Adibul Hassan Rizvi1
1Director, Sindh Institute of Urology and Transplantation, Karachi, Pakistan (Correspondence to Adibul Hassan Rizvi:
EMHJ, 2006, 12(Supplement 1): 6-9
I would like to welcome Professor Pirzada Qasim, the Vice-Chancellor of Karachi University, and all the delegates and thank you all for participating in this conference Fundamentals of Research Ethics – International and Regional Perspectives. I am especially grateful to the foreign participants, who came despite discouragement by their governments. I am confident that you will appreciate how peaceful Pakistan is and that you will not hesitate to come again.
I appreciate all the support provided by Karachi University and Professor Pirzada Qasim in developing the Institute of Urology and Transplantation (SIUT) by initiating the postgraduate programme for a Masters degree in surgery. The Institute has the honour to produce the first such Masters in the country. The MD in nephrology and the PhD and MPhil in basic sciences have followed this. All these programmes are on-going. Another unique development is the addition of Bachelors degrees in medical technology, laboratory medicine, theatre technology, intensive care and dialysis. Young men and women, who are bright but could not gain admission in medical institutions due to having slightly lower grades, have joined these courses. Credit goes to Karachi University for starting this programme by providing financial assistance.
After the establishment of the Centre of Biomedical Ethics and Culture (CBEC), the International Centre for Bioethics will be formed which will be affiliated with Karachi University. The Centre is the first such centre in the country, and the regional centre, the Institute of Biotechnology, in Karachi University will be the first of its kind catering to the needs of the region. The World Health Organization is expected to help with this programme. A postgraduate diploma programme will soon be started and the Masters in bioethics will follow.
Surgeons always try to abide with ethics, but they tend not to be keen researchers. Ethicists are the real custodians of research and its safety, and are responsible for safeguarding the interests of the common man in research. Research is for the benefit of mankind and the good results should be made accessible to everybody in this world. Both these factors make research meaningful. Ethics is an important component of research and without ethics, research will end in disasters such as Hiroshima and Nagasaki. Without ethics, research will produce biological warfare instead of antibiotics. The whole world is gripped by the fear of bioterrorists. The United States of America spends about 9.5 billion US dollars against bioterrorism because research is being carried out without ethical control. It is quite possible that the wars being fought today are out of fear.
It is known that 80% of the people do not benefit from research results. For example, people are still dying of malaria and tuberculosis, more so in the developing countries, although the treatment is available. About 25 000 000 people have succumbed to AIDS, approximately 49 000 000 are suffering from this disease and 14 000 are dying or contracting AIDS every day in the African countries. It is also evident that 91% of them do not have access to treatment although treatment is available. The question arises, “Where does the problem lie?”
It is known that the best research, because its aplication is not controlled by ethics, is easily hijacked by multinationals, which can do so because they have the money. The poor continue to suffer as they will never be able to afford the drugs that have been tried out on them and given good results. This poverty gap is widening day by day and even a person with an average or modest income will not be able to buy the research products. Ethically, research becomes meaningless if the majority of the people cannot have access to its results.
The economic disparity is evident in the developing world where health is a complex issue. It is not just treating a disease by dispensing medicines or providing surgical services. It includes disease prevention, health education and a healthy environment, both physical and social. It includes access to safe water and good nutrition. The question is, “Why can’t people living in developing countries buy healthy food and be offered standard health facilities?” This question can be answered after analysing the differences between the developed and developing countries.
Historically, many countries were colonized by the richer countries. They are economically deprived and have poverty as a dominant feature. The British medical journal in 1999 drew attention to the economic disparity between developed and developing countries in the shape of a champagne glass [1]. The world was divided into two regions on the basis of economic and technological inequalities. Economically the developing countries own only 25% of the total wealth, whereas they are inhabited by 80% of the world population. It has also been shown that the assets of the top three billionaires of the world are more than the combined Gross National Product of all the least developed countries inhabited by 600 000 000 people.
The impact of poverty can be seen in the health budget of a developing country. An example is the health budget of Pakistan where only 3.4% is allocated for the health sector. This scenario is similar in most developing nations and the result of this meager allocation towards health is seen as the pathology of poverty depicted in deaths caused by acute infectious diseases. Malaria alone kills 3000 people daily or more than 1 000 000 each year. Diarrhoeal diseases claim roughly 2 200 000 lives annually. Almost 2 000 000 of the victims are small children and virtually all from developing nations. Tuberculosis kills 1 700 000 people a year, mostly in Africa and South-East Asia. Acute respiratory infections are responsible for killing 4 000 000 people annually with a disproportionate number belonging to the world’s poorest nations. Measles claims 900 000 lives a year in developing countries and HIV/AIDS affects 3 000 000 people annually. Hepatitis B and C afflict 400 000 000 people, 30% of whom end up with end-stage liver disease.
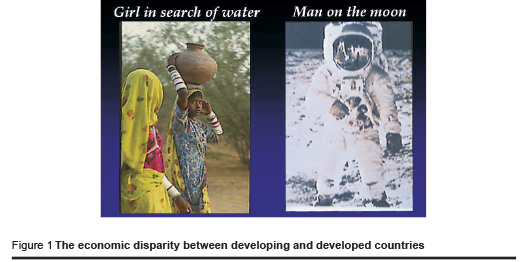
In reality, the difference is apparent when the landing of man on the moon is compared to a village girl walking with a pitcher on her head in search of drinking water (Figure 1). This large discrepancy is factual, but it is also accepted that health is a birth right for every individual. We need to consider who will bear the cost of treatment, the patient or the government of a developing country.
If the situation in a developing country is analysed, it is evident that the priorities of the government on spending are unrealistic and with poor governance. Investment is directed to the maximum towards debt servicing followed by defence services. The health sector is the worst sufferer with the least funds, making it impossible for people of a low economic status to obtain good health care. It is not possible for a person living below the poverty line with earnings of less than 1 US dollar a day to think about medical treatment, because he/she does not know where the next meal will come from. In this situation, medical care is a luxury.
Rational thinking provides a solution to this problem. Neither the government alone nor the individual patient can shoulder this responsibility. This is a big challenge for every medical institution and SIUT took a bold step to find a way forward. It has been proved by SIUT that a government and community partnership can be successfully employed in a government-sector hospital where the patient is the beneficiary and receives standard treatment without any charges being levied. This requires sufficient autonomy of functioning with transparency to gain community confidence.
The philosophy of SIUT is based on this triad of community, government and doctors, with doctors playing the role of catalyst. Here limited government grants are supplemented largely by public donations for providing free treatment facilities to all patients.
The achievements of SIUT are many. SIUT had a humble beginning as an eight-bed urology ward in 1972. It has grown in response to the needs of the people. Patients come for treatment from all over the country and the neighbouring regions of Afghanistan and expatriates from Middle Eastern countries. The number of patients has grown from 120 000 in 1997 to 404 000 in 2005. All services are free and include 27 outpatient clinics and inpatient facilities for nephrology, urology, transplantation intensive care unit, medical intensive care unit, critical care unit, paediatric unit, gastrointestinal and liver unit and day care ward. The number of patients in these units has increased from 6991 in 2000 to 13 957 in 2005.
The very busy dialysis department has 130 units performing 350 dialysis sessions per day. Renal transplantation is a routine procedure and 130 transplants are carried out annually. Other surgeries take place in the 14 operation theatres which are all very well equipped. The high prevalence of stone disease in the region has called for non-invasive techniques of stone removal at SIUT. There are four modern lithotriptors performing on 12 patients daily. Also available are laser technology and lithoclast to remove urinary tract stones.
SIUT has invested in technology. The centre for molecular medicine performs all sophisticated tests including serology, virology and antigen detection by polymerase chain reaction. A reference laboratory provides all required services round the clock with 2 million tests done in 2005. Facilities for radiology, computed tomography, magnetic resonance imaging, angiography, and colour Doppler are all available at the Institute.
Children receive priority services in the paediatric urology, nephrology, hepatology and oncology units. Paediatric renal transplantation is an important section of the transplant activities in SIUT.
Kidney recipients are provided regular follow-up services, laboratory tests and immunosuppressive drugs at regular intervals. Similarly kidney donors are offered free annual check-ups and laboratory investigations through a donor follow-up weekly clinic. Rehabilitation advice and facilities are provided through the medical social officers.
Another important achievement of SIUT is the establishment of a school for medical technologists. It offers a three-year course for a Bachelor degree in medical technology.
The future plans include an institute for transplant sciences and biotechnology located at Kathore.
References
1. The champagne glass of world poverty. British medical journal, 1999, 318 (Editor’s choice).


