Research article
H.M. El Kady 1 and H.K. Ibrahim 1
الاكتئاب لدى مجموعة من المسنّين في الإسكندرية، مصر
هبة محمود القاضي، هالة قدري إبراهيم
الخلاصـة: يقدَّر أن الاكتئاب سيكون هو السبب الرئيسي للعبء المرضي لدى المسنّين في عام 2020. وتهدف هذه الدراسة لتقييم معدل انتشار الاكتئاب بين مجموعة من المسنّين في الإسكندرية، مصر، ومقارنة خصائص المسنين في ثلاثة مواقع مختلفة، وهي دراسة وصفية مستعرضة شملت مئة شخص ممن تزيد أعمارهم على ستين عاماً، يقيمون في أحد النزل الحكومية و فى أحد أجنحة قسم الأمراض الباطنة بالمستشفى الرئيسى الجامعى، وفي جناح الطب الباطني وفي أحد المناطق العشوائية في الإسكندرية. واستخدَمَت الباحثتان سلم مقياس الاكتئاب للمسنين (بشكله المختصر)، فوجدتا أن أعلى معدلات الانتشار التي تشير أو توحي بالاكتئاب كانت لدى المودعين بالمستشفى الذين أُدخلوا المستشفيات (%79)، أو الذين لديهم مرض عيني (%85.7)، أو أورام (%80)، أو لديهم أكثر من مرضَيْن مزمنَيْن (%64.9)، أو الذين يتناولون أكثر من أربعة أدوية يومياً (%83.3)، أو الذين يعتمدون بدنياً على غيرهم أكثر من سواهم، أو الذين أدخلوا المستشفى لأكثر من مرتين خلال السنوات الثلاث المنصرمة (%90.9). وتَمَسُّ الحاجة للنظر في العوامل القابلة للتعديل والتي تؤثِّر على الاكتئاب لابتكار تدخلات تستهدف تحسين الأحوال المزاجية لدى المسنين.
ABSTRACT Depression is projected to be the leading cause of disease burden in older populations by the year 2020. The aim of this study was to assess the prevalence depression among a group of elders in Alexandria, Egypt and compare the characteristic of elders in 3 different settings. A descriptive, cross-sectional study was carried out among 100 people aged 60+ years in a government elderly home, an internal medicine ward in Alexandria Main University Hospital and a slum area in Alexandria. Based on the Geriatric Depression Scale (short form) the highest prevalence of scores that were suggestive or indicative of depression was among elders who were hospitalized (79.0%), had ophthalmic diseases (85.7%) or tumours (80.0%), had 2+ chronic morbidities (64.9%), were taking 4+ medications daily (83,3%), were more physically dependent and had had 2+ hospital admissions in the last 3 years (90.9%). Modifiable factors that impact on depression need to be considered in developing interventions for improving mood states in the elderly.
Dépression dans un groupe d'anciens à Alexandrie (Égypte)
RÉSUMÉ Il a été estimé que la dépression représenterait la cause principale de la charge morbide dans les populations de personnes âgées d'ici 2020. L'objectif de la présente étude était d'évaluer la prévalence de la dépression dans un groupe d'anciens à Alexandrie (Égypte), et de comparer les caractéristiques de ces derniers dans trois milieux différents. Une étude transversale descriptive a été menée auprès de 100 personnes âgées de plus de 60 ans dans une maison de retraite du gouvernement, dans un service de médecine interne et dans un bidonville à Alexandrie. À partir de la version abrégée de l'échelle gériatrique de dépression, les scores indiquant ou suggérant une dépression étaient plus élevés dans les populations suivantes : les anciens hospitalisés (79,0 %), les personnes âgées souffrant de maladies ophtalmiques (85,7 %) ou de tumeurs (80,0 %), atteintes de plus deux comorbidités chroniques (64,9 %), ou prenant plus de quatre traitements quotidiens (83,3 %), ou davantage dépendants physiquement et admis plus de deux fois à l'hôpital au cours des trois années précédentes (90,9 %). Les facteurs modifiables ayant un impact sur la dépression doivent être pris en compte dans l'élaboration d'interventions visant à lutter contre la dépression chez les anciens.
1Department of Family Health, High Institute of Public Health, University of Alexandria, Alexandria, Egypt (Correspondence to H.K. Ibrahim:
Received: 15/02/12; accepted: 21/02/12
EMHJ, 2013, 19(2):167-174
Introduction
Depression is an important problem that may highly influence the quality of life of elderly people in different settings. The prevalence of depression in people aged 65 years and older may be as high as 40% in hospitalized and 30% in nursing home patients and 8%–15% in community settings. Studies of depressed elders indicate that they have comparable or poorer physical functioning than elders with chronic medical conditions such as heart and lung diseases, arthritis and diabetes [1,2]. Depression can increase perceptions of poor health, the utilization of medical services and health care costs. Conversely, a diagnosis of certain chronic diseases may trigger symptoms of depression [3].
There are many factors related to depression among elders. It has been attributed to the increasing stressors with age resulting from declining health and dwindling social relationships [4]. Low socioeconomic status was found to be significantly associated with depression after adjustment for age, illness, sex and self-rated health [5]. Presence of comorbidity may correlate with depression among the elderly. Also, several clinical trials reported a positive correlation of depression with functional decline, impairment in activities of daily living (ADL) and a steep decline in strength [6].
Research suggests that the living environment of older adults is an important determinant of health and longevity. Existing evidence indicates that the health care needs and costs of institutionalized persons are much higher than those of elders in other settings [7]. Significant differences have been found between elders residing in institutions or in the community in terms of mortality risk, daily functioning, disease prevalence, life satisfaction, depression and quality of life [8,9]. For many older adults, especially in developed countries, institutionalization represents a loss of independence, marked by feelings of limited usefulness, a loss of self-actualization, reliance on others and a general lack of mastery or sense of control. Institutionalized persons are typically those with no spouse or living children or with offspring who are not available to provide care [10]. In many cases, these individuals are considered abandoned by children who have not fulfilled their filial obligations. Consequently, the institutionalized are socially disadvantaged and depend on support from limited subsidies from local government or collectives [9]. Depression can also have adverse health effects for many hospitalized older adults. High levels of depressive symptoms are associated with poor treatment adherence, longer lengths of hospital stays, increase in hospital readmission and reduced functional status [11].
Most of the research on this subject is based on high-income countries and little is known about elders in developing countries. The aim of this study was to assess the prevalence of depression among elders in Alexandria, Egypt, and compare the characteristics of those from 3 different settings: hospitalized, institutionalized or community dwelling.
Methods
Study setting and sample
A descriptive, cross-sectional study was carried out among elders aged 60+ years in a government-run home for the elderly (Dar El Saada), an internal medicine ward in the Main University Hospital and a slum area (Ezbet Sekeena) in Alexandria city.
The sample included all elders who were able to communicate and agreed to participate in the study. Using a power of 80% to detect a difference of 37% [4,12] at the depression prevalence among hospitalized and community dwelling elders as the largest recorded difference in comparison to institutionalized elders, α-error = 0.05, the minimal required sample size was found to be 28 (increased to 33) for each group. The sample size was calculated using Epi-info 2002 software. We randomly selected 33 elders from institutions, 33 who were in hospital at the time of the study and 34 who were currently living in the community.
Data collection
A structured pre-coded interview schedule was used to collect data about sociodemographic characteristics and medical history (the type and number of chronic diseases from which the patient suffered, the number of medications he/she was taking and the number of hospital admissions in the 3 years before the study).
The Katz scale for ADLs was used to assess degree of dependency in performing the basic ADLs including bathing, dressing, toileting, transfer, urinary and faecal continence and feeding [13]. The 6 functions are measured and scored according to the individual’s actual performance of these functions. They are categorized into 3 levels of dependency: each item is scored from 0–2, where 2 = full independence without need for human assistance, 1 = partial dependence with the need for some help and 0 = total dependence with an inability to perform the task even with assistance. The total score of the scale is from 0–12. According to the scale patients are classified into 3 categories: totally independent (score 9–12), partially dependent (score 5–8) or totally dependent (score 0–4). The Katz scale was translated in to Arabic language and tested for reliability using test–retest ], which showed a Pearson correlation coefficient of 0.8.
The short form of the Geriatric Depression Scale (GDS) [14] was used to assess the presence or absence of depression among the elders. The responses to each item are yes/no (scored 1 or 0) and the total scores (15 items) are classified as follows: no depression (score 0–4), suggestive of depression (score 5–9), almost always indicative of depression (score > 9). The scale was translated into Arabic, and validated by the juries including 6 experts in administration and geriatric health. The required corrections and modifications were carried out accordingly. Reliability was tested using internal consistency and a reliability coefficient (Cronbach alpha) of 0.88 was found for the 15 items of the scale.
The study was approved by the ethics committee of the High Institute of Public Health, University of Alexandria before the start of the study and written approvals from the elders were taken before interviewing. Each elder was interviewed individually after explanation of the purpose of the study and assurances of confidentiality were given. Each individual interview took about 20 minutes. Data were collected during a period of 5 months from the beginning of March 2011 to August 2011.
Statistical analysis
Data management and computations of descriptive statistics and prevalence were performed using SPSS, version 16. Differences with P-value < 0.05 were considered statistically significant. The Pearson chi-squared, Monte Carlo exact and Fisher exact probability tests were used as tests of significance. There were no missing data.
Results
The mean age for hospitalized elders was 70.0 (SD 5.3) years, for community dwelling elders was 68.7 (SD 5.2) years and for institutionalized elders was 69.0 (SD 4.3) years. Among hospitalized and institutionalized elders the highest percentage were widowed (54.5% and 69.7% respectively) whereas more than two-thirds of those living in the community were married (67.6%). As regards education, the majority of hospitalized elders (78.8%) were illiterate or could only read and write, while the majority of community dwelling and institutionalized elders (82.4% and 60.6% respectively) were secondary school or university graduates. Just over half of the hospitalized (51.5%) and the majority of community dwelling elders (67.6%) considered there income was sufficient, but for the institutionalized elders more than one-third (36.4%) reported it as insufficient and the income of about half of them (48.5%) was not sufficient and they had to borrow money.
Figure 1 shows the distribution of the study sample according to the GDS scores. The majority of community dwelling and institutionalized elders had no depression (77.0% and 64.0% respectively), but the majority of hospitalized elders had scores that were suggestive or indicative of depression (58.0% and 21.0% respectively). The data also showed that 18.0% of community dwelling and 24.0% of institutionalized elders had scores that were suggestive or indicative of depression respectively.
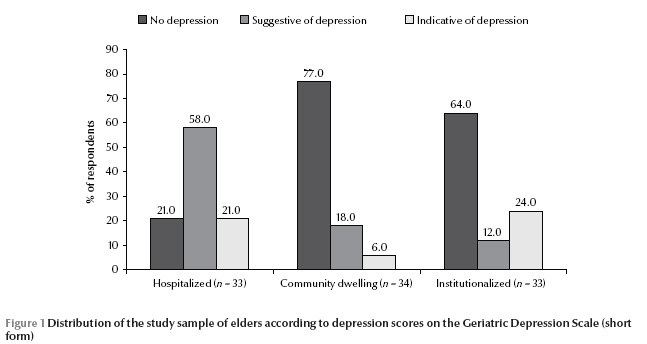
Table 1 1* shows the relation between GDS score and demographic variables. The percentage of elders with scores that were suggestive or indicative of depression were higher among those aged 75+ years (75.0%) compared with those aged 60–< 65 years (20.0%); among females (57.1%) compared with males (35.3%); in widowed or single (90.0% and 80.0%) than married elders (31.7%); among elders living with their offspring (68.4%) compared with those who lived in elderly homes (36.4%). The rate of depression was also higher among those who were illiterate/semi-literate (66.7%) than those having secondary/university education (24.5%); in those who were housewives (68.8%) versus those receiving a pension or had left work (33.9%); and those receiving social support (100%) rather than a pension (23.1%) and with insufficient income/borrowing money (100%) rather than a sufficient income (11.1%).
Table 1 also shows that more than half of the elders who had chronic diseases (54.1%) had scores that were suggestive or indicative of depression and more elders who had 2+ diseases had depression scores (64.9%) than those who had only 1 disease (32.1%) or no diseases (0%). Elders were also more likely to have depression scores if they were taking 4+ medications (83.3%) than 1–3 medications (41.2%) and were hospitalized 2+ times in the last 3 years (90.9%) than those who had no previous hospitalizations (35.5%).
The correlation between the GDS scores and Katz scale scores showed a significant inverse intermediate relation between score of Katz scale for ADL and level of depression as measured by the GDS among hospitalized (–0.43, P < 0.05), community dwelling (–0.4, P < 0.05) and institutionalized (–0.5, P < 0.01) elders and among the whole sample (–0.5, P < 0.01).
Table 2 shows the relationship between GDS scores and chronic morbidity. The highest percentage of GDS scores that were suggestive or indicative of depression was among chronically ill elders, with the highest rates among elders who had ophthalmic diseases (85.7%), tumours (80.0%) and renal diseases (100.0%).
Discussion
Depression is a major contributor to health care costs associated with older populations, and is projected to be the leading cause of disease burden in older populations by the year 2020 [2]. Several factors are related to the causes of depression. Some researchers have focused on socioeconomic variables such as advanced age, low education, poor economic status, manual occupation and current living situation as causes of depression, and demonstrated that these variables had a relationship with depression [8].
The present study showed that the highest rate of depression was among those aged 75+ years (75.0%) compared with younger age groups. This is in accordance with other studies, which reported similar findings [1,12]. This may be attributed to the fact that with increasing old age people experience a greater loss of physiological, psychological and social functioning and become increasingly prone to depression. However, some other studies indicated a lower prevalence of depression among the elderly [15,16]. Such inconsistency in the literature can be attributed to differences in the methodology and diagnostic criteria used.
The present study also found that depression was more prevalent among females. This agrees with numerous epidemiological studies showing that women have a higher prevalence of depression than men across generations and cultures [17,18] and that sex differences in the prevalence of depression, which first become apparent in early adolescence, continue into the 60+ years age group. In addition, most studies have shown that women are more exposed to risk factors for depression, such as financial difficulties, widowhood, social isolation, low education and functional disability.
The present study revealed that depression was more prevalent among widowed and single elders, who may suffer a sense of loneliness and bereavement that aggravates feelings of sadness among such elders. This is in accordance with a study in Korea which reported that widowhood significantly influenced depression among older adults [19].
Socioeconomic variables, such as low education, poor economic status and current living situation, have been reported as causes of depression among elders in previous studies [1,8]. The present study revealed that depression was more prevalent among elders of lower educational status, which may reflect their lower socioeconomic status, which in turn may mean that they are exposed to more life stressors. The present study also revealed that depression was more prevalent among elders whose source of income was social support and among those who reported their income as insufficient. This agrees with a study in Japan which found that low socioeconomic status was significantly associated with depression, after adjustment for age and sex [20].
The present study revealed that depression was more prevalent among chronically ill elders, especially those with 2 or more diseases, who received 4 or more medications daily and those who had ophthalmic diseases, tumours and renal diseases. This is in accordance with other studies which found that depressive symptoms were higher among chronically ill elders, especially those who had diabetes, stroke, cardiac disease, chronic lung disease and hypertension [2,21]. Several factors associated with depressive symptoms, including obesity-promoting health behaviours (e.g., physical inactivity, hypercaloric diets) and activation of the neuroendocrine and inflammatory responses (resulting in increased cortisol, catecholamines and cytokines), can induce the development of these chronic diseases. These associations may be also related to increased risk of depressive symptoms in individuals with these chronic diseases, increased risk of these chronic diseases in individuals with depressive symptoms or both [2].
In the present study, depression was more prevalent among elders who had 2 or more previous hospital admissions. This agrees with a study in the United States, which showed that high rates of depressive symptoms were associated with more frequent hospital admissions [11]. The present study also revealed that there was an inverse relationship between scores on the Katz scale for ADL and level of depression as measured by the GDS among the study sample. This is in accordance with several clinical trials that reported a positive correlation of depression with functional decline and impairment of ADL [22,23]. This is due to the fact that physical dependence brings about marked feelings of limited usefulness, loss of self-actualization, reliance on others and a general lack of mastery or sense of control.
Research suggests that the living environment of older adults is an important determinant of their health and longevity. Existing evidence indicates that the health care needs of institutionalized persons are much higher than those of elders in other settings [9]. Significant differences have also been found between institutionalized and community-residing individuals in mortality risk, daily functioning, disease prevalence, life satisfaction, depression and quality of life [11]. In addition, depression can have adverse health effects for many hospitalized older adults. High levels of depressive symptoms are associated with poor treatment adherence, longer lengths of stay, increase in hospital readmission and reduced functional status [24]. Compounding this relationship is the fact that hospitalization can increase depressive symptoms in many older adults. The prevalence of depressive symptoms was as high as 50% among hospitalized older adults in a study in Australia, yet it was reported to be much lower in persons 3–12 months after hospital discharge [25]. The present study revealed similar findings; depression was more prevalent among hospitalized and institutionalized elders than among those living in the community.
Most of the previous studies on geriatric depression have focused on its high prevalence. They have not attempted to reduce the occurrence of depression among elders. The way in which depression among the elderly is related with their residence and competence of ADL has rarely been studied. The identification of factors to predict the depression level among the elderly population can pave the way to developing effective interventions for decreasing geriatric depression. Any interventions should be focused on factors that are modifiable or on the behavioural characteristics which contribute to depression.
Conclusion
In conclusion, depression rates were higher among hospitalized and institutionalized elders, among women, widowed and single elders, among housewives, among those living with their offspring only and among more physically dependent elders. Depression was also more prevalent among elders whose source of income was social support and among those whose income was insufficient. It was more prevalent among elders having 2 or more chronic morbidities, those taking 4 or more medications daily and those who had 2 or more hospital admissions in the last 3 years. It is recommended that modifiable factors such as competence in ADL, presence of chronic morbidities and degree of social and financial support should be considered as variables in developing interventions for improving mood states in the elderly.
References
- Huang CQ et al. Chronic diseases and risk for depression in old age: a meta-analysis of published literature. Ageing Research Reviews, 2010, 9:131–141.
- Von Korff M et al. Disability and depression among high utilizers of health care. A longitudinal analysis. Archives of General Psychiatry, 1992, 49:91–100.
- Carvalhais SM et al. The influence of socio-economic conditions on the prevalence of depressive symptoms and its covariates in an elderly population with slight income differences: the Bambuí Health and Aging Study (BHAS). International Journal of Social Psychiatry, 2008, 54:447–456.
- Borson S et al. Geriatric mental health services research: strategic plan for an aging population. American Journal of Geriatric Psychiatry, 2001, 9:191–204.
- Demura S, Sato S. Relationships between depression, lifestyle and quality of life in the community dwelling elderly: a comparison between gender and age groups. Journal of Physiological Anthropology and Applied Human Science, 2003, 22:159–166.
- Rantanen T et al. Depressed mood and body mass index as predictors of muscle strength decline in old men. Journal of the American Geriatrics Society, 2000, 48:613–617.
- Federal Interagency Forum on Aging Related Statistics. Older Americans 2004: key indicators of well-being. Washington DC, US Government Printing Office, 2004.
- Van Dijk PT et al. Comorbidity and 1-year mortality risks in nursing home residents. Journal of the American Geriatrics Society, 2005, 53:660–665.
- Harris Y, Cooper JK. Depressive symptoms in older people predict nursing home admission. Journal of the American Geriatrics Society, 2006, 54:593–597.
- Davis MA et al. Living arrangements, changes in living arrangements, and survival among community dwelling older adults. American Journal of Public Health, 1997, 87:371–377.
- Carrie A et al. Patterns and correlates of depression in hospitalized older adults. Archives of Gerontology and Geriatrics, 2011, 30:33–36.
- Jeon HS, Dunkle RE. Stress and depression among the oldest-old: a longitudinal analysis. Research on Aging, 2009, 31:661–687.
- Katz S et al. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychological functions. Journal of the American Medical Association, 1963, 185:914–919.
- Sheikh JI, Yesavage JA. Geriatric Depression Scale: recent evidence and development of a shorter version. In: Brink TL, ed. Clinical gerontology. New York, Haworth Press, 1986:112.
- Copeland JR et al. Depression in Europe. Geographical distribution among older people. British Journal of Psychiatry, 1999, 174:312–321.
- Mara Cristina F et al. Depressive symptoms and cognitive performance of the elderly: relationship between institutionalization and activity programs. Revista Brasileira de Psiquiatria, 2006, 28:118–121.
- Wang JK, Su TP, Chou P. Sex differences in prevalence and risk indicators of geriatric depression: the Shih-Pai community-based survey. Journal of the Formosan Medical Association, 2010, 109:345–353.
- Zunzunegui MV et al.; CLESA Working Group. Gender differences in depressive symptoms among older adults: a cross-national comparison: the CLESA project. Social Psychiatry and Psychiatric Epidemiology, 2007, 42:198–207.
- Shin KR et al. Depression among community-dwelling older adults in Korea: a prediction model of depression. Archives of Psychiatric Nursing, 2009, 23:50–57.
- Murata C et al. Association between depression and socio-economic status among community-dwelling elderly in Japan: the Aichi Gerontological Evaluation Study (AGES). Health and Place, 2008, 14:406–414.
- Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. European Heart Journal, 2006, 27:2763–2774.
- Unützer J et al. Depressive symptoms and mortality in a prospective study of 2,558 older adults. American Journal of Geriatric Psychiatry, 2002, 10:521–530.
- Onishi J et al. The relationship between functional disability and depressive mood in Japanese older adult inpatients. Journal of Geriatric Psychiatry and Neurology, 2004, 17:93–98.
- Cullum S et al. Does depression predict adverse outcomes for older medical inpatients? A prospective cohort study of individuals screened for a trial. Age and Ageing, 2008, 37:690–695.
- Brodaty H et al. Rates of depression at 3 and 15 months poststroke and their relationship with cognitive decline: the Sydney Stroke Study. American Journal of Geriatric Psychiatry, 2007, 15:477–486.


