M. Asefzadeh1 and B. Peyrovian2
ABSTRACT We studied measles incidence and morbidity in Ghazvin district by retrospective review of cases registered at the central health office and admitted to two hospital in Ghazvin city during April 1997–April 2003. There were 824 clinically confirmed cases of measles over the 6-year period giving a mean annual incidence of 18.67 per 100 000 population, higher than for the country generally. There were no deaths from measles. Of the 824 cases, 591 (71.1%) had serum specimens for serological analysis and 199 (24.3%) were confirmed serologically. Of the serologically confirmed cases, the grea-test proportion (44.2%) were over 20 years (median age was 17.5 years), 54.5% had been in contact with a measles case and 21.6% cases had received 2 doses of vaccine. We studied 33 serologically confirmed hospitalized cases. Common complications were vomiting (45.5%), diarrhoea (42.4%) and pneumonia (21.2%). The mean duration of hospitalization was 3.8 days.
Étude épidémiologique de la rougeole à Ghazvin (République islamique d’Iran), avril 1997-avril 2003
RÉSUMÉ Nous avons étudié l’incidence de la rougeole et la morbidité due à cette maladie dans le district de Ghazvin en procédant à un examen rétrospectif des cas enregistrés au bureau central de la santé et admis dans deux hôpitaux de la ville de Ghazvin entre avril 1997 et avril 2003. On a dénombré 824 cas de rougeole confirmés cliniquement au cours de cette période de 6 ans, soit une incidence annuelle moyenne de 18,67 pour 100 000 habitants, ce qui est plus élevé que pour le pays en général. Il n’y a eu aucun décès dû à la rougeole. Sur les 824 cas, 591 (71,1 %) ont subi des prélèvements d’échantillons de sérum pour analyse sérologique et 199 (24,3 %) ont eu une confirmation sérologique. Parmi les cas sérologiquement confirmés, la plus forte proportion (44,2 %) étaient âgés de plus de 20 ans (l’âge médian était de 17,5 ans), 54,5 % avaient eu un contact avec un cas de rougeole et 21,6 % des cas avaient reçu deux doses de vaccin. Nous avons étudié 33 cas hospitalisés ayant une confirmation sérologique. Les vomissements (45,5 %), la diarrhée (42,4 %) et la pneumonie (21,2 %) étaient les complications courantes. La durée moyenne d’hospitalisation était de 3,8 jours.
1Boalisina Hospital of Ghazvin City, 2Ghazvin Medical University of Iran, Ghazvin, Islamic Republic of Iran (Correspondence to B. Peyrovian:
Received: 27/01/05; accepted: 09/08/05
EMHJ, 2006, 12(1-2): 14-22
Introduction
Although measles is a preventable disease, it is still a major health problem in developing countries. Because of the complications of measles infection, it remains the fifth leading cause of death in children under 5 years in the world [1]. In 1997, the 23 member countries of the World Health Organization (WHO) Eastern Mediterranean Region resolved to eliminate measles from the region by 2010 [2]. In the Islamic Republic of Iran, as a part of the Eastern Mediterranean Region of the WHO, measles vaccination was begun in 1980 with 2 doses of live vaccine, one dose given at the end of the ninth month of birth and other in the fifteenth month. This schedule was followed until 2004. After that time the measles vaccination schedule was changed to 1 dose of the MMR (mumps–measles–rubella) vaccine given at the end of the twelfth month of birth and another dose given at 5 years.
In view of the fact that statistical research forms the base of executive planning to achieve measles elimination by 2010, we studied measles epidemiological indexes in Ghazvin city and its territories (as a pilot model) from April 1997 to April 2003 and compared our data with those for the Islamic Republic of Iran as a whole for the same time. We also studied measles morbidity in hospitalized patients in the district to investigate the complication of measles.
Methods
Ghazvin district includes Ghazvin city and 8 towns with a few surrounding villages. The estimated population of the district is 700 000 according to the records of the Shahid Bolandian Health Centre. All clinically confirmed measles cases diagnosed by physicians from all governmental health centres in the area and also private clinics and governmental and nongovernmental hospitals in this region are required to be reported to Shahid Bolandian Health Centre as a central office.
This study was conducted retrospectively to determine measles epidemiological indexes by review of patient’s files that were registered at the Shahid Bolandian Health Centre over the period April 1997 to April 2003. Their related data, including demographic data, vaccination status, date of illness, signs and symptoms (fever, typical rashes, conjunctivitis, cough and coryza), contact history and serological results are recorded on standard paper forms in the central health centre. These forms are completed by general practitioners but in some cases data were missing. Serum specimens of cases are referred to the virology section of the Tehran Medical University for Laboratory Studies. Measles is diagnosed if there is a 4-fold increase in measles IgG antibodies in 2 serum specimens, 1 at the time of diagnosis and the other after 2 weeks (this was the criterion used before 1999), or there is a positive result in a single serum specimen obtained by IgM using an ELISA technique (this was the criterion used after 1999). In some cases, with an unclear serological result in the forms, we obtained the information directly from the virology section of Tehran University.
In order to study measles complications and morbidity, we also reviewed the medical records of 113 measles patients hospitalized in Boalisina and Quds hospitals, which are government teaching hospitals in Ghazvin. The medical records of patients in the other 4 hospitals in the district were not available to us. The patients’ records included demographic data, vaccination status, contact history, signs and symptoms (fever, conjunctivitis, cough and Koplik spots), mean duration of signs and symptoms at the time of admission, complications, duration of hospitalization, and results of common laboratory tests such as urine analysis and complete blood count. Some patients had chest X-ray, erythrocyte sedimentation rate (ESR), liver function tests and stool examination depending on their signs and symptoms. We used the following definitions [3,4]: urinary complications as haematuria and dysuria with or without frequency; nervous complications as loss of consciousness, seizure or encephalitis; gastrointestinal complications as nausea and vomiting or diarrhoea or melena or abdominal pain; respiratory complications as pneumonia and its complications or laryngitis or otitis. High ESR was defined as > 20 mm/h in children, > 20 mm/h in females over 50 years and > 30 mm/h in females under 50 years, > 20 mm/h in males over 50 years and > 15 mm/h in males under 50 years. Pyuria was defined as white blood cells > 5–10 in high power field. Leukocytosis was defined as white blood cell count >10.8 × 109/L in adults and > 13.5 × 109/L in children 2–6 years old and > 15.5 × 109/L in children 6–12 years old. Leukopenia was defined as white blood cell count < 4.3 × 109/L in adults and < 4.5 × 109/L in paediatric patients. Abnormal liver function tests were defined as aspartate aminotransferase (AST) > 47 U/L and alanine aminotransferase (ALT) > 53 U/L.
Abnormal chest X-rays were identified by radiologists and registered in the patients’ charts.
Vaccination coverage for the previous 15 years and the mean population of this region were obtained from the statistics section of Shahid Bolandian Health Centre. Mean duration of hospitalization in the infectious disease section of Boalisina hospital was calculated from data recorded in the hospital.
Measles reported cases for all Islamic Republic of Iran and also the population of the country was obtained from WHO records and measles incidence was calculated according these figures for each year [5,6].
Data were analysed by SPSS, version 9.01 software.
Results
Incidence
During April 1997 to April 2003, 824 clinically diagnosed cases were reported to Shahid Bolandian Health Centre. Of these, 591 (71.7%) had serum specimens for laboratory analysis and 199 (24.15%) were confirmed serologically. The number of clinically confirmed cases with serum specimen and serologically confirmed cases and also hospitalized cases in the different years are shown in Figure 1.
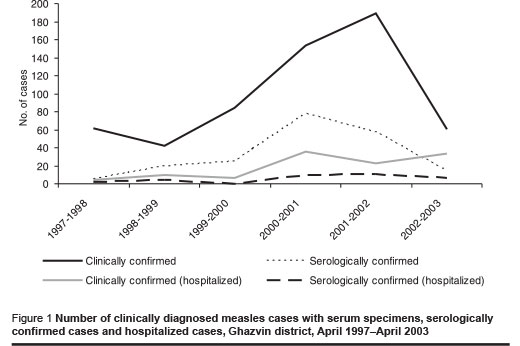
Incidence per 100 000 population in clinically confirmed cases was 10 in 1997–1998, 6 in 1998–1999, 13 in 1999–2000, 27 in 2000–2001, 32 in 2001–2002 and 24 in 2002–2003, giving an mean annual incidence of 18.67 per 100 000 population.
There were no deaths due to measles in Ghazvin district during this period.
Demographic data of the cases
Of 824 clinically confirmed cases, 356 (43.2%) were female and 468 were male giving a male to female ratio of 1.3:1.
Age was registered in 817 of the 824 clinically diagnosed measles cases. Of these, 32 (3.9%) were under 1 year, 28 (3.4%) were 1–4 years, 225 (27.5%) were 5–9 years, 184 (22.5%) were 10–14 years, 149 (18.2%) were 15–19 years and 201 (24.6%) were over 20 years. The mean age was 13.5 years.
In 706 patients residence was recorded on the forms; 496 (70.3%) of these cases lived in urban and 210 (29.7%) in rural areas.
Season of acquiring measles was recorded on 805 patient forms. Of these, 478 (59.4%) had measles in spring, 97 (12.0%) in summer, 28 (3.5%) in autumn and 202 (25.1%) in winter.
Of 807 cases for whom contact data were available, 418 (51.8%) had a positive history of contact with a measles case. The contact was a family member in 85% of cases, a fellow soldier in barracks in 12% and a schoolmate in 7% of cases.
Vaccination status
Of the 824 measles cases, 512 (62.1%) had a clearly documented history of vaccination and 312 (37.8%) had not and therefore their vaccination status was unknown. Of the 512, 419 (81.8%) had received 2 doses of vaccine, 38 (7.4%) had received 1 dose and 55 (10.7%) had not received any vaccination. Thus 89.2% had received at least 1 dose of vaccine. Of the serologically confirmed cases of measles, 14.2% had received 2 doses of vaccine and 32% had received 1 dose of vaccine (Table 1).
The characteristics of the serologically confirmed cases of measles are shown in Table 2.
Hospitalized patients
Of all diagnosed cases of measles, 181 (22.0%) were hospitalized; 113 of these patients were hospitalized in Boali Sina and Quds hospitals and their hospital records were available. Of these, 53 had serum specimens and 33 were confirmed serologically. The male to female ratio was 1:3.
Of the main signs and symptoms of measles recorded on first examination in patients in the 2 hospitals, fever was found in 99.1% of cases, rash in 97.33%, cough in 85.85%, conjunctivitis in 69.91% and Koplik signs in 26.6%.
The frequency of hospitalization was highest in April 2000 to April 2001 [31.9% of the 113 cases]. Hospitalization also occurred more frequently in spring (52.2%) and summer (23.9%).
Only 29 of 113 cases had a clear history of vaccination: 23 of these patients had received at least 1 dose of vaccine, while 6 of them had never been vaccinated. Most (59.3%) of the 113 patients were over 20 years of age; the fewest number of cases was in the 5–9-year-old age group. The mean age of the hospitalized patients was 20.5 years.
As regards complications, 61 (54.0%) of the 113 hospitalized patients had gastrointestinal complications, vomiting (42.4% of the patients) and diarrhoea (45.5%) being the commonest. Respiratory complications were found in 30.1% of cases, pneumonia in 17.7% of the patients and laryngitis in 12.4% being the commonest: 18 patients had both respiratory and gastrointestinal complications. Urinary and nervous system complications were found with 13 (11.5%) and 1 (0.9%) hospitalized measles cases respectively. Pyuria was found in 18 of 97 cases tested (7 of 33 serologically confirmed measles cases had abnormal urine), abnormal chest X-ray in 12 of 58, abnormal liver function tests in 4 of 8, abnormal stool examination in 7 of 16, high ESR in 36 of 81, leukopenia in 28 of 110 and leukocy-tosis in 6 of 110 of cases tested. Laboratory tests were performed on the basis of the patient’s signs and symptoms.
Rashes began at the head and progressed toward the legs in 76.1% of hospitalized patients and in 15.9% of hospitalized patients the rash began in the extremities.
Mean duration of fever was 5.7 days, cough 5.4 days, rash 2.8 days, conjunctivitis 4.6 days and Koplik signs 2.6 days at the time of admission. Mean duration of patient’s hospitalization was 3.8 days. Characteristics of the 33 hospitalized patients who were confirmed serologically are shown in Table 3.
Discussion
The average of incidence during 1997–2003 in the Islamic Republic of Iran and Ghazvin district was 11.23 per 100 000 and 18.67 per 100 000 population respectively. Thus the Ghazvin region had a high incidence compared with that of the whole of the country while according to records of Ghazvin district, vaccination coverage was over 90% in the past 15 years.
The highest incidence of clinically diagnosed measles in Ghazvin in the study period was in 2001–2002 but for serologically confirmed cases it was in 2000–2001. The highest incidence of clinically confirmed measles was 32 per 100 000 population but according to WHO figures it was 14 per 100 000 population for the whole of the Islamic Republic of Iran for the same time.
Of the 591 clinically diagnosed cases of measles, 71.7% had serum samples available for laboratory analysis but only 24.2% were serologically confirmed. This is low compared with other countries in the Region; for example in Morocco and Egypt, 82% of cases had serum specimen for serological analysis [7].
Of the clinically confirmed measles cases that had serum specimens, 33.7% were confirmed for measles antibody IgM. Again, this rate is low compared with other studies in the Islamic Republic of Iran. One study reported 39% with confirmed IgM [8] and another reported a rate of 63.9% [9]. However, our figure is higher than those reported from studies outside the country. For example in a study in the United States the figure was 6.2% in 1999 and 1.18% in 2000 [10] and in Oman, the highest rate of serologically confirmed measles cases du-
ring 1996–2000 was 43% while the lowest was less than 21% [11]. Data from other EMR countries show that measles had a high incidence but the percentage of serologically confirmed cases was low [7].
Analysis of the vaccination status of measles cases in our district indicates that 89.2% of clinically and 70.3% of serologically diagnosed measles cases had received at least 1 dose of vaccine, suggesting a high rate of vaccine failure. This is high compared with other studies both in the country and outside. For example, in a study that was performed on serum specimens in the Islamic Republic of Iran during 1996–1997 the rate was 0.9% [8] and in a study in India it was 19.7% [12].
Of serologically confirmed measles cases, there was a sudden increase in the number of cases from the under-5 age group to the 5–9-year-old age group, despite the fact that 86% had received at least 1 dose of the vaccine. Thereafter there was a steady increase in measles cases with age. This sudden increase, together with the increase in cases with age, may suggest that the hypothesis of decreasing antibodies is valid. Decreasing antibodies in adolescents was shown in one study in Shiraz by measuring antibody level in different age groups after vaccination [13]. In another study performed in Iranshahr during 1994–1995, only 63% of 2–5-year-old children who had received 2 doses of vaccine had in fact any antibodies against measles [14]. These data indicate the necessity of further serological studies to determine the need for additional vaccination at later ages.
The mean age of the clinically and serologically diagnosed measles cases was 13.5 years and 17.5 years respectively. This is similar to other studies in the Islamic Republic of Iran; in one study 35.7% of patients were over 15 years [9]. In a study in Turkey, however, the mean age of measles cases was 3.79 years [15] and in England 58.8% of measles cases were under 15 years [16]. This suggests that in our area, the incidence of measles has shifted to older age groups (adolescents).
The hospitalized cases in our study tended to be older, which may again suggest decreasing antibodies over time and also that the severity of illness in greater in adults [4].
Incidence of measles in urban areas was higher than in rural areas which may suggest lower case detection in villages or higher urban incidence as a result of over-crowding in cities.
In serologically confirmed cases, the male to female ratio was 1.6:1 which is similar to another study in the country where 82.3% of cases were male [9]. However, generally measles is considered to affect both sexes equally [4] and the difference may be related to the culture of the society whereby males (e.g. as soldiers) are more exposed than females.
Common complications in both clinically and serologically confirmed measles cases were gastrointestinal complications, while in textbooks and other articles, respiratory and nervous system complications are given as the commonest complications [17,18]. This may be related to severity of the gastrointestinal complications in the measles cases in this region that led to hospitalization.
Urinary tract complications, such as dysuria, frequency, gross haematuria, and also abnormal laboratory findings were seen in hospitalized clinically confirmed measles cases. We found that 1 in 4 of the serologically confirmed cases had abnormal urine, which may be due to fever or to a secondary bacterial infection. One patient had haematuria but no other urinary complications were.
In 15.9% of clinically confirmed cases and 22.2% of serologically confirmed cases, rashes begun at the extremities and progressed towards the head. In a similar study in India this figure was 16.2% of clinically confirmed cases [12]. These findings suggest a possibility of atypical measles with the usage of live vaccine but only 1 in 4 of these atypical measles cases were confirmed serologically. This indicates that when illness appears in an atypical form there is a possibility of a measles-like illness.
Conclusion
There appears to be adequate vaccination coverage in our area, with about 89% of clinically confirmed cases with a clear history of vaccination. Because such a high proportion of patients contracting measles had in fact been vaccinated and a large proportion were school-aged children, an additional vaccination dose in children 5–9 years and in adults could reduce the incidence of measles in this district. Furthermore, serological studies after vaccination to determine antibody levels would be useful.
There is a need to improve health centre facilities in order to increase the rate of serological confirmation of clinically diagnosed measles cases.
Acknowledgements
We acknowledge the help of Dr Parviz Ayazi (paediatrician expert in infectious disease) and we thank Ahmad Rezaie, Zahra Saadatmand and the clerks in the archive section of Quds and Boalisina hospitals for obtaining data and Banafsheh Peyrovian for computing analysis of data.
References
- World Health Organization. Measles. Available at: http://www.who.int/topics/measles/en/ (accessed 21 September 2005).
- Forty-fourth Session of the Regional Committee for the Eastern Mediterranean Teheran, Islamic Republic of Iran, 4 to 7 October 1997. Resolutions. Available at http://www.emro.who.int/governance/PDF/RC44_Resolutions.pdf (accessed 23 September 2005).
- Braunwal D et al., eds. Harrison’s principles of internal medicine, 15th ed., Vol. 2. Columbus, McGraw–Hill Professional Publishing, 2001.
- Feigin RD et al., eds. Textbook of pediatric infectious diseases, 5th ed. Philadelphia, WB Saunders, 2003:chapter 183.
- Immunization surveillance, assessment and monitoring. Measles reported cases. Available at: www.who.int/immunization_monitoring/en/globalsummary/timeseries/tsincidencemea.htm (accessed 24 September 2005).
- Immunization surveillance, assessment and monitoring. Immunization profile - Iran (Islamic Republic of). Available at: www.who.int/immunization_monitoring/en/globalsummary/countryprofileresult.cfm?C=’irn’ (accessed 24 September 2005).
- Gaafar T, Moshni E, Lievano F. The challenge of achieving measles elimination in the Eastern Mediterranean Region by 2010. Journal of infectious diseases, 2003, 187(1):S164–71
- Mokhtari Azad T et al. [Epidemiological feature of measles in Iran, 1995–1996]. Hakim research journal, 1379 [2000 AD], 1(3):19–26 [in Persian].
- Sadeghi Pour Roudsari HR et al. [The study of measles cases and suspected cases in southern Tehran (1379)]. Journal of the Tehran Faculty of Medicine, 1381 [2000 AD], 2(60): 100–60 [in Persian].
- Venczel L et al. The measles laboratory network in the region of the Americas. Journal of infectious diseases, 2003, 187(1):S140–5.
- Kohler KA et al. Immunogenicity of measles and rubella vaccines in Oman: a prospective clinical trial. Journal of infectious diseases. 2003, 187(1):S177–85.
- Ray SK et al. Epidemiological study of measles in slum areas of Kolkata. Indian journal of pediatrics, 2004, 71(7):583–6.
- Karimi A et al. Measles antibody in different age groups of children in Shiraz (2000–2001). Iranian journal of infectious disease & tropical medicine, 1381 [2000 AD], 18(7):7–11 [in Persian].
- Moradi A, Salehi M, Rakhshani F et al. Seroepidemiological study of measles among 25–60 months children in Iranshahr district. Tabib-E Shargh (Journal of Zahedan University of Medical Sciences and Health Services), 1380 [20001 AD], 9:137–42 [in Persian].
- Caksen H et al. Measles is still a severe problem in Eastern Turkey. Journal of the Medical Association of Thailand, 2004, 87(4):387–8.
- Ramsay ME et al. The elimination of indigenous measles transmission in England and Wales. Journal of infectious diseases, 2003, 187(1):S198–207.
- Mandell GL, Bennett JE, Dolin R. Mandell’s principles & practice of infectious diseases, 5th ed. New York, Churchill Livingstone, 2000:782; 1801–7.
- Ariyasriwatana C, Kalayanarooj S. Severity of measles: a study at the Queen Sirikit National Institute of Child Health. Journal of the Medical Association of Thailand, 2004, 87(6):58.


