira journal of health sciences, 2004, 1(Suppl.):47–51.
- CBS year book (Population data sheet for Sudan by states). Khartoum, Sudan, Central Bureau of Statistics and United Nations Population Fund, 2003.
- El Sayed BB et al. A study of the urban malaria transmission problem in Sudan. Acta tropica, 2000, 25, 75(2):163–71.
- Balfour A, ed. First report of the Wellcome Tropical Research Laboratories at the Gordon Memorial College, Khartoum. Khartoum, Department of Education, Sudan Government, 1904.
- Castro MC et al. Integrated urban malaria control: a case study in Dar Es Salaam, Tanzania. American journal of tropical medicine and hygiene, 2004, 71(Suppl. 2):103–17.
- Implementation of the global malaria control strategy. Report of a WHO study group on the implementation of the global plan of action for malaria control 1993–2000. Geneva, World Health Organization, 1993 (WHO Technical Report Series, No. 839).
- Malaria control today. Current WHO recommendations. Geneva, World Health Organization, Roll Back Malaria Department, 2005.
- Ibrahim SM. Decisive assessment of diagnostic staining methods of malaria in eight public and private laboratories, Khartoum area. In: Operational research in tropical diseases, final report summaries 1992–2000. Cairo, World Health Organization Regional Office for the Eastern Mediterranean, 2003 (WHOEM/ TDR/004/E/G).
- Afrane YA et al. Does irrigated urban agriculture influence the transmission of malaria in the city of Kumasi, Ghana? Acta tropica, 2004, 89:25–34.
- Donnelly MJ et al. Malaria and urbanization in sub-Saharan Africa. Malaria journal, 2005, 4(1):12.
- Gilles HM. Epidemiology of malaria, quantitative epidemilogy of malaria. In: Gilles HM, Warrell DA, eds. Bruce-Chwatt’s essential malariology, 3rd ed. London, Edward Arnold, 1993.
- Vector control for malaria and other mosquito-borne diseases. Geneva, World Health Organization, 1995 (WHO Technical Report Series, No. 857).
- Garfield R. Malaria control in Nicaragua: social and political influences on disease transmission and control activities. Lancet, 1999, 354:414–8.
- Hunq le Q et al. Control of malaria: a successful experience from Viet Nam. Bulletin of the World Health Organization, 2002, 80(8):660–6.
- Utzinger J, Tozan Y, Singer BH. Efficacy and cost–effectiveness of environmental management for malaria control. Tropical medicine and international health, 2001, 6(9):677–87.
- Kazadi W et al. Malaria in primary school children and infant in Kinshasa, Democratic Republic of the Congo: surveys from 1980s and 2000. American journal of tropical medicine and hygiene, 2004, 71 (Suppl. 2):97–102.


