M. Heidari 1 and F. Najafi 1
اتجاهات معدلات حدوث سرطان الجلد في ستة مناطق جغرافية في جمهورية إيران الإسلامية 2000 - 2005
محمد حيدري، فريد نجفي
الخلاصـة: هناك غياب للمعطيات حول معدل حدوث سرطان الجلد في جمهورية إيران الإسلامية. وتستقصي هذه الدراسة اتجاهات معدلات حدوث سرطان الجلد (الراموز 44 C في الإخراجة العاشرة للتصنيف الدولي للأمراض)، وسرطانات الجلد غير الـميلانومية)؛ في ست مناطق، باستخدام المعطيات المستمدة من السجل الإيراني للسرطان للفترة 2000 – 2005. وقد حَسَبَ الباحثان معدلات الحدوث المعيارية لكل عام بطريقة مباشرة، باستخدام نموذج منظمة الصحة العالمية المعياري للسكان، وتحوُّف بواسون، وتطبيقهما على اتجاهات التحليل. واتضح لهما أنه خلال فترة الدراسة، تم تشخيص 701 30 حالة سرطان، كانت 2353 في عام 2000 وارتفعت إلى 8484 في عام 2005. وكانت نسبة الذكور إلى الإناث = 1.6، وارتفع معدل الحدوث المعيَّر وفقاً للعمر ارتفاعاً يعتد به إحصائياً من 3.8 حالة لكل مئة ألف عام 2000 إلى 13.0 حالة لكل مئة ألف عام 2005 (الـمَمَال = 0.26)؛ كما لوحظ الاتجاه ذاته في جميع المناطق باستثناء منطقة شرق بحر قزوين. ويرى الباحثان أن الازدياد في معدل حدوث سرطان الجلد في جمهورية إيران الإسلامية مشابه لما سُجِّل في البلدان الأخرى.
ABSTRACT Data about the incidence of skin cancer in the Islamic Republic of Iran are lacking. This study investigated trends in the incidence of skin cancer (ICD-10 category C44, other malignant neoplasms of skin) in 6 regions using data from the Iranian cancer registry from 2000 to 2005. The standardized incidence rates in each year were calculated by the direct method using the standard World Health Organization population and a Poisson regression model was applied to analyse trends. Over the study period, 30 701 cases of cancer were identified, rising from 2353 in 2000 to 8484 in 2005. The male-to-female ratio was 1.6. The age-standardized incidence rose significantly from 3.8 cases per 100 000 in 2000 to 13.0 in 2005 (slope = 0.26), and the same trend was seen in all regions except the region to the east of the Caspian Sea. This increasing incidence of skin cancer in the Islamic Republic of Iran is similar to that reported in other countries.
Évolution de l'incidence du cancer de la peau dans six régions géographiques de la République islamique d'Iran entre 2000 et 2005
RÉSUMÉ Les données sur l'incidence du cancer de la peau en République islamique d'Iran font défaut. L'étude a examiné l'évolution de l'incidence du cancer de la peau (CIM-10 catégorie C44, autres tumeurs malignes de la peau) dans six régions à partir des données du registre du cancer iranien entre 2000 à 2005. Les taux d'incidence normalisés chaque année ont été calculés par méthode directe à l'aide de la population type de l'Organisation mondiale de la Santé. Un modèle de régression de Poisson a été appliqué pour analyser les évolutions. Pendant la période de l'étude, 30 701 cas de cancer ont été identifiés, passant de 2353 en 2000 à 8484 en 2005. Le rapport hommes/femmes était de 1 pour 6. Le taux d'incidence normalisé selon l'âge a nettement augmenté, passant de 3,8 cas pour 100 000 en 2000 à 13,0 en 2005 (pente = 0,26), et la même évolution a été observée dans toutes les régions à l'exception de la région située à l'est de la mer Caspienne. L'incidence croissante du cancer de la peau en République islamique d'Iran est similaire aux incidences notifiées dans d'autres pays.
1School of Public Health, Kermanshah University of Medical Sciences, Kermanshah, Islamic Republic of Iran (Correspondence to F. Najafi:
Received: 22/11/11; accepted: 26/01/12
EMHJ, 2013, 19(1):59-65
Introduction
Skin cancer is the most prevalent type of cancer in Caucasian populations (Indo-Europeans) [1]; 80% of the total incidence is observed in the United States (US), Europe, Australia and New Zealand [2]. In the US only, more than 1 million new cases of skin cancer were diagnosed in 2009 and approximately 12 000 people lost their lives in the same year [3]. There are 2 types of skin cancer: melanoma and non-melanoma. While melanoma accounts for only 1% of cases of skin cancer [4], it is considered the main cause of mortality from the disease [3]. As for the non-melanoma type, Caucasians have the highest incidence compared with Asian and Hispanic races. However, it rarely occurs in black populations [5–7]. Monitoring the incidence of skin cancer has shown that there is an increasing trend in most countries in the world. Some examples are the Netherlands, where the incidence increased by 80% between 2000 and 2005 [8], and Brazil, where the incidence increased from 50 cases per 100 000 in 2000 to 94 per 100 000 in 2006 [9].
The important risk factors for skin cancer are high exposure to solar ultraviolet (for both melanoma and non-melanoma types) and racial susceptibility of Caucasians [3]. Decreasing latitude is associated with increased incidence of non-melanoma skin cancer [10]. For example in Queensland, Australia, the incidence is higher than in Europe and North America [2]. Although sunlight is an important risk factor, the development of skin cancer is mainly related to solar ultraviolet radiation [3,8,11], the dose of which are thought to be increasing as a result of thinning of the ozone layer of the atmosphere [12]. Among other risk factors are high alcohol consumption [13], diets high in fat and meat [14] and genetic predisposition [15].
In the Islamic Republic of Iran, skin cancer is also the most prevalent cancer [16,17] with a male-to-female ratio of 1.6 [18]. In 2004, a study in Golestan province showed that the incidence of skin cancer in men aged 80+ years was 161.9 per 100 000, the highest reported rate for skin cancer worldwide [19]. From the epidemiological viewpoint, the peak of skin cancer incidence in Islamic Republic of Iran is observed in the 7th and 8th decades of life [18] and is mostly reported in farmers [20].
The present study was designed to evaluate the age-standardized incidence trend for non-melanoma skin cancer from 2000–05, based on data from the Iranian cancer registry. The results of the study were expected to inform policy-makers about future trends in skin cancer in the Islamic Republic of Iran in order to plan health interventions.
Methods
Data sources
In this population-based study data were obtained from the national cancer registry at the Centre for Disease Control of the Iranian Ministry of Health. Each year, cancer data are collected from all pathology centres across the country. The data received are then monitored for errors in coding, demographic information, duplicates and missing identities. It should be noted that recording and reporting cases of cancer became mandatory in 1984 in the Islamic Republic of Iran, and the first report was published in 1986. With the development of the Pars software, the Iranian national cancer registry was improved in 2000. Cancers are classified according to the International Classification of Disease (ICD-10) second revision [21].
Coding and analysis
For the purpose of this study, we used ICD-10 category C44 for skin cancer, non-melanoma type (other malignant neoplasms of skin). The country was divided into 6 geographical regions: south and west of the Caspian Sea (Gilan and Mazandaran provinces), east region of the Caspian Sea (Golestan province), flat region (Tehran, Qom, Qazvin, Zanjan, East Azerbaijan, West Azerbaijan and Ardebil provinces), mountainous region (Kermanshah, Kurdestan, Hamedan, Ilam, Chaharmahal va Bakhtiari and Kohkiluye va Buyerahmad provinces), desert region (Fars, Kerman, Sistan va Baluchistan, Yazd, Semnan, Khorasan, Birjand and Isfahan provinces) and region around the Persian Gulf (Khuzestan, Bushehr and Hormozgan provinces). Cases with no information on residential province were considered in the calculation of overall national incidence rate and not in calculations for different geographical regions.
For standardization of incidence, the results of the national population consensus of 2006 were used [22]. Considering the annual population growth rate of 1.01%, the population of different geographical regions was determined for 2000, 2001, 2002, 2003, 2004 and 2005. The World Health Organization (WHO) standard population was used as the reference population [23].
Using direct methods and STATA software, version 11, age–sex incidence rates and 95% confidence interval (CI) for the country overall and for the 6 geographical regions were calculated. The significance of incidence trends was tested by a Poisson regression model. All graphs were drawn with Microsoft Excel 2007.
Results
Over the 6-year period of the study, 30 701 cases of skin cancer were registered in the Islamic Republic of Iran, with an increase from 2353 cases in 2000 to 8484 cases in 2005. The male-to-female ratio was 1.6. The mean age was 61.4 [standard deviation (SD 14.6)] years: 60.0 (SD 14.9) for women and 62.0 (SD 14.3) for men. There was a significant increase in age-standardized incidence from 3.8 cases per 100 000 in 2000 to 13.0 cases per 100 000 in 2005. This increasing trend was observed with various gradients in all the 6 geographical regions of the country.
The age-standardized incidence for men was higher, rising from 4.5 cases per 100 000 in 2000 to 16.0 cases in 2005, while the rate for women increased from 3.0 cases per 100 000 in 2000 to 9.8 cases in 2005 (Table 1).
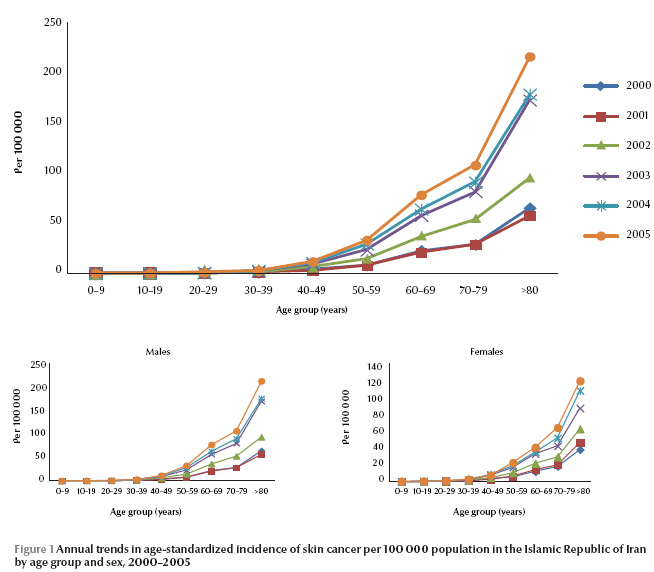
Despite different gradients of incidence trend for different years, the trend across age groups was similar each year: a very slow rise in the age groups < 20 years, with a 4-fold increase by the age group 50–59 years, rising sharply thereafter up to the age 80+ years, where it reached the highest incidence (Figure 1).
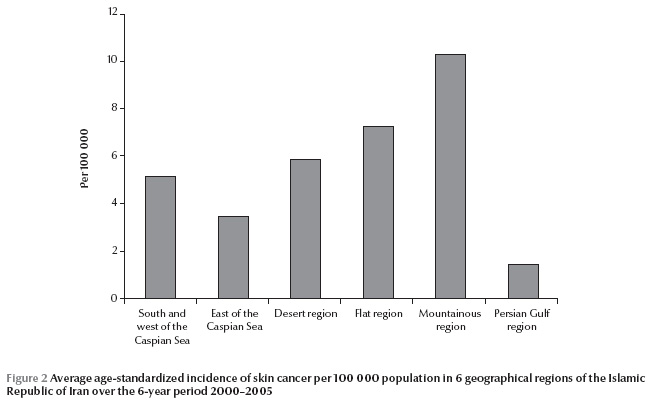
Over the period of the study and on average, the highest incidence of skin cancer occurred in the mountainous region followed by the flat and desert regions (Figure 2).
South and west of the Caspian Sea
The region with the highest amount of rainfall ranked 4th for average incidence of skin cancer (Figure 1 ). The age-standardized incidence for skin cancer increased significantly from 2.6 cases per 100 000 in 2000 to 8.9 cases in 2005. In 2001, the incidence fell sharply to half the figure of 2000, only to bounce back 3-fold in 2002. The trend was steady for 2005, rising only 0.4 per 100 000 above the figure for 2004. The incidence trend for both sexes was similar, with the age-standardized incidence decreasing in 2001, and then increasing onwards with almost the same gradients (Table 1 ). However, as seen in other regions, the incidence for men was higher.
East of the Caspian Sea
Except for 2001, where the incidence of skin cancer rose dramatically to 5.4 cases per 100 000, the regional incidence was lower than that of the other regions of the Caspian Sea (Table 1). The region saw an increase from 1.0 cases per 100 000 in 2000 to 6.1 cases in 2005. The changes in incidence trend for both sexes were very similar, with a rise observed in 2001. Apart from 2000, the incidence of skin cancer was higher for men. The Poisson regression test showed a significant trend in men only.
Mountainous region
The mountainous region had the highest incidence of skin cancer compared with the other regions (Figure 2). Except for 2000, the age-standardized incidence was higher than other regions. There was an increasing trend in incidence, with 4.5 cases per 100 000 in 2000 rising to 16.1 cases in 2005. The age-standardized incidence for men rose dramatically from 5.4 cases per 100 000 in 2000 to 19.7 cases in 2005, the highest incidence among the regions. The figure for women increased from 3.5 cases per 100 000 in 2000 to 12.5 cases in 2005 (Table 1). The trend was similar for both sexes.
Desert region
This region was ranked 3rd considering the 6-year average incidence, after the mountainous and flat regions (Figure 2). Like other regions, the general trend of age-standardized incidence was increasing from 5.8 cases per 100 000 in 2000 reaching 12.4 cases in 2005. In 2001, the incidence was almost half that of the previous year before rising in 2002. The increase had a steeper gradient from 2003 onwards. Trends of incidence in men and women were similar (Table 1). Both sexes showed a decrease in incidence in 2001 and a gentle gradient up to 2003, followed by a large increase from 2003 onwards.
Flat region
This region came 2nd after the mountainous region in terms of the highest risk for skin cancer (Figure 2). The age standardized rate increased from 2.2 cases per 100 000 in 2000 to 15.1 cases in 2005, indicating a 7.5-fold increase in incidence over the period. After a slight decrease in 2002, the occurrence of skin cancer increased sharply. The trend for age-standardized incidence was similar for men and women with both dropping slightly in 2002. The incidence for men was higher and rose from 2.3 cases per 100 000 in 2000 to 18.7 cases in 2005. The figure for women rose from 2.0 to 11.5 cases per 100 000 in the same period (Table 1).
Region around the Persian Gulf
The region around the Persian Gulf had the lowest incidence of skin cancer (Figure 2). In fact, the average 6-year incidence was 10 times lower than in the mountainous region, where the greatest number of cases was found. Here the trend was also upwards, albeit with a gradient lower than other regions. The age-standardized incidence increased from 0.05 cases per 100 000 in 2000 to 3.0 cases in 2005. Unlike other regions and similar to the mountainous region, there was an increase in the incidence in all the years under study. The difference between the incidence of skin cancer in men and women was small and slightly higher for women (contrary to other regions). While the age-standardized incidence for men increased from 0.04 cases per 100 000 in 2000 to 3.0 in 2005, women showed an increase from 0.05 to 2.9 cases per 100 000 in the period. Although the incidence for men experienced a continuous increase, the rate for women decreased slightly in 2004.
Discussion
Overall, the results of the study showed an upwards trend in the incidence of skin cancer in the Islamic Republic of Iran, with a 3.4-fold increase over the 6-year period. Although a rising trend was observed in all regions the change gradient was different, with the lowest and highest increases in incidence for the mountainous and Persian Gulf regions respectively. In all regions, the incidence was higher for men and for both sexes the incidence rose slowly at younger ages and accelerated at older age groups up to 80+ years.
This finding of an increased incidence of skin cancer in the Islamic Republic of Iran is compatible with findings from studies other in other countries. For instance, Italy [24], the Netherlands [25], England [26], Brazil [9], Finland [27] and Pakistan [28] have all reported an increased incidence of skin cancer. However, despite the global increase in the incidence, the mortality rate from the condition has decreased, especially in the US and Europe [29]. Researchers consider higher rates of reported (due to higher awareness of the symptoms and early detection) [30], thinning of the ozone layer and thus higher exposure to ultraviolet light [12], changes in people’s exposure to sunlight and bad sun protection habits [31] and diet changes towards higher intake of fat and meat [32] as the major underlying causes of the increased incidence of skin cancer.
In recent years, Iranians have gained greater awareness of skin cancer symptoms and its complications. For instance, a study by Montazeri et al. showed that 95% of skin cancer patients were eager to know more about cancers [33]. At the same time, improvements in the health services in Islamic Republic of Iran has made diagnosis easier [34], perhaps explaining the increased incidence of skin cancer. Furthermore, the country has followed similar changes in nutritional patterns as developed countries, from lower-calorie diets rich in vegetables and fruits to fatty and high-calorie foods [35]. There is also direct relationship between skin cancer and working outdoors and direct exposure to sunlight [10,36]. This is likely to be one of the underlying causes of increases in the incidence of skin cancer in rural regions of Islamic Republic of Iran. Zamanian et al. showed that in Hamedan most skin cancer patients were farmers who had a high exposure to sunlight [37]. Another study in Alexandria, Egypt showed a positive association of sun exposure and skin colour, in which the relative risk of skin cancer incidence was 4.8-fold greater in those with high exposure to sunlight [38].
The most important risk factor for skin cancer is skin colour and more than 80% of ultraviolet light damage occurs in individuals with sun-sensitive skins [2]. As mentioned earlier, the mountainous region had the highest incidence of skin cancer. This region has mild to cold weather and the population are mainly Turks, Lore and Kurd with white complexions susceptible to skin cancer. On the other hand, the region around the Persian Gulf had the lowest incidence of skin cancer. Interestingly, the region has a hot and humid climate and its Fars and Arab inhabitants have darker skin, closer to black. This is in contrast to the theory that the incidence of skin cancer increases with decreasing latitude. An important finding regarding trends in different regions was that the steepest and lowest gradients were observed in the Persian Gulf and mountainous regions respectively.
While interpreting the results of our study, it should be noted that increases in the average age of the Iranian population, reflecting increases in life expectancy [24], may partly explain the steadily increasing incidence of skin cancer with age. Another important item to consider is the cancer registry system in the country. It has been shown that a large proportion of the increase in incidence is due to advances in diagnostic techniques and developments of the cancer registry system [39]. Despite the recent improvement in the cancer registry in the Islamic Republic of Iran, there are still some problems that need to be considered [40]. The Iranian national cancer registry was established under the supervision of the Tehran University of Medical Sciences in 1984 and has been publishing data since 1999 [41]. The coverage of the registration system in Islamic Republic of Iran has been improving in recent years [41]. According to the Iranian Ministry of Health, cancer registration rates have risen from 18% in 1999 to 80% in 2005 [38]. This could explain the upward trend in the incidence of all cancers including skin cancer in the country. Studies of cancer rates in the Islamic Republic of Iran should address the effect of such improvements in the cancer registry on observed trends. Although studies such as ours do not aim to investigate the reasons for such changes over time, there is a need to investigate the contribution of different factors on the observed increases in incidence of skin cancer in the Islamic Republic of Iran in future studies.
References
- Boyle P et al. Cancer of the skin: a forgotten problem in Europe. Annals of Oncology, 2004, 15:5–6.
- Boyle P, Levin B. World cancer report 2008. Lyon, France, International Agency for Research on Cancer, 2008.
- Cancer facts and figures. Atlanta, Georgia, American Cancer Society, 2004.
- Leboit PE et al., eds. IARC/World Health Organization classification of tumours. Pathology and genetics of skin tumours. Lyon, France, International Agency for Research on Cancer, 2006.
- Koh D et al. Basal cell carcinoma, squamous cell carcinoma and melanoma of the skin: analysis of the Singapore Cancer Registry data 1968–97. British Journal of Dermatology, 2003, 148:1161–1166.
- Scotto J, Kopf AW, Urbach FJS. Non-melanoma skin cancer among Caucasians in four areas of the United States. Cancer, 1974, 34:1333–1338.
- Koh D et al. Basal cell carcinoma, squamous cell carcinoma and melanoma of the skin: analysis of the Singapore Cancer Registry data 1968–97. British Journal of Dermatology, 2003, 148:1161–1166.
- Almahroos M, Kurban A. Ultraviolet carcinogenesis in nonmelanoma skin cancer. I: incidence rates in relation to geographic locations and in migrant populations. Skinmed, 2004, 1:29–36.
- Nunes DH, et al. Incidencia do carcinoma de celulas escamosas da pele na cidade de Tubarao (SC)–Brasil nos anos de 2000, 2003 e 2006. [Incidence of squamous cell carcinoma of the skin in the city of Tubarao (SC)–Brazil in the years 2000, 2003, and 2006]. Anais Brasileiros de Dermatologia, 2009, 84:482–488.
- Suzuki T et al. Doses of solar ultraviolet radiation correlate with skin cancer rates in Japan. Kobe Journal of Medical Sciences, 1996, 42:375–388.
- Tatalovich Z et al. The objective assessment of lifetime cumulative ultraviolet exposure for determining melanoma risk. Journal of Photochemistry and Photobiology. B, Biology, 2006, 85:198–204.
- Abarca JF, Casiccia CC. Skin cancer and ultraviolet-B radiation under the Antarctic ozone hole: southern Chile, 1987–2000. Photodermatology, Photoimmunology and Photomedicine, 2002, 18:294–302.
- Le Marchand L et al. Sun exposure, diet, and melanoma in Hawaii Caucasians. American Journal of Epidemiology, 2006, 164:232–245.
- Ibiebele TI et al. Dietary pattern in association with squamous cell carcinoma of the skin: a prospective study. American Journal of Clinical Nutrition, 2007, 85:1401–1408.
- Schauberger G, Keck G, Cabaj A. Trend analysis of solar ultraviolet exposure of the Austrian population caused by holiday patterns since 1969. Photodermatology, Photoimmunology and Photomedicine, 1992, 9:72–77.
- Habibi A. Epidemiological aspects of cancer in Iran. International Surgery, 1985, 70:105–108.
- Mousavi SM et al. Cancer incidence and mortality in Iran. Annals of Oncology, 2009, 20:556–563.
- Noorbala MT, Kafaie P. Analysis of 15 years of skin cancer in central Iran (Yazd). Dermatology Online Journal, 2007, 13(4):1.
- Marjani A, Kabir MJ. Male skin cancer incidence in Golestan province, Iran. Journal of the Pakistan Medical Association, 2009, 59:287–289.
- Zamanian A, Farshchian M, Meheralian A. A 10-year study of squamous cell carcinoma in Hamedan in the west of Iran (1993–2002). International Journal of Dermatology, 2006, 45:37–39.
- Fritz A et al., eds. International Classification of Disease for Oncology, 3rd ed. Geneva, World Health Organization, 2000.
- Statistical Center of Iran [online database] (http://www.amar.org.ir/Default.aspx, accessed 11 November 2012).
- WHO Statistical Information System (WHOSIS). World Health Organization [online database] (http://www.who.int/whosis/indicators/en/, accessed 11 November 2012).
- Italian cancer figures, report 2009. Cancer trend (1998–2005). Epidemiologia e Prevenzione, 2009, 33(4–5 Suppl. 1):1–168.
- De Vries E et al. Predictions of skin cancer incidence in the Netherlands up to 2015. British Journal of Dermatology, 2005, 152:481–488.
- Hughes JR et al. Increase in non-melanoma skin cancer—the King’s College Hospital experience (1970–92). Clinical and Experimental Dermatology, 1995, 20:304–307.
- Stang A et al. Time trend analysis of the skin melanoma incidence of Finland from 1953 through 2003 including 16,414 cases. International Journal of Cancer, 2006, 119:380–384.
- Zeb A, Rasool A, Nasreen S. Cancer incidence in the districts of Dir (North West Frontier Province), Pakistan: a preliminary study. Journal of the Chinese Medical Association, 2008, 71:62–65.
- Leiter U, Garbe C. Epidemiology of melanoma and nonmelanoma skin cancer—the role of sunlight. Advances in Experimental Medicine and Biology, 2008, 624:89–103.
- Bulliard JL, Panizzon RG, Levi F. Prevention du metanome en Suisse: ou en sommes-nous? [Melanoma prevention in Switzerland: where do we stand?]. Revue Medicale Suisse, 2006, 2:1122–1125.
- Ibiebele TI et al. Dietary pattern in association with squamous cell carcinoma of the skin: a prospective study. American Journal of Clinical Nutrition, 2007, 85(5):1401–1408.
- Moan J, Dahlback A. The relationship between skin cancers, solar radiation and ozone depletion. British Journal of Cancer, 1992, 65(6):916–921.
- Montazeri A et al. Cancer patient education in Iran: a descriptive study. Support Care Cancer, 2002, 2010;169–173.
- Khosravi A, Najafi F, Rahbar M. [The indicators of heath feature in Iran]. Tehran, Ministry of Health and Medical Education, 2010 [In Farsi].
- Delavari A, Alikhani S, Alaedini F. [A national profile of noncommunicable disease risk factors in the IR Iran]. Tehran, Ministry of Health and Medical Education, Deputy for Health Directory, CDC, 2005 [In Farsi].
- Gallagher RP et al. Sunlight exposure, pigmentation factors, and risk of nonmelanocytic skin cancer. II. Squamous cell carcinoma. Archives of Dermatology, 1995, 131(2):164–169.
- Zamanian A, Farshchian M, Meheralian A. A 10-year study of squamous cell carcinoma in Hamedan in the west of Iran (1993–2002). International Journal of Dermatology, 2006, 45(1):37–39.
- El Khwsky F et al. Risk factors for non-melanomatous skin cancer in Alexandria, Egypt. International Journal of Cancer, 1994, 56(3):375–378.
- Iranian Annual National Cancer Registration Report 2005–2006. Tehran, Ministry of Health and Medical Education, 2007 [In Farsi].
- Mousavi SM et al. Cancer incidence and mortality in Iran. Annals of Oncology, 2009, 20(3):556–563.
- Etemadi A et al. Cancer registry in Iran: a brief overview. Archives of Iranian Medicine, 2008, 11(5):577–580.


